Clinical and Diagnostic Profile and Management of Inferior Vena Cava Obstruction- A Descriptive Study at a Tertiary Care Centre, Hyderabad
Syed Imamuddin1, Chamarti Venkata Arunavalli2, Parvathareddy Krishnamala Konda Reddy3, Malladi Ramakrishna Reddy4
1 Professor, Department of Cardiology, Osmania General Hospital, Hyderabad, Telangana, India.
2 Associate Professor, Department of Cardiology, Osmania General Hospital, Hyderabad, Telangana, India.
3 Professor, Department of Cardiology, Osmania General Hospital, Hyderabad, Telangana, India.
4 Resident, Department of Cardiology, Osmania General Hospital, Hyderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Chamarti Venkata Arunavalli, Flat No. 304, Sowbhagya Lakshmi Residency, Vasavi Colony, S Aroornagar, Hyderabad-500035, Telangana, India.
E-mail: cv_arunavalli@yahoo.com
Introduction
Obstruction to hepatic venous outflow is a rare disease with a potentially fatal outcome, if not recognised and managed promptly. The level of obstruction can vary, anywhere from the small hepatic venules to the entry point of the Inferior Vena Cava (IVC) into the right atrium. The original patients that Budd-Chiari described had acute hepatic vein thrombosis but this syndrome now encompasses various hepatic venous outflow blocks, of which a membrane in the IVC is the most common anatomical form of obstruction. Pure IVC obstruction is commonly seen among Asians.
Aim
To study the clinical and diagnostic profile of patients presenting with IVC obstruction and to evaluate the treatment efficacy and safety of percutaneous transluminal angioplasty.
Materials and Methods
For this prospective, descriptive study, from November 2015 to August 2019, a total of 21 patients were admitted with obstruction of hepatic venous flow. Most of the patients were young adults. Clinical features, aetiologies and coagulation profiles were studied. Ascites, pain abdomen and pedal oedema were common presentations. Diagnosis was established by clinical examination and was confirmed by ultrasound-doppler study, computed tomography and conventional angiography. Statistical analysis was done by using statistical package for social sciences IBM SPSS statistics for Windows, version 20.0. The data were expressed as percentages of study population while, continuous data were expressed as mean±standard deviation.
Results
The mean age of the population was 24.7±2.9 years, with a female preponderance. (male: female=1:2). IVC angiography was done in 15 patients. Seven of the 15 patients had diffuse narrowing of IVC. Eight patients had focal or segmental narrowing of IVC, among them seven patients underwent Percutaneous Transluminal Angioplasty (PTA) with stenting. The venous access was obtained from femoral vein. The stenoses were crossed with either guide wire or Brocken brough needle with Mullins sheath. Three patients did not need predilatation. In four patients, obstructed IVC was dilated with Inoue balloon and then self-expanding stents were placed. Success was achieved in all cases, with significant drop in the pressure gradients from 20±5 mmHg before procedure to 3±2 mmHg immediately after the procedure. After PTA, all seven patients had either total relief or decrease of symptoms and clinical signs of hepatic venous obstruction. No major complications were observed and no repeat interventions were required. The mean postprocedural follow-up was six months that showed good outcomes with good stent patency.
Conclusion
Chronic obstruction of IVC presents with abdominal pain, progressive ascites and portal hypertension in young adults, with mild abnormality of liver function tests. The IVC obstruction can be due to an obstructive membrane or segmental stenosis or diffuse narrowing of IVC. PTA with stenting can be done safely and it effectively relieves the symptoms and venous congestion and can be considered as the first line decompressive procedure in patients with IVC stenosis.
Brockenbrough needle, Hepatic vein, Inoue balloon, Percutaneous transluminal angioplasty, Stenting
Introduction
Hepatic venous outflow obstruction, also known as Budd-Chiari syndrome can be located anywhere from the small hepatic venules to the entry point of the IVC into the right atrium. There are various aetiologies causing the obstruction. By convention, hepatic veno-occlusive disease and cardiac disorders are not included in this definition [1]. The pathophysiological consequences include obstruction, which leads to sinusoidal congestion, ischemia and finally hepatocellular necrosis, fibrosis and cirrhosis [1]. IVC Obstruction (IVCO) is clinically suspected under the following circumstances: (a) simultaneous presentation of pain in the right hypochondriac region, ascites and hepatomegaly; (b) whenever severe and resistant ascites is seen with mildly deranged liver function tests in patients with liver disease symptoms and signs; (c) when a patient with prothrombotic disorder presents with liver disease manifestations; (d) when there is liver enlargement and ascites in a patient presenting with fulminant hepatic failure; (e) when there is unexplained chronic liver disease after common causes are ruled out [1].
