There is a continued emerging evidence to suggest that the use of Supraglottic Airway Devices (SGDs) for airway management in children results in fewer perioperative airway complications when compared to tracheal intubation [1,2]. Second generation SGDs with their inbuilt gastric drainage channel and a better oropharyngeal sealing pressure provide effective controlled ventilation and minimise the chances of gastric insufflation in children [3].
LMA P (teleflex incorporated, US) a reusable device made up of silicon is considered a gold standard second generation SGD. There is a huge data showing LMA ProSeal as an effective ventilatory device in children. It has been shown to have high OSP and is thus, less likely to cause gastric insufflation [3,4]. The main disadvantage of a reusable LMA ProSeal is the risk of transmitting infections due to deposition of prions, despite washing and standard sterilisation [5]. Single use devices are preferred by paediatric anaesthesiologists to minimise the chance of transmitting infections [6].
The AAG (Ambu A/S, Ballerup) is a newer single use anatomically curved second generation SGD, launched in June 2014. The integrated gastric access channel is designed to facilitate easy placement of a gastric tube. The original preformed anatomical, soft and rounded curve of the AAG ensures rapid placement. It has thin and soft inflatable cuff which delivers high OSPs. It also has an advantage of having a shorter and wider airway tube, which may facilitate tracheal tube passage through it [7].
Seal pressure is one of the properties that determine the efficiency of a SGD, as the device with higher oropharyngeal sealing pressure offers effective ventilation at higher Peak Airway Pressure (PAP) with a greater margin of safety. A study showed that AAG provided higher OSP as compared with LMA ProSeal in anaesthetised and paralysed children but the success, number of attempts and ease of placement and fibreoptic visualisation of larynx were comparable for the two devices [8].
Therefore, this study was conducted to evaluate and compare the clinical performance of the single use AAG with that of LMA ProSeal as a ventilatory device with primary objective of comparing OSP, in children undergoing elective surgery under general anaesthesia with controlled ventilation. The secondary objectives were number of attempts taken for successful insertion of the device, time taken for achieving effective airway, ease of gastric tube placement and anatomical alignment of device with fibreoptic view of glottis.
Materials and Methods
This randomised controlled trial was conducted after obtaining approval from Institutional Ethics Committee (IEC/VMMC/SJH/Thesis/october/2018-145). The trial was registered with Clinical Trials Gov (CTRI/2019/ 04/018844). The study was conducted at Vardhman Mahavir Medical College from May 2019 to February 2020. Written informed consent was obtained from guardian/parent of all the patients.
Sample size calculation: Sample size was calculated with reference to a similar study conducted by Joshi R et al., where they observed that the mean OSP with AAG was significantly higher than that with LMA ProSeal (23.3±4.6 cmH2O vs 20.6±4.8 cmH2O, respectively, p=0.007) [8]. Taking these values as reference, the minimum required sample size with 80% power of study and 5% level of significance was 48 patients in each study group.
Inclusion criteria: This study was conducted on 100 paediatric patients in age group of 1 to 12 years, weighing 5 to 30 kg, fulfilling the criteria of ASA Physical Status I and II and undergoing elective surgical procedures.
Exclusion criteria: Patients with anticipated difficult airway, cervical spine pathology, anticipated surgery time greater than 4 hours, high risk of aspiration and preoperative respiratory tract infection were excluded from the study.
