SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis and osteitis) is heterogenous, rare entity with manifestations of Pustulo-Psoriatic Hyperostotic Spondyloarthritis (PPHS) and Chronic Recurrent Multifocal Osteomyelitis (CRMO). It can occur in all the age groups with unknown etiology. Hereby, author presents a case of 37-year-old female who reported with the complaint of bilateral knee pain and lower back pain. Laboratory investigations revealed elevated Erythrocyte Sedimentation Rate (ESR) and C-Reactive Protein (CRP) levels. Bone scintigraphy and Magnetic Resonance Imaging (MRI) showed bone lesions, The diagnosis of SAPHO syndrome was made. The present article highlights the role of physical therapy as a non-pharmacological treatment modality to reduce pain, the intensity of which was measured by Numeric Pain Rating Scale (NPRS). The Range Of Motion (ROM) was measured by digital inclinometer and her Quality of Life (QoL) was measured by the 36-item short form health survey (SF-36) scale. Eight weeks postprotocol showed significant improvement in pain, ROM and QOL. This suggests a positive outcome of rehabilitation in SAPHO syndrome.
Knee pain, Numeric pain rating scale, Quality of life
Case Report
A 37-year-old female patient complained of bilateral knee pain (more on left) since the past 25 days. She reported that she was apparently well two years back, when the pain started to spread gradually over the lower back and in front of the chest, which was dull in nature and accompanied by some skin lesions. She was prescribed the Non-Steroidal Anti-Inflammatory Drug (NSAID), Ibuprofen 200 mg, three times a day along with a Proton Pump Inhibitor (PPI) for a period of three months by a neurologist for an inflammatory joint pain. She was advised to undergo blood tests, bone scan and X-ray. Following treatment, the pain subsided and she did not consult any physician. However, for the past one month she was not able to carry out her day-to-day activities and the intensity of pain increased. She was non-responsive to medications or icing. Since the pain did not subside, she came to the Outpatient Department of Physiotherapy. She grimaced when she entered the department with antalgic gait and scout posture. She was a non-smoker, non-alcoholic with mesomorphic built, unmarried and nulliparous.
On examination, her blood pressure and breathing pattern were within normal limits. Informed consent was taken from the patient. Subjective finding revealed a slightly raised temperature and swelling on her medial compartment of left knee with grade 3 tenderness, especially after riding a bicycle and NPRS was 7/10. There was also redness in her palms with peeling skin, which was absent when she first visited her neurologist for which she had been referred to a dermatologist, who diagnosed it as erythematous pustules [Table/Fig-1]. Tone was normal and the patient was able to perform active ROM exercises with little pain over the medial aspect of left knee. Resisted isometric contraction was painful during knee flexion. There was no functional tightness, contracture or deformity. The patient was instructed to sit in a flexion posture of spine with hips at 90°, keeping the ankle in neutral position, active knee ROM was measured by inclinometer. The 36-item short form health survey (SF-36) form was filled by asking the difficulties in day-to-day activities.
Erythematous pustules on the palm of the hands.

The patient had not undergone any immunochemistry, but the blood levels showed raised ESR (30 mm/h, with normal range 0-15 mm/h and CRP levels (1.06 mg/dL, of normal range <0.80 mg/dL).
Magnetic resonance imaging (MRI) showed, marrow changes on the iliac side of the bilateral sacroiliac (SI) joints, chronic sacroilitis and tiny lesions in the right iliac bone. There appeared to be osteoid osteoma and perineural cyst along the right SI neural foramen.
X-ray of the knees suggested minimal fluid in the left knee joint, adjacent to the lateral patellar retinaculum, along with reduced patellofemoral joint space [Table/Fig-2,3].
Anteroposterior (AP) view of knee X-ray.

Lateral view of knee X-ray.

Based on the above findings, the following diagnosis were made: Paget’s disease (genetic predisposition with increased bone turnover, recurrent fractures and deformities, with elevated level of alkaline phosphatase, and radiographs showing the characteristic of mosaic pattern, both osteolysis and osteosclerosis) and Sweet’s syndrome (characterised by neutrophilic dermatosis with raised inflammatory markers that can be accompanied by aching joints), with the involvement of clavicle. Tietze’s syndrome (swollen costal cartilages, mostly in adults, rare in children) and avascular necrosis of the clavicular epiphysis were also considered.
Taking into consideration the joint ache with the skin pustules, as observed by the neurologist, the patient was advised to undergo bone scintigraphy. The bone scintigraphy investigation showed diffuse uptake of tracer throughout the skeleton, as well as evidence of increased uptake in the bilateral costochondral joints. However, there was no increase in tracer uptake in the joints, which rules out the possibility of bilateral symmetrical polyarthritis. The scan features were also suggestive of osteomalacia with bilateral costochondritis, marked osteosclerosis and hypertrophic osteitis on the left arm [Table/Fig-4,5].
So, the final diagnosis of SAPHO syndrome was made based on the criteria mentioned in [Table/Fig-6] [1].