Primary IVC obstruction is a diagnosis of exclusion of secondary causes like thrombus, extrinsic compression by thrombus, cysts etc., [1,2]. In western countries, pure hepatic vein thrombosis is most common. In Asian countries, either pure IVC or combined IVC and hepatic vein obstruction predominates. The IVC obstruction can be membranous, a short segment stenosis or diffuse narrowing [3]. To establish the diagnosis of IVCO, the initial investigations are abdominal ultrasound and doppler study of IVC and hepatic veins. Both the investigations together have a diagnostic sensitivity of 75%. Various features on doppler study include absence of flow signal in the hepatic veins, collateral formation, a spider-web appearance around the hepatic vein ostia. The presence of intrahepatic or subcapsular hepatic venous collaterals is a distinguishing feature of IVCO on Doppler study. Computed Tomography (CT) or Magnetic resonance imaging (MRI) are the second line of investigation. The gold standard of investigation is IVC and hepatic vein venography which defines the site and extent of obstruction prior to intervention [4,5].
Medical treatment consists of diuretics, therapeutic paracentesis where indicated, anticoagulation, and compressive stockings to lower limbs [6,7]. Transjugular Intrahepatic Portosystemic Shunt (TIPS) can be done when there is extensive hepatic vein obstruction. It relieves the portal pressure in both cirrhosis and IVC obstruction. But indications for TIPS are limited [8]. Surgical options include porto-caval shunt procedures, liver transplantation. Both these have high procedural risk. When there is narrowing of only a short segment of IVC or hepatic veins, it is feasible to do a percutaneous transluminal angioplasty of the affected venous segment, with or without stenting. These procedures relieve the liver congestion and decrease the portal hypertension. PTA is increasingly done presently to treat chronic IVC obstruction as it is a safe, minimally invasive and low-risk procedure with a fairly good procedural success rate, causing immediate relief of symptoms [9]. After obtaining venous access via femoral vein, the obstructed IVC segment can be crossed either by a Terumo 0.032 or in case of critical obstruction, by a brockenbrough needle-mullen sheath assembly. The dilatation is done by peripheral angioplasty balloon or Inoue balloon [9]. Usually self-expanding stents can be placed across the obstructed segment.
PTA alone is associated with recoil of the dilated segment and re-occlusion, especially in segmental stenosis. Stenting of the affected segment maintains good long term patency. The studies evaluating the use of Inoue balloon for dilatation of chronic IVC obstruction, followed by stenting are rare. This study was conducted as the authors have experienced increased incidence of patients with IVC obstruction in the specific geographical location and the patient profile and percutaneous management has never been studied at the institute. Thus, the study aimed to evaluate the clinical and diagnostic profile of patients presenting with IVC obstruction and to assess the treatment efficacy and safety of percutaneous transluminal angioplasty.
Materials and Methods
This prospective, descriptive study, was conducted between November 2015 to August 2019 upon a total of 21 patients who were admitted in Cardiology Department of Osmania General Hospital, Hyderabad with the symptoms suggestive of IVC obstruction. This study was conducted while following the Helsinki guidelines. The patient data were collected ensuring that the identities are not revealed in any manner.
Inclusion criteria: Patients presenting with progressive ascites, pain in the right hypochondrium, upper gastrointestinal bleeding and pedal oedema in younger people with minimal jaundice and little derangement of liver function, despite clinical features of cirrhosis with diagnosis of IVCO established by doppler study of IVC and hepatic veins, confirmed by CT angiogram.
Exclusion criteria: Hepatic ailments such as alcoholic liver disease, cirrhosis of liver, hepatocellular neoplasms, cysts, metastatic liver disease and viral hepatitis were excluded from the study. Cardiac diseases such as congestive heart failure, right heart failure of any cause, constrictive pericarditis were ruled out. Splenic vein thrombosis, portal vein thrombosis, extrinsic compression of IVC were excluded.
Written consent was obtained from all the patients for inclusion in the study. A diagnostic workup of the patients was done, consisting of haemogram, hepatic function tests like serum bilirubin, liver enzymes, serum proteins. Coagulation profile was studied in all patients. Ultrasound study of the abdomen was done to rule out cirrhosis and any other causes of abdominal pain and portal hypertension. All patients underwent upper GI endoscopy to rule out oesophageal varices. Initially diagnosis was established by Doppler study of the IVC and hepatic veins. The diagnosis was confirmed by CT angiogram. In the absence of contraindications, informed consent was taken from willing patients and IVC venogram by conventional angiography was done. All the patients were treated with diuretics, anticoagulation and paracentesis where indicated.