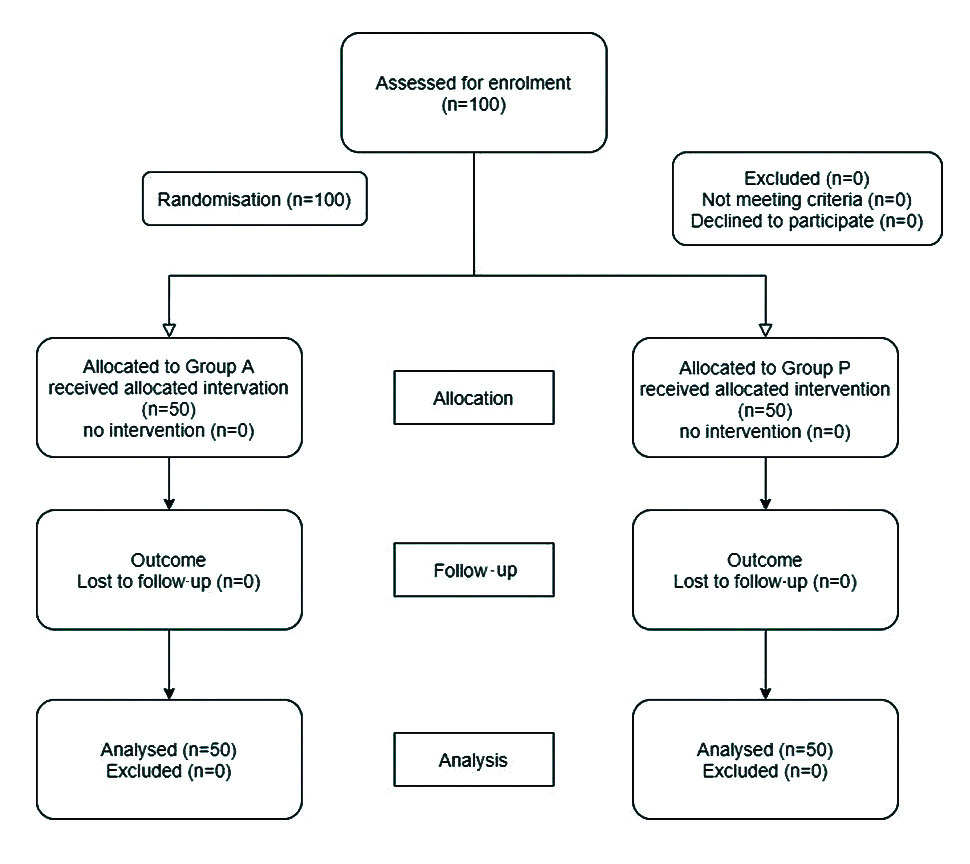
Patients were randomly allocated into two groups using closed sealed envelope method:
Group A-AAG was inserted (n=50) and Group P-LMA ProSeal was inserted (n=50) [Table/Fig-1].
Study Procedure
All children were made to fast as per ASA guidelines and received premedication with syrup pedichloryl 50 mg/kg body weight orally two hours before surgery to allay separation anxiety from parents. Once sedated, children were taken to the operation theatre. Standard monitors for non-invasive blood pressure, electrocardiography and pulse oximetry (SpO2) were attached and baseline vitals were recorded.
Anaesthesia was induced with inhalation of sevoflurane up to 8% in oxygen and nitrous oxide (1:1) or thiopentone. Intravenous line was established with 24/22 guage cannula. Intravenous fentanyl 2 μ/kg body weight was given. After checking ventilation, vecuronium bromide 0.1 mg/kg body weight was given intravenously to achieve neuromuscular blockade. Face mask ventilation was done for 3 minutes to allow full jaw relaxation and then appropriate SGD was inserted as per group allocation.
The principal investigator who inserted the device had an experience of inserting each of the devices at least 30 times successfully in paediatric patients before starting the study. The observer, assessing the postoperative pharyngolaryngeal morbidity was blinded to the allocation of the group and the airway device that was used.
In group A, a lubricated AAG of appropriate size was inserted as per manufacturer’s instructions with the patients head and neck in sniffing position [6]. It was held with three fingers placed on the flat part of the bite absorption area and the thumb on the vertical line on the bite absorption area, which was oriented anteriorly toward the patient’s nose. Other hand was placed under the patient’s head. Then the tip of the cuff was inserted pressing upwards against the hard palate and cuff was flattened against it. AAG was advanced into the hypopharynx in a smooth motion until a definite resistance was felt. Cuff of the device was inflated with air to 60 cm of water using cuff pressure gauge.
