In the last decade, there has been a steep increase in several instances of violence against doctors and health care professionals not only in India but also in many other countries [1]. There are various factors that contribute to the violence this includes the uncertainty associated with treatments, overworked health care providers along with vulnerability of the patients and their relatives. From the various factors there is one important factor that is lack of EI among the physicians and health care professionals [2]. In 21st century, medical health care professional has to respond to both the technical aspects of disease and associated emotional aspects [3].
Emotional Intelligence (EI) is a type of social intelligence that involves the ability to monitor one’s own and others’ emotions, to discriminate among them and to use this information to guide one’s thinking and actions. Goleman has claimed that EI at times is more powerful than Intelligent Quotient (IQ) in predicting how successful one is in life [4,5]. IQ is widely used to predict career success in any field but IQ is said to predict only about 20% of career successes, which leave the remaining 80% to other factors such as EI [6,7].
EI is never taught in any educational course and is perceived that medical students will learn on themselves. In current scenario medical students and health care professions are inadequately prepared for handling the emotional component. The emotional competence is necessary for healthy medical training and practice [8]. Thus, this study was planned to evaluate the EI in medical students from different academic years.
Materials and Methods
A cross-sectional questionnaire based survey of 200 undergraduate medical students {50 in each academic year i.e., Ist year, IInd year, IIIrd year and IVth year of Bachelor of Medicine and Bachelor of Surgery (MBBS)} from medical college and tertiary care hospital in a metropolitan city. Institutional Ethics Committee permission from Rajiv Gandhi Medical College and Chhatrapati Shivaji Maharaj Hospital, Thane, Maharashtra, was taken before starting the study (RGMC/CSMH/IEC/A/06/10/2017 dated 13/10/2017). Study site was Department of Pharmacology and Psychiatry, medical college and tertiary care hospital. The study was conducted from January 2018 to February 2020.
Inclusion criteria: Students of either gender with age more than 18 years and willing to participate in the study were included.
Exclusion criteria: Students not willing to participate or did not return the questionnaire or returning incompletely filled forms were excluded from the study.
Sample size calculation: Sample size was calculated by Epi info software by {DEFF*Np(1-p)}/{(d2/Z21-α/2*(N-1)+p*(1-p)} formula. There were around 400 (N) students in medical college and tertiary care hospital. The calculations were based on the assumption that 50% (p) of the students will be having good EI at 95% confidence interval, limit of precision of 5% (d) and design effect of (DEFF) 1.0, the calculated sample size was 197 participants. Total 200 medical students were considered for the study, 50 students were selected from each of four academic years, Z21-α/2=1.96.
The validity (content and criterion) and reliability (test-retest reliability) of the questionnaire was tested. The content and face validity of the questionnaire was obtained by two psychiatrist and two teachers from field of medical education that were other than study. Test-retest reliability was estimated with a subsample of 20 students by taking two interviews seven days apart, these were also not included in the final analysis. Internal consistency reliability by Cronbach’s-alpha coefficient was 0.85 by Statistical Package for the Social Sciences (SPSS) version 23.0. Participation in the study was voluntary and students willing to give informed consent were enrolled in study.
Total 253 questionnaires were distributed, 229 were collected out of which 200 satisfying the inclusion and exclusion criteria were selected. The objectives of the study were informed to the participants and informed written consent was taken. The demographic information annexure and study questionnaire were administered and collected after 20-30 minutes.
The demographic information consisted of demographic details of the participants (age, gender, area of residence, year of education, accommodation, education and profession of parents, their understanding of EI). The students were asked to describe about EI, whether they knew it or not and its importance. EI was assessed using [Emotional quotient self-assessment checklist devised by Sterrett]. Emotional quotient self-assessment checklist consisted of 30 statements, five statements each for the areas for self-awareness, self-confidence, self-control, empathy, motivation and social-competency [9]. Each question statement was based on a 5-point Likert scale scoring from 1 to 5 (virtually never=1 to virtually always=5). The total score was sum of all 6 domain scores. The minimum and maximum scores for each domain was 5 and 25, respectively with a cut-off value for good EI of 20 in each domain, the score below which indicates need of improvement in the respective domain [9,10].