Study Procedure
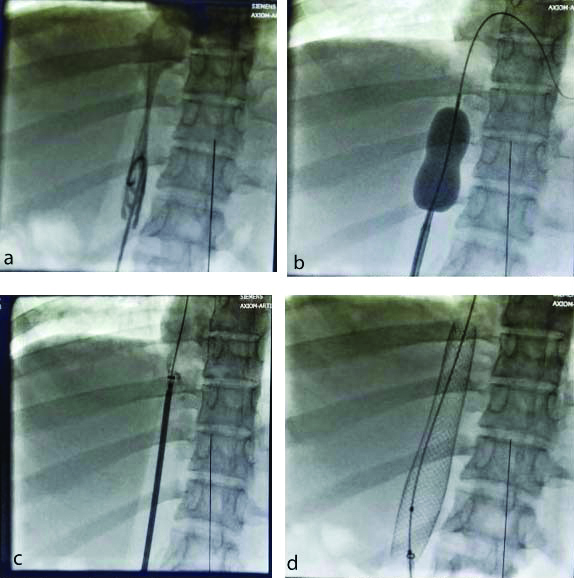
All the patients were given mild sedation in the form of oral alprazolam 0.5 mg. The patients were kept fasting overnight. The procedures were performed under local anaesthesia with xylocaine injection. The procedures were done under anticoagulation with unfractionated heparin, with Activated Partial Thromboplastin Time (APTT) levels 2 to 2.5 times the normal value. The venous access was obtained by Seldinger technique via the right femoral vein. Where the obstruction was incomplete, the lesion was crossed with 0.032″ Terumo guidewire and direct stenting was done with good result. Where the obstruction was critical, it was crossed with Brockenbrough needle with Mullins sheath, which was exchanged to steel-coiled guide wire. Septal dilator was used to dotter the lesion. Obstructed IVC was dilated with Inoue balloon. The size of the Inoue balloon used was 18 to 20 cc volume. Self-expanding wall stents were placed across the dilated segments [Table/Fig-1]. The size of stents used was 18×40 mm to 20×80 mm.
Angioplasty of IVC using inoue balloon and stenting. a) Venogram showing obstruction; b) Dilatation of IVC obstruction with Inoue balloon; c) Stent across the obstruction; d) Expanded stent across the obstruction.
Statistical Analysis
Statistical analysis was done by using IBM Statistical Package for the Social Sciences (SPSS) statistics for Windows, version 20. The data were expressed as percentages of study population; Continuous data were expressed as mean±standard deviation.
Results
A total of 21 subjects were studied. The mean age of patients was 24.7±2.9 years. There was a preponderance of female patients (male: female ratio of 7:14).
All patients had less than normal haemoglobin. Five patients had anaemia with haemoglobin less than 10 gms/dL and were given blood transfusions. Eighteen (85%) patients had deranged liver function, with mild elevation of serum bilirubin and liver enzymes [Table/Fig-2]. One female patient had history of intake of oral contraceptive pills. Twelve (57%) patients had abnormal coagulation profile in form of shortened coagulation time and Prothrombin Time (PT)/International Normalised Ratio (INR) in the lower range of standard levels and protein C deficiency in one female patient. Seventeen (79%) patients had significant oesophageal varices on upper GI Endoscopy. All patients had confirmed IVC obstruction on IVC Doppler study and CT Venogram. Eleven patients had associated hepatic vein obstruction of varying degrees in radiological studies.
Baseline characteristics and investigation profiles of the study population.
| Characteristics | Values n (%) |
|---|
| Age (Years) | 24.7±2.9 |
| Sex (M/F) | 7/14 |
| Pedal oedema | 21 (100) |
| Abdominal pain | 15 (71) |
| Ascites | 21 (100) |
| Superficial engorged veins | 17 (79) |
| Hepatomegaly | 21 (100) |
| Oesophageal varices | 17 (79) |
| Impaired LFT | 18 (85) |
| Abnormal coagulation profile | 12 (57) |
M: Male; F: Female; LFT: Liver function test
Of the 21 patients admitted, one female had subacute bacterial peritonitis and had to be managed conservatively. One male patient presented with fulminant liver failure and upper gastrointestinal bleeding and died one week after admission. Four patients were not willing to undergo IVC Venogram. Thus, 15 patients consented for angiography of the IVC. Seven patients had diffuse obstruction of the IVC and the hepatic veins. Eight patients had focal or segmental narrowing of the IVC. Among them, one patient had poor general health in the form of anaemia and repeat UGI bleeding but refused interventional procedure. Among the 15, 7 patients underwent PTA with stenting [Table/Fig-3].