In group P, a lubricated LMA ProSeal of appropriate size was inserted with the patient’s head and neck in sniffing position using introducer technique as per manufacturer’s instructions. Introducer was removed, cuff was inflated with air to 60 cm of water using cuff pressure gauge [9].
Airway tube of the device was connected to closed circuit. Effective airway was said to be present if there was bilateral symmetrical chest expansion, square wave form tracing on capnograph, lack of gastric insufflation and no audible significant leak during gentle manual ventilation.
The ease and time of insertion of the device was noted and scored as:
Score 1- easy-insertion successful at first attempt without any tactile resistance
Score 2- slightly difficult-insertion successful at first attempt with tactile resistance
Score 3- difficult-insertion successful at second attempt
Score 4- very difficult-insertion successful at third attempt
Score 5- impossible-insertion failed at third attempt
Airway manipulations such as jaw thrust, head and neck flexion or extension, chin lift, pushing in or pulling out the device for achieving effective airway was noted.
If effective airway was present, a lubricated gastric catheter of recommended size was passed through the drain tube into the stomach. The correct placement of the gastric tube was confirmed by epigastric auscultation. Achieving effective airway and successful insertion of gastric tube was considered as successful insertion of device. In the event of failure to insert the device, or inability to achieve effective airway or pass the gastric catheter into the stomach, the device was removed and was counted as a failed attempt. Three failed attempts of insertion were considered as failure of device. Any change in the size of the device on the subsequent attempt was noted. In case of failure of device, airway was secured with endotracheal intubation. If SpO2 fell <95% at any time during insertion of device, the attempt was terminated and the patient was mask ventilated with 100% oxygen.
The OSP was determined by closing the Adjustable Pressure-Limiting (APL) valve with a fresh gas flow of 3 L/min and observing the airway pressure at which equilibrium was attained (pressure not allowed to exceed 30 cm of water) in the aneroid manometer and an audible leak was auscultated in the neck with stethoscope placed just beside the thyroid cartilage [10]. OSP was measured within 5 and 30 minutes postdevice insertion after checking that the intracuff pressure was 60 cm of water. Any audible air leak at mouth was noted during leak pressure testing.
A flexible fiberoptic bronchoscope was introduced into the airway tube and its tip positioned 1 cm proximal to the end of the airway tube to view placement of the device with respect to the larynx, and the view obtained was scored as [11]:
Score 4: full view of vocal cords
Score 3: part of vocal cords and posterior surface of epiglottis seen
Score 2: part of vocal cords and anterior surface of epiglottis seen
Score 1: vocal cords not visible
Patient was ventilated on volume controlled mode at tidal volume of 8 mL/kg body weight, respiratory rate of 16-24/minute using closed circle breathing system with soda lime at flow rate of 3 L/minute, maintaining normocarbia. Anaesthesia was maintained with sevoflurane (1 minimum alveolar concentration) in a mixture of 50% oxygen and 50% nitrous oxide.
Difference in OSP and PAP was calculated at 5 and 30 minutes postdevice insertion. At the end of surgery, 100% oxygen was given and residual neuromuscular blockade was reversed with intravenous neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg. The gastric catheter was attached to suction and gastric contents suctioned out. The device was removed when patient was awake with reflexes intact and any blood stains on the device were noted. Postoperative pharyngolaryngeal morbidity was evaluated by interviewing the patient at one hour and four hours and any problems encountered such as sore throat, dysphagia and hoarseness of voice were noted.
Statistical Analysis
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean±SD and median. Normality of data was tested by Kolmogorov-Smirnov test. The normality was rejected and non-parametric tests were used.
Statistical tests were applied as follows:
Quantitative variables were compared using Independent t-test/Mann-Whitney Test (when the data sets were not normally distributed) between the two groups.
Qualitative variables were correlated using Chi-Square test/Fisher’s-Exact test.
A p-value of <0.05 was considered statistically significant. The data was entered in MS Excel spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
Results
The demographic profile of patients in both the groups was similar with regard to age (years) (p-value=0.976), sex (p-value=0.834), weight (kg) (p-value=0.49), height (cm) (p-value=0.748), BMI (p-value=0.393) and duration of surgery (p-value=0.506) [Table/Fig-2].