Statistical Analysis
Unpaired t-test and one-way ANOVA with Tukey post-hoc test was used to compare EI scores and its components among medical students. Pearson’s Correlation was used to see the relationship between components of EI and Multiple Linear regression was used to analyse the contribution of each component in predicting EI score. The data were represented as numbers, percentage, mean±standard deviation. The p<0.05 was considered to be statistically significant and Graphpad software version 8.0.2 for Windows, GraphPad Software, La Jolla California USA, www.graphpad.com was used for statistical analysis.
Results
In the study, 116 (58%) were female students and 84 (42%) were male students. Out of 200 students, 177 (88.5%) were from urban area of residence and 23 (11.5%) were from rural area. Out of 200 students, 135 (67.5%) were Hostel residents and 65 (32.5%) were non-Hostel residents. The age (years) in different academic years was MBBS Ist year (18.88±1.92), IInd year (19.44±1.67), IIIrd year (20.76±1.79) and IVth year (21.56±1.63). EI score in different socio-demographic parameters is given in [Table/Fig-1].
EI score in different socio-demographic parameters.
| EI score (M±SD) | p-value (unpaired t-test) |
|---|
| Female | 113.09±11.14 | Male | 105.45±10.8 | <0.001 |
| Rural | 111.45±9.8 | Urban | 108.46±10.97 | 0.005 |
| Hostel | 107.96±10.79 | Non-hostel | 110.57±09.58 | 0.023 |
| Medical parents | 113.06±10.15 | Non-medical parents | 106.57±10.76 | 0.161 |
There were 113 (56.5%) students that felt they knew about EI while 87 (43.5%) have not heard about EI. Out of 113 students that felt that they knew about EI, only 16 (8%) could describe about EI correctly. Out of 200 students, 89 (44.5%) felt EI very important, 92 (46%) felt EI is important, 19 (9.5%) felt EI is slightly important in medical profession. Out of 200 students, 185 (92.5%) desired to learn about EI while 165 (82.5%) felt there is need to have EI in medical curriculum. Out of 200, 12 students had parents from medical profession and 188 from non-medical profession.
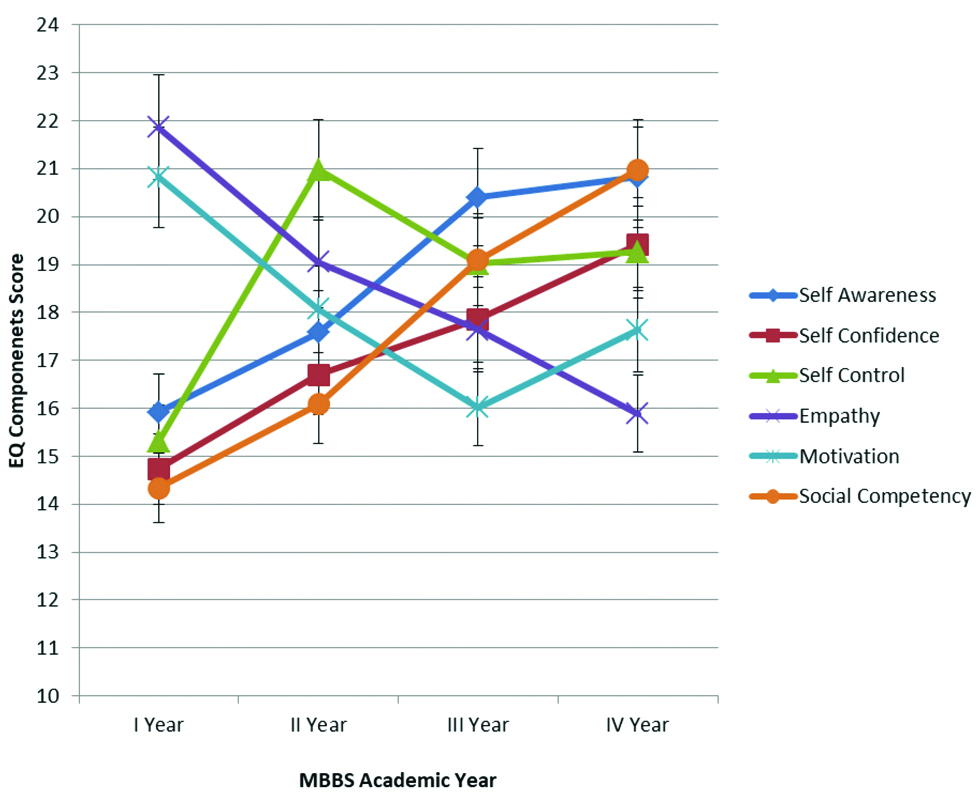