Type of IVC and hepatic vein obstruction on angiography and PTA procedural details.
| Characteristics | Values n (%) |
|---|
| Angiography | 15 |
| Pure IVC obstruction | 8 (53) |
| IVC, HV diffuse disease | 7 (46) |
| PTA with stenting | 7 (46) |
| Direct stenting | 3 (20) |
| Predilatation+stenting | 4 (26.6) |
| Pre and postdilatation | 2 (13.3) |
IVC: Inferior vena cava; HV: Hepatic vein
Technical success was defined as free flow of contrast through the stented IVC segment and absence of significant gradient across the stented segment which was achieved in all cases. [Table/Fig-4]. The mean fall of gradients was from 20±5 mmHg to 3±2 mmHg in the immediate postprocedural period. The symptoms and signs were relieved after PTA in all seven patients. All the patients were given double antiplatelet therapy in form of Tab. Aspirin 150 mg per day and Tab. Clopidogrel 75 mg per day.
Poststenting inferior vena cava computed tomography angiogram.

In all patients, oral anticoagulation was started four days after the procedure, continued indefinitely, with INR value maintained at 2 to 3. No major complications were observed, and no repeat interventions were required. Short-term follow-up was for six months, once in every month. Repeat Doppler studies were done at one month, three months and six months after the procedure and showed good stent patency in all patients.
Discussion
The original patients that Budd-Chiari described had acute hepatic vein thrombosis, but this syndrome now encompasses various hepatic venous outflow blocks, of which pure IVC obstruction is more common in Asia whereas pure hepatic vein obstruction predominates in Western countries [9]. Usually, there is a male preponderance of the condition [9]. In contrast, this series of patients showed a female preponderance. Yang XL et al., performed angioplasty of membranous IVC obstruction in 40 patients, with Inoue balloon dilatation and reported procedural success of 91% (38 patients). Stenting of dilated IVC was not done. On long term follow-up of eight years, only one patient developed restenosis and underwent repeat PTA, followed by a third procedure of balloon dilatation and stenting. The Inoue balloon diameter is closer to IVC diameter and can be tailor-made based on the degree of obstruction. It allows the usage of low pressure inflations shorter inflation times and has the ability to dilate tougher membranes [10]. In the present study, there was segmental occlusion and dilatation using Inoue balloon was 100% successful.
In the study by Srinivas BC et al., patients were in the older age group (35±6.1 years) and had a male preponderance (M/F=7/5). Out of the twelve patients studied, membranous obstruction was seen in six patients i.e., 50% cases. Segmental obstruction was seen in five patients. There was no hepatic vein involvement. Out of the 12 cases, only balloon dilatation was done in six patients and six patients underwent stenting as well. All were followed-up for upto 13 years. There was only one case of restenosis [11]. In the present study, the patients were younger (24.7±2.9 years) and there was a preponderance of female patients. Principal anatomy was discrete segmental occlusion of IVC, followed by diffuse thrombotic occlusion of IVC and hepatic veins. There were no cases with membranous web. Zhang CQ et al., reported the long term effects of stent placement in IVC or hepatic veins in 115 patients [12]. In this study, the primary site of obstruction was IVC followed by combined IVC and hepatic veins. (IVC obstruction: 85 patients. hepatic vein obstruction: 13 patients, obstruction at both sites: 17 patients). Stenting was done under ultrasound guidance. Procedural success was 94% for IVC stenting (96/102) and 87% for hepatic vein stenting (26/30). A 96.7 % of IVC stents remained patent over a mean follow-up of 49 months [12].
Jagtap N et al., retrospectively analysed 88 patients with Budd-Chiari syndrome who underwent endovascular intervention. Here too the main site of stenosis was IVC 42 (47.7%), followed by hepatic veins 33 (37.5%), combined IVC and HV 13 (14.8%). IVC angioplasty alone was done in 11 subjects, IVC angioplasty with stenting in 36 patients, HV angioplasty with stenting done in 26 patients, combined HV and IVC stent performed in two subjects. Procedures were successful in 87 patients (98.86%). The stent patency rate at four years was 70.45% [13]. Procedural success was 100% in the present study but long term follow-up results are not available. Thus, endovascular management of IVC obstruction with stent placement has very good long term patency rates. All the patients showed excellent symptomatic relief and 100% stent patency on short term follow-up of six months. Thus, in IVC obstruction, PTA and stenting can be a treatment choice. The morbidity and mortality is least and the long-term patency rates are excellent.
Limitation(s)
The number of patients was less and the long term follow-up results are not yet available.