Comparison of demographic profile of patients in group A vs group P.
| Variables | Group A (n=50) | Group P (n=50) | p-value |
|---|
| Mean age (years) | 6.23±3.53 | 6.4±3.51 | 0.809*** |
| Age distribution (years) n (%) |
| 1-5 | 22 (44) | 21 (42) | 0.976* |
| 6-10 | 20 (40) | 21 (42) |
| >10 | 8 (16) | 8 (16) |
| Weight (kg) median (IQR) | 17.5 (11-25.25) | 19.5 (12-26) | 0.49** |
| Height (cm) mean±SD | 112±21.82 | 114.32±21.62 | 0.748*** |
| Sex n (%) |
| Male | 32 (64) | 33 (66) | 0.834* |
| Female | 18 (36) | 17 (34) |
| BMI kg/m2 (mean±SD) | 14.1±1.41 | 14.32±1.09 | 0.393*** |
| Duration of surgery (hours) median (IQR) | 1.5 (1.128-2) | 1.75 (1-2) | 0.506** |
| Size of device n (%) |
| 1.5 | 8 (16) | 7 (14) | 0.831* |
| 2 | 22 (44) | 20 (40) |
| 2.5 | 20 (40) | 23 (46) |
*chi-square test; **mann-whitney test; ***t-test
p-value less than 0.05 considered significant
The median (IQR) OSP within 5 minutes of insertion was 22 (21-23) cm of water in group A and 21 (20-22) cm of water in group P. The difference was statistically significant (p-value <0.0001). At 30 minutes after insertion of device it was 23 (22-24) cm of water in group A and 21 (20-22) cm of water in group P (p-value 0.0001) [Table/Fig-3].
Comparison of clinical performance in group A vs group P.
| Variables | Group A | Group P | p-value |
|---|
| OSP (cm of water) {median(IQR)} |
| 5 minutes | 22 (21-23) | 21 (20-22) | <0.001* |
| 30 minutes | 23 (22-24) | 21 (20-22) | 0.0001* |
| OSP-PAP (cm of water) {median(IQR)} |
| 5 minutes | 9.5 (7.75-11) | 8 (6-9) | 0.005* |
| 30 minutes | 10 (9-12) | 9 (7.75-10) | 0.035* |
| No. of attempts for successful ventilation |
| First attempt | 50 (100%) | 50 (100%) | |
| Time taken for successful ventilation (seconds) median (IQR) | 18 (17-19) | 19 (18-20) | 0.0005* |
| Ease of insertion of device n (%) |
| Easy | 47 (94%) | 46 (92%) | 1.00** |
| Slightly difficult | 3 (6%) | 4 (8%) |
| Ease of insertion of gastric tube n (%) |
| First attempt | 50 (100%) | 49 (98%) | 1.00** |
| Second attempt | 0% | 1 (2%) |
| Fibreoptic score n (%) |
| 3 | 13 (26%) | 10 (20%) | 0.476*** |
| 4 | 37 (74%) | 40 (80%) |
*Mann-Whitney test; **Fisher-Exact test; ***Chi-Square test
p-value less than 0.05 considered significant
There was no statistically significant difference between group A and group P with regard to median PAP at 5 and 30 minutes postdevice insertion. The median (IQR) OSP-PAP at 5 minutes was 9.5 (7.75-11) cm of water in group A and 8 (6-9) cm of water in group P. The difference was statistically significant, (p-value=0.005). The median (IQR) OSP-PAP at 30 minutes was 10 (9-12) cm of water in group A and 9 (7.75-10) cm of water in group P. The difference was statistically significant, (p-value=0.035) .
In both groups, there was a 100% success rate at insertion in first attempt [Table/Fig-3]. In group A, the median (IQR) time for achieving effective airway was 18 (17-19) seconds and 19 (19-20) seconds in group P. The difference was statistically significant, (p-value=0.0005) [Table/Fig-3].