EI comparison in different academic years is given in [Table/Fig-2,3]. By post-hoc Tukey test comparison was made in groups. For self-awareness and self-control components of EI in IInd year (p<0.001), IIIrd year (p<0.001) and IVth year (p<0.001) were statistically significant as compared to Ist year, similarly IIIrd year (p<0.001) and IVth year (p<0.001) were statistically significant as compared to IInd year. For self-confidence, empathy and social competency components of EI in IInd year (p<0.001), IIIrd year (p<0.001) and IVth year (p<0.001) were statistically significant as compared to Ist year, similarly IIIrd year (p<0.001) and IVth year (p<0.001) were statistically significant as compared to IInd year while IVth year (p<0.001) was statistically significant as compared to IIIrd year. Motivation component in II year (p<0.001), IIIrd year (p<0.001) and IVth year (p<0.001) was statistically significant as compared to Ist year similarly IIIrd year (p<0.001) and IVth year (p<0.001) was statistically significant as compared to IInd year. The average of total EI score in IIIrd year (p<0.01) and IVth year (p<0.01) was statistically significant as compared to Ist year while IVth year (p<0.01) was statistically significant as compared to IInd year.
EI score comparison in different academic years.
| EI components | MBBS Academic years | p-value (ANOVA) |
|---|
| Ist year | IInd year | IIIrd year | IVth year |
|---|
| Self-awareness | 15.92±1.01 | 17.58±1.23*** | 20.4±2.17† ††,§§§ | 20.82±2.23‡‡‡,### | <0.001 |
| Self-confidence | 14.74±1.54 | 16.7±1.71*** | 17.86±1.32† ††,§§§ | 19.42±2.03‡‡‡,,###,$$$ | <0.001 |
| Self-control | 15.31±1.45 | 20.98±1.52*** | 19.02±1.65† ††,§§§ | 19.26±1.79‡‡‡,### | <0.001 |
| Empathy | 21.86±2.14 | 19.05±1.83*** | 17.64±1.72† ††,§§§ | 15.89±1.58‡‡‡,###,$$$ | <0.001 |
| Motivation | 20.82±2.15 | 18.07±1.79*** | 16.02±1.42† ††,§§§ | 17.64±1.57‡‡‡,### | <0.001 |
| Social competency | 14.34±1.35 | 16.08±1.45*** | 19.1±1.94† ††,§§§ | 20.98±2.03‡‡‡,###,$$$ | <0.001 |
| Average of total EI score | 103.45±13.73 | 108.02±12.2 | 111.74±13.86† †† | 115.02±14.79‡‡‡,### | <0.001 |
*Ist year versus IInd year, †Ist year versus IIIrd year, ‡Ist year versus IVth year, §IInd year versus IIIrd year, #IInd year versus IVth year, $IIIrd year versus IVth year
EI components in different academic years.
[Table/Fig-4] shows correlation between different components of EI correlation. Empathy component was negatively correlated with social competency and was statistically significant in all academic years. Contribution of each component in predicting the EI score is given in [Table/Fig-5]. Social competency, motivation and empathy followed by self-confidence and self-control were statistically significant components of EI in predicting EI score.