Conclusion(s)
Chronic IVC obstruction is a rare obstructive disease of hepatic venous outflow and an important treatable cause of progressive ascites and portal hypertension. PTA with stenting is a safe and effective first line decompressive treatment in patients with chronic IVC stenosis and is associated with very good long term symptomatic relief and IVC patency.
M: Male; F: Female; LFT: Liver function test
IVC: Inferior vena cava; HV: Hepatic vein
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? No
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 17, 2020
Manual Googling: Feb 10, 2020
iThenticate Software: Feb 18, 2021 (18%)
[1]. Janssen HLA, Garcia-Pagan JC, Elias E, Mentha G, Hadengue A, Valla DC, European Group for the Study of Vascular Disorders of the LiverBudd-Chiari syndrome: A review by an expert panelJ Hepatol 2003 38(3):364-71.10.1016/S0168-8278(02)00434-8 [Google Scholar] [CrossRef]
[2]. Shin N, Kim YH, Xu H, Redefining Budd-Chiari syndrome: A systematic reviewWorld J Hepatol 2016 8(16):691-702.10.4254/wjh.v8.i16.69127326316 [Google Scholar] [CrossRef] [PubMed]
[3]. Okuda K, Membranous obstruction of the inferior vena cava (obliterative hepatocavopathy, OkudaJ Gastroenterol Hepatol 2001 16(11):1179-83.10.1046/j.1440-1746.2001.02577.x11903732 [Google Scholar] [CrossRef] [PubMed]
[4]. Mahmoud AE, Mendoza A, Meshikhes AN, Olliff S, West R, Neuberger J, Clinical spectrum, investigations and treatment of Budd-Chiari syndromeQ J Med 1996 89:37-43.10.1093/oxfordjournals.qjmed.a0301358730341 [Google Scholar] [CrossRef] [PubMed]
[5]. Valla DC, Budd-Chiari syndrome/hepatic venous outflow tract obstructionHepatol Int 2018 12(Suppl 1):168-80.10.1007/s12072-017-9810-528685257 [Google Scholar] [CrossRef] [PubMed]
[6]. Menon KV, Shah V, Kamath PS, The Budd-Chiari syndromeN Engl J Med 2004 350:578-85.10.1056/NEJMra02028214762185 [Google Scholar] [CrossRef] [PubMed]
[7]. Hernández-Gea V, De Gottardi A, Leebeek FWG, Rautou PE, Salem R, Garcia-Pagan JC, Current knowledge in pathophysiology and management of Budd-Chiari syndrome and non-cirrhotic non-tumoral splanchnic vein thrombosisJ Hepatol 2019 71:175-99.10.1016/j.jhep.2019.02.01530822449 [Google Scholar] [CrossRef] [PubMed]
[8]. Parker R, Role of transjugular intrahepatic portosystemic shunt in the management of portal hypertensionClin Liver Dis 2014 18:319-34.10.1016/j.cld.2013.12.00424679497 [Google Scholar] [CrossRef] [PubMed]
[9]. Poddar P, Gurizala S, Rao S, Endovascular stenting of IVC using Brockenborough’s Needle In Budd-Chiari syndrome- A case reportIndian Heart J 2014 66(3):363-65.10.1016/j.ihj.2014.03.01424973846 [Google Scholar] [CrossRef] [PubMed]
[10]. Yang XL, Cheng TO, Chen CR, Successful treatment by percutaneous balloon angioplasty of Budd-Chiari syndrome caused by membranous obstruction of inferior vena cava: 8-year follow-up studyJ Am Coll Cardiol 1996 28(7):1720-24.10.1016/S0735-1097(96)00385-3 [Google Scholar] [CrossRef]
[11]. Srinivas BC, Dattatreya PV, Srinivasa KH, Prabhavathi, Manjunathan CN. Inferior vena cava obstruction: Long-term results of endovascular managementIndian Heart J 2012 64:162-69. [Google Scholar]
[12]. Zhang CQ, Fu LN, Xu L, Zhang GQ, Jia T, Liu JY, Long-term effect of stent placement in 115 patients with Budd-Chiari syndromeWorld J Gastroenterol 2003 9(11):2587-91.10.3748/wjg.v9.i11.258714606103 [Google Scholar] [CrossRef] [PubMed]
[13]. Jagtap N, Sharma M, Singh J, Tandan M, Rao PN, Gupta R, Budd-Chiari syndrome: Outcomes of endovascular intervention-A single-center experienceIndian J Gastroenterol 2017 36(3):209-16.10.1007/s12664-017-0760-6 [Google Scholar] [CrossRef]