Insertion of device was easy in 94% patients in group A and in 92% patients in group P. Insertion was slightly difficult in 6% patients in group A and in 8% patients in group P (p-value=1.000). Manipulation (jaw thrust) was required in 3 (6.00%) patients in group A and in 4 (8.00%) patients in group P to insert the device (p-value=1.000). Ease of insertion of gastric tube was easy (score1) in 100% patients in group A and 98% patients in group P [Table/Fig-3].
Full view of the vocal cords (grade 4 view) was seen in 37 (74%) patients in group A and 40 (80%) patients in group P. A grade 3 view was observed in 13 (26%) patients in group A and 10 (20%) patients in group P (p-value=0.476) [Table/Fig-3].
No intraoperative and postoperative adverse events such as desaturation (SpO2<92%), aspiration or regurgitation, bronchospasm, laryngospasm or airway obstruction were noted in any group. No patient had visible trauma to lip, tongue, teeth and oral tissues as well as no blood staining on the device was found in any groups.
Sore throat was observed in 4 (8%) patients in group A and in 4 (8%) patients in group P. However, it resolved in all patients within 4 hours. Difficulty in swallowing was observed in 2 (4%) group A and in 2 (4%) group P.
Discussion
In this randomised controlled trial, the efficacy of AAG, new second generation, single use SGD was compared with LMA ProSeal, a multiple use second generation SGD in paediatric patients undergoing elective surgery with respect to OSP, ease and time taken for insertion, number of attempts taken for successful insertion, ease of gastric tube placement, anatomical alignment to glottic opening, and perioperative adverse events.
Joshi R et al., compared the performance of AAG with LMA ProSeal in 94 children, aged between 6 months to 12 years, undergoing elective surgical procedures [8]. They found that mean OSP with AAG was significantly higher than that of LMA ProSeal (23.3±4.6 cmH2O vs 20.6±4.8 cmH2O, p=0.007, respectively). They concluded that AAG could be a useful disposable alternative to LMA ProSeal for securing airway in children. In this study the median OSP within 5 minutes of insertion of device (cm of H2O) was higher in group A 22 (21-23) as compared to that in group P 21 (20-22) and the difference was statistically significant.
Jagannathan N et al., compared AAG and LMA Supreme in 100 infants and children for airway maintenance during mechanical ventilation [12]. The primary outcome were initial and 10 minutes airway leak pressure. The initial OSP of both devices was lower than that at 10 minutes postdevice insertion and comparable in the two groups (AAG vs LMA Supreme, median initial: 19 vs 18 cmH2O, p=0.4; and at 10 minutes: 22 vs 20 cmH2O, p=0.08, respectively). They concluded AAG may be a useful alternative to the LMA Supreme in children. Their results concur with the results in this study that AAG provides better OSP as compared to other second generation SGDs.
Higher OSP of AAG could be due to its preformed anatomical curve and larger sized cuff which probably helps in better sealing with the glottis structures. Lower OSP with LMA ProSeal in children could be due to the absence of dorsal cuff in LMA ProSeal of size 1.5, 2 and 2.5 used in children. This implies that AAG will be superior to LMA ProSeal in children who need to be ventilated at high airway pressures such as those who are obese, or have restrictive or obstructive respiratory disease and those undergoing laproscopic procedures with pneumoperitoneum.
There was no significant difference between the groups with respect to number of attempts taken for successful insertion of the device. First attempt success rate of insertion and overall success rate of insertion was 100% with both devices. A success rate of insertion with either device has been reported to be 96-100% in various studies [13-15]. The results of this study are concurrent with them. AAG has a preformed curve to follow the anatomy of human airway, and a soft rounded tip that allows easy insertion. Introducer tool of the LMA ProSeal also aids in its placement. Thus, both AAG and LMA ProSeal are comparable in success rate of insertion in this study.