Pearson’s product moment correlation between the components of emotional intelligence correlation.
| EI components | Self-awareness | Self-confidence | Self-control | Empathy | Motivation | Social competency |
|---|
| R-value | R-value | R-value | R-value | R-value | R-value |
|---|
| Ist Year MBBS |
| Self-awareness | 1.0 | | | | | |
| Self-confidence | 0.18 | 1.0 | | | | |
| Self-control | 0.19 | 0.89 | 1.0 | | | |
| Empathy | -0.98 | -0.15 | -0.16 | 1.0 | | |
| Motivation | -0.98 | -0.13 | -0.13 | 0.99 | 1.0 | |
| Social competency | 0.98 | 0.19 | 0.20 | -0.98* | -0.98 | 1.0 |
| IInd Year MBBS |
| Self-awareness | 1.0 | | | | | |
| Self-confidence | 0.17 | 1.0 | | | | |
| Self-control | 0.17 | 0.92 | 1.0 | | | |
| Empathy | -0.87 | -0.28* | -0.25* | 1.0 | | |
| Motivation | -0.89 | -0.10* | -0.10* | 0.93 | 1.0 | |
| Social competency | 0.88 | 0.19 | 0.20 | -0.96* | -0.97 | 1.0 |
| IIIrd Year MBBS |
| Self-awareness | 1.0 | | | | | |
| Self-confidence | 0.18 | 1.0 | | | | |
| Self-control | 0.17 | 0.65 | 1.0 | | | |
| Empathy | -0.88 | -0.33** | -0.07 | 1.0 | | |
| Motivation | -0.91 | -0.18 | -0.03 | 0.93 | 1.0 | |
| Social competency | 0.93 | 0.23 | 0.01 | -0.95* | -0.98 | 1.0 |
| IVth Year MBBS |
| Self-awareness | 1.0 | | | | | |
| Self-confidence | -0.05 | 1.0 | | | | |
| Self-control | -0.10 | 0.77 | 1.0 | | | |
| Empathy | -0.76 | -0.29* | -0.12 | 1.0 | | |
| Motivation | -0.85 | -0.06 | 0.09 | 0.93 | 1.0 | |
| Social competency | 0.85 | 0.15 | -0.02 | -0.95* | -0.98 | 1.0 |
Correlation strength: r>0.70=Strong; 0.30<r<0.69=Moderate; 0.01<r<0.29=Weak; *=p<0.05, **=p<0.001
Multiple linear regression to analyse the contribution of each component in predicting the emotional intelligence score.
| EI components | Unstandardised coefficients | Standardised coefficients | t | p-value | R square | F | p-value | Shapiro-Wilk |
|---|
| B | SE | β |
|---|
| Self-awareness | -1.813 | 4.070 | -1.813 | 0.4454 | 0.65 | 0.781 | 4.573 | p<0.001 | 0.2759 |
| Self-confidence | -0.1193 | 0.0494 | -0.119 | 2.415 | 0.016* | 0.739 | 3.845 |
| Self-control | 0.0879 | 0.0430 | 0.0879 | 2.041 | 0.042* | 0.959 | 24.68 |
| Empathy | 0.4252 | 0.1053 | 0.425 | 4.038 | <0.001* | 0.787 | 4.709 |
| Motivation | -0.2918 | 0.0504 | -0.291 | 5.780 | <0.001* | 0.966 | 29.70 |
| Social competency | 1.038 | 0.1008 | 1.038 | 10.29 | <0.001* | 0.781 | 4.573 |
*Significant Predictors
Discussion
With growing complexity, and multidisciplinary approach EI has become one of the key competencies of modern practice of medicine [11,12]. In present study, EI score in female medical students was statistically significant as compared to male students. Females are emotionally more mature than males, this could be the reason for EI score was more in female than male students. In present study, the overall EI score was less for both the genders thus there is need to teach and reinforce EI from the inception of undergraduate medical training. There are similar studies where female students had significantly higher levels of EI compared to male students [13-15]. Study by Papageorgiou A et al., in medical students for 5 years found female students had higher empathy scores compared to male students [16]. While study by Tavakol S et al., had increase in empathy and EI scores seen in male students as compared to female [12]. There were contrary results in other studies where there was no gender difference regarding EI [10].
The EI in present study was measured by self-assessment questionnaire checklist by Sterret. Sterrets is a standardised questionnaire used for evaluating EI and has components that match the five components of EI given by Goleman D and Mayer JD, Salovey P four branch model of EI [17].