Diagnostic criteria proposed by Kahn for SAPHO syndrome diagnosis [1].
| Chronic recurrent multifocal sterile and axial osteomyelitis, with or without dermatosis |
| Acute, subacute, or chronic arthritis associated with palmoplantar pustulosis, pustulous psoriasis, or severe acne |
| Any sterile osteitis associated with palmoplantar pustulosis, pustulous psoriasis, or severe acne |
Rehabilitation was added as a non-pharmacological treatment. This included hot fermentation, using commercially available hydrocollator packs over the knee and lower back. Surface application of hot pads help in pain reduction in chronic cases. Temperature of the hydrocollator unit was set at 70°C and 6-8 layers of a towel was used to diminish the direct heat. It was given for 20 minutes [2].
Transcutaneous Electrical Nerve Stimulation (TENS) was carried out, using a pulse width of 250 microseconds; internal frequency of 100 Hertz with a burst frequency of 3 Hertz; intensity: until unpleasant but not painful. The electrodes were placed 10 cm above the knee at L4 dermatome [3].
The aquatic program was given twice a week for eight weeks. The total number of sessions were 16, with the duration of each session being 60 minutes. The water temperature was maintained at approximately 32°C (89°F), with a depth of 1.2 m [Table/Fig-7] [4].
Aquatic exercise protocols.
| 1st week to 2nd week | Walking forward, side-to-side, and backward (3 min);-Patellar mobilisation (2 min);-Passive stretching of particular muscles including quadriceps, gluteus, adductors, and abductors of the hip, triceps surae, and hamstrings (5 min);-Isometric and dynamic exercises of quadriceps, gluteus, adductors, and abductors of the hip, triceps surae, and hamstrings (5 min);-Balance exercises such as step-up, side, and down (5 min);-Proprioceptive exercises associated with water board (5 min);-Extension exercises associated with board in supine position (5 min);-Aerobic exercise in stationary running (20 min);-Manipulation on knee joints (5 min). |
| 3rd week to 4th week | Walking in front, side-to-side, and backward with TheraBand (3 min);-Patellar mobilisation (2 min);-self-stretching of the leg muscles: quadriceps, gluteus, adductors, and abductors of the hip, triceps surae, and hamstrings (5 min);-Isometric and dynamic exercises with TheraBand for quadriceps, gluteus, adductors, and abductors of the hip, triceps surae, and hamstrings (5 min);-Balance exercises including step-up, side, and down with TheraBand (5 min);-Proprioceptive exercises with water board with eyes closed (5 min);-Extension exercises with board in prone lying-swimming leg (5 min). |
| 5th to 8th week | Walking forward, side-to-side, and backward with TheraBand (3 min);-Patellar mobilisation (2 min);-self stretching of the leg muscles: quadriceps, gluteus, adductors, and abductors of the hip, triceps surae, and hamstrings (5 min);-Isometric and dynamic exercises with TheraBand for quadriceps, gluteus, adductors, and abductors of the hip, triceps surae, and hamstrings (5 min);-Balance exercises with step: kicks and squats (5 min);-Proprioceptive exercises with spaghetti (5 min);-Extension exercises with the board in supine and prone lying (5 min);-Aerobic exercise with deep-water running (20 min);-Manipulation on quadriceps and triceps surae (5 min). |
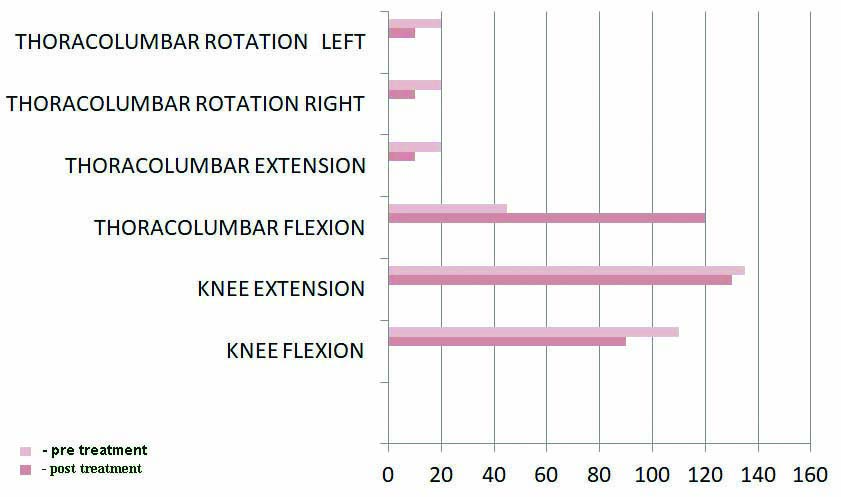
The effect of physical therapy and electrotherapy in patients with SAPHO syndrome were found to be effective in reducing pain from 7 to 3 on NPRS of moderate reliability ICC-0.67 [5] and improving QOL {36-item short form health survey (SF-36) scale} from 36 to 70 with high internal consistency of 0.88 to 0.89 [6], and ROM via inclinometer of high inter and intra-rater reliability of >0.99 and >0.98, respectively [Table/Fig-8,9] [7].
