Caesarean section is a very common surgical procedure in obstetric practice both in developed and developing countries [1-3]. Just like every other major surgery, it is not without complications, which could be foetal or maternal [4,5]. The maternal mortality and morbidity associated with the procedure are becoming rare as a result of improved surgical skill, better anaesthetic technique, use of thrombo-prophylaxis, improved blood transfusion facilities, and availability of potent antibiotics [6,7]. However, genitourinary infection remains one of the most common morbidities of caesarean delivery, accounting for 1.7 per 1000 caesarean sections [8]. Prior to either elective or emergency caesarean section, preoperative assessment of the patient is usually carried out to ensure both optimal intraoperative and postoperative outcomes. One of these preparations routinely done before the caesarean section is the placement of an indwelling urinary catheter and its retention for 24 hours after the procedure [9,10]. The empirical use of an indwelling urethral catheter during caesarean section is aimed at emptying or decompressing the bladder which allows for the proper visualisation of the lower segment, minimising the risk of accidental bladder injury intraoperatively, as well as avoiding postoperative urinary retention [11-13].
Urinary Tract Infection (UTI) is a significant problem following urethral catheterisation in caesarean section [14-17] and it is the most common aetiology for post caesarean section febrile morbidity with a reported incidence range of 2-31.4% [8,18,19]. The condition could also become lethal, especially when adequate treatment is not offered, resulting in pyelonephritis and urosepsis. UTI is more common when there is a practice of catheterisation in the ward before caesarean section in less hygienic circumstances, as well as in patients with diabetes mellitus, sickle cell trait, anatomical defect of the urinary tract, and those who have an indwelling catheter for a long period of time [20-22]. Although pregnancy itself is a risk factor for UTI, urinary tract morbidities including UTI and voiding difficulties experienced following caesarean section are preventable [16,23].
The risk of UTI is associated with urethral catheterisation before caesarean section, the perceived benefit of emptying the bladder is to prevent intraoperative bladder injury. Also, the possibility of urinary retention and postpartum haemorrhage due to bladder atony in non-catheterised patients is a matter of concern to obstetricians. Previous studies have shown an increased risk of UTI in women who had urethral catheterisation preoperatively before an elective caesarean section when compared to those who were not catheterised. However, the incidence of urinary retention and other complications were not consistent [15,13,24]. In Egypt, a randomised multicentre study reported a significantly higher incidence of UTI in the catheterised group but, there was no case of accidental cystostomy or urinary retention [24]. A related report from Karachi, Pakistan [25] also found no case of accidental cystostomy in both catheter and non-catheter groups; however, the incidence of UTI and urinary retention were significantly higher in the catheter group. Furthermore, a systematic review [13] showed that non-catheterisation before caesarean section was associated with a lower incidence of UTI when compared to the catheterised women but urinary retention rates did not differ between the two groups.
The controversy associated with the benefits or otherwise of non-use of routine urinary bladder catheterisation during caesarean section is far from being settled. Also, the non-uniformity of the study methods in previous studies, such as elective or emergency caesarean section, the time interval for removal of an indwelling catheter, participants’ randomisation, and assessment of postpartum haemorrhage due to urinary retention, justify the need for further studies on the subject. This study, therefore, was aimed at determining the impact of non-catheterisation of the urinary bladder on the incidence of significant bacteriuria and other perioperative urinary bladder morbidities during elective caesarean section in Enugu, Nigeria.
Materials and Methods
The study was a multicentre, non-inferiority, randomised control study of consenting eligible pregnant women booked for elective caesarean section at term within the study period. Data collection commenced after ethical approval by the University of Nigeria Teaching Hospital, Ituku-Ozalla Health Research Ethics Committee. The ethical clearance number is NHREC/05/01/2008R and sample collection was done within the study period. A total of 264 pregnant women who met the study criteria and completed the study from 1st May 2012 to 30th April 2013 was included. Written informed consent was obtained from every participant before the commencement of the study. The study was reported according to CONSORT guidelines and followed the standards of Good Clinical Practice (GCP).
The study was conducted at the UNTH, MOCSH, and BASH, all in Enugu State