Among the EI components, empathy decreased in present study as the academic years of education progressed. When student progress in academics there is gain in knowledge and increase in clinical exposure, due to this the empathy might have decreased with progress in academic years. There were similar studies whereas years of medical education increased, empathy significantly declined beginning from the start of clinical year and persisting till graduation [11,18]. Study by Gupta A and Nagesh L had indicated that medical student’s empathy varies with the year of curriculum, empathy being highest at the start of the medical course and declining to a low in third year [14]. As student progresses through medical curricular years, with increase in clinical knowledge it is negatively correlated with empathy levels [13,18].
In present study, empathy and motivation steadily decreased from first year to final year while self-awareness, self-confidence, self-control and social competency steadily increased from first year to final year. There was statistically significant negative correlation between empathy and social competency. In present study self-awareness, self-confidence, self-control and social competency were the four components of EI that increased showing that as student progresses in medical curriculum student has gained these four components and these are very important for medical undergraduate to practice. In medical schools, as curriculum progresses student has to do emergency duty hours, shift duties leadings to increase in workload over the course of curriculum period, thus putting an increase in stress levels and this may cause decrease in EI among medical students as possible outcome [19].
Studies have shown that higher EI was associated with lower levels of stress and better coping ability among medical students [20]. It is recommended that medical educators must include EI not only in medical syllabus but also in assessment of the students [21]. Studies have demanded that as medical student’s progress, they should be more vigorously tested during medical school admissions process, however in Indian scenario it can be difficult [22].
Training in EI is necessary to improvise the control, perception and expression of their emotions in order to provide better patient care and improve teamwork. Accreditation Council for Graduate Medical Education had concluded that competencies of EI and empathy are essential components for 21st century physicians [23]. EI can be taught sustainably to guard against declining empathy levels and is a primary factor in developing and promoting both compassion and self-compassion [24].
The Coronavirus Disease 2019 (COVID-19) pandemic is taking monumental toll on emotions of the individual’s globally [25]. Role of positive and negative emotions and their impact is crucial in current pandemic [26]. Health Care Workers (HCW) are the frontline workers of any epidemic prevention as well as control facing heavy work tasks. HCW are in dilemma of managing their own emotions, emotions of colleagues as well as patients, thus a HCW competent to handle emotions in the current crisis event becomes a necessity [27]. Medical students are the future physicians and this pandemic has highlighted that emotions management are crucial for HCW.
The Medical Council of India envisages in producing an Indian medical graduate competent to perform the roles of clinician, professional, leader, communicator, and learning throughout life. Producing a professionally competent physician demands training of students in the medical competencies as well as soft skills that include EI [28,29]. Despite growing EI importance, there is no or minimal informal training in regard to emotional competencies in India. It is high time that a formal training for medical undergraduates on EI is initiated to produce professionally competent graduates [29]. With the change in curriculum introduced by Medical Council of India, EI has been missed and needs to be inculcated in competency based curriculum. Developing emotional competence has become the need of the time for fostering professionally competent medical students to become competent future physicians. Longitudinal studies can give further insight on the individual components aspects of EI.
Limitation(s)
There were certain limitations to the study, being a questionnaire based study there are always a chance of recall bias. The study was done at a single medical college and may not reflect the views from other medical college. Study was cross-sectional study, a longitudinal study would have been a better study design.
Conclusion(s)
This study recognises gap in EI components that can serve as basis to design and develop EI programs. EI is always considered to be known by medical students and never taught. From the current study, it can be concluded that there is a need of EI training in medical curriculum. EI needs to be included in clinical teaching along with communication skills and also in case based discussions. A medical student is competent in handling emotions has become the need of hour.
*Ist year versus IInd year, †Ist year versus IIIrd year, ‡Ist year versus IVth year, §IInd year versus IIIrd year, #IInd year versus IVth year, $IIIrd year versus IVth year
Correlation strength: r>0.70=Strong; 0.30<r<0.69=Moderate; 0.01<r<0.29=Weak; *=p<0.05, **=p<0.001
*Significant Predictors