Pain and Quality of Life (QoL) measurements.
| Parameters | Pre-treatment | Post-treatment |
|---|
| PAIN | 7 | 3 |
| Quality of Life | 36 | 70 |
Range of motion improvement on various joints pre and post-treatment.
Discussion
‘SAPHO syndrome’ constitutes an array of heterogeneous conditions. However, two entities are considered among the predominant manifestations- Pustulo-Psoriatic Hyperostotic Spondyloarthritis (PPHS) and Chronic Recurrent Multifocal Osteomyelitis (CRMO). PPHS, seen in young adults, is characterised by the presence of dermatological manifestations which are usually associated with osteoarticular involvement of the Sternoclavicular Joint (SCJ). CRMO, seen in children and adolescents, involves osteoarticular involvement of the anterior chest wall with or without other axial involvement [8].
Apart from pharmacological studies, no study has been conducted till date on the management of SAPHO syndrome by means of physiotherapy. However, there is evidence to support the favourable effects of heat, including the reduction of pain and improvement of the movement breadth that is providing local body relaxation in chronic SAPHO syndrome patients [9].
Similar effects were seen by application of TENS for treating chronic shoulder pain and other major inflammatory and degenerative conditions in different parts of the body [10].
Study showed the effects of aquatic exercise on pain because of fluid mechanics. The effect of buoyancy reduced pain during exercise as the depth of immersion is directly related to the percentage weight bearing. The hydrostatic pressure compresses the tissues, which in combination with circulatory changes that occur with immersion, reduces swelling and promotes greater movement to reduce joint and soft-tissue stiffness, which in turn improves pain complaints [11].
Conclusion(s)
The present report described a rare case of SAPHO syndrome with skin and musculoskeletal involvement. The condition has been successfully treated with physiotherapy interventions. This indicates that early and effective rehabilitation of SAPHO syndrome patients is vital for a positive outlook.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 02, 2020
Manual Googling: Jan 06, 2021
iThenticate Software: Feb 01, 2021 (15%)
[1]. Kahn MF, Khan MA, The SAPHO syndromeBailliere’s clinical rheumatology 1994 8(2):333-62.10.1016/S0950-3579(94)80022-7 [Google Scholar] [CrossRef]
[2]. Prentice WE, Therapeutic Modalities for Physical Therapists 2002 2nd EdNew York [Google Scholar]
[3]. Beckwée D, De Hertogh W, Lievens P, Bautmans I, Vaes P, Effect of TENS on pain in relation to central sensitization in patients with osteoarthritis of the knee: Study protocol of a randomized controlled trialTrials 2012 13(1):01-07.10.1186/1745-6215-13-2122353582 [Google Scholar] [CrossRef] [PubMed]
[4]. Taglietti M, Facci LM, Trelha CS, de Melo FC, Effectiveness of aquatic exercises compared to patient-education on health status in individuals with knee osteoarthritis: A randomized controlled trialClinical Rehabilitation 2018 32(6):766-76.10.1177/026921551775424029417831 [Google Scholar] [CrossRef] [PubMed]
[5]. Young IA, Dunning J, Butts R, Mourad F, Cleland JA, Reliability, construct validity, and responsiveness of the neck disability index and numeric pain rating scale in patients with mechanical neck pain without upper extremity symptomsPhysiotherapy Theory and Practice 2019 35(12):1328-35.10.1080/09593985.2018.147176329856244 [Google Scholar] [CrossRef] [PubMed]
[6]. Kwan YH, Yong ST, Fong W, Lui NL, Malhotra R, Ostbye T, Thumboo J, Reliability and validity of the Short-Form 36 (SF-36) health survey in patients with spondyloarthritisValue in Health 2016 19(7):A85410.1016/j.jval.2016.08.455 [Google Scholar] [CrossRef]
[7]. Hancock GE, Hepworth T, Wembridge K, Accuracy and reliability of knee goniometry methodsJournal of Experimental Orthopaedics 2018 5(1):01-06.10.1186/s40634-018-0161-530341552 [Google Scholar] [CrossRef] [PubMed]
[8]. Carr F, The ‘hidden’ SAPHO syndromeCase Reports 2014 2014:bcr201320166510.1136/bcr-2013-20166524473422 [Google Scholar] [CrossRef] [PubMed]
[9]. Maugars Y, Berthelot JM, Ducloux JM, Prost A, SAPHO syndrome: A follow-up study of 19 cases with special emphasis on enthesis involvementThe Journal of Rheumatology 1995 22(11):2135-41. [Google Scholar]
[10]. Hammond A, Rehabilitation in rheumatoid arthritis: A critical reviewMusculoskeletal Care 2004 2(3):135-51.10.1002/msc.6617041978 [Google Scholar] [CrossRef] [PubMed]
[11]. Hinman RS, Heywood SE, Day AR, Aquatic physical therapy for hip and knee osteoarthritis: Results of a single-blind randomized controlled trialPhysical Therapy 2007 87(1):32-43.10.2522/ptj.2006000617142642 [Google Scholar] [CrossRef] [PubMed]