Time taken for achieving effective airway was significantly less with AAG as compared to that with LMA ProSeal (p=0.0005). Difference of one second is clinically irrelevant although statistically significant. The time of achieving effective airway was more with LMA ProSeal as compared to AAG probably because of the additional time taken to remove the introducer of LMA ProSeal. Insertion of device was easy i.e., no tactile resistance was encountered during insertion of the device (score1) in 94% patients in group A and in 92% patients in group P [Table/Fig-2]. There was statistically insignificant (p-value=1.000) difference in the number of manipulations required while inserting both the devices. Jaw thrust was required in 4 (8%) patients in group P to facilitate insertion of the device as compared to 3 (6%) patients in group A. Nalini KB et al., did the comparison of three insertion techniques of ProSeal LMA [16]. Study showed that none of the patients required manipulation in the group.
The alignment of AAG with glottic opening was comparable to that of LMA ProSeal (p-value=0.476). Fiberoptic bronchoscopic view grade 4 (full view of the vocal cords) was seen in 37 (74%) patients in the group A, as compared to 40 (80%) patients in group P. Grade 3 view (partial view of vocal cords with posterior surface of epiglottis) was observed in 13 (26%) patients in group A and 10 (20%) patients in group P [Table/Fig-3]. Similarly a study by Jagannathan N et al., comparing AAG with LMA Supreme in 100 children found full view of vocal cords (grade 4 view) in 48% of the patients, partial view of vocal cords (grade 3 view) without downfolding of epiglottis in 26% patients with AAG [12].
Gasteiger L et al., conducted a randomised trial comparing LMA ProSeal vs. I-gel using the size 2 mask in 51 children aged 1.5-6 years weighing 10-25 kg. Fiberoptic position of the airway tube for the LMA ProSeal and the I-gel was similar, with the vocal cords visible from the distal airway tube in 94% and 96%, patients, respectively. They concluded that fiberoptic position of the airway tube was similar for both devices [17].
Grade 4 view means that both devices are suitable conduits for fibreoptic assisted intubation through them. AAG has a shorter and wider airway tube and maybe used as a direct conduit for intubation. Intubation with an appropriate size endotracheal tube through narrower airway tube of LMA ProSeal will have to be indirect with the help of a tube exchanger [18].
The median (IQR) OSP-PAP at 5 minutes was 9.5 (7.75-11) cm of water in group A and 8 (6-9) cm of water in group P. The difference was statistically significant, (p-value=0.005) which implies that AAG would be a better option to LMA ProSeal in patients with decreased thoracic compliance or in those who need to be ventilated at high PAPs.
Joshi R et al., reported that the gastric drain was significantly easier to insert in AAG compared to LMA ProSeal (p=0.01) probably due to its low friction inner surface of polyvinyl material [8]. However we found no difference in gastric tube insertion in both groups.
Sore throat was observed in 4 (8%) patients in group A and in 4 (8%) patients in group P. However, it resolved in all patients within 4 hours. Hoarseness of voice was not observed in any of the patients.
The similar low incidence of postoperative pharyngolaryngeal morbidity in both groups could be attributed to the fact that the recommendation of maintaining cuff pressure of 60 cm of water was strictly adhered to throughout the surgery. Other studies also reported few adverse effects like cough and sore throat with these devices [19-21].
Limitation(s)
Blinding was not possible and observer’s bias could not be eliminated. Secondly, sample size was calculated for comparing OSP, the primary outcome of the study therefore could be underpowered for other end points such as adverse effects. Moreover, as the study was conducted in anaesthetised and paralysed paediatric patients with normal airway, the result of this study may not be applicable to patients with difficult airway and those undergoing anaesthesia with spontaneous breathing.
Conclusion(s)
The study concludes that AAG, a single use second generation SGD is an effective ventilatory device and has a favourable profile with better oropharyngeal sealing pressure as compared to the LMA ProSeal in children undergoing elective surgery under general anaesthesia.
*chi-square test; **mann-whitney test; ***t-test
p-value less than 0.05 considered significant
*Mann-Whitney test; **Fisher-Exact test; ***Chi-Square test
p-value less than 0.05 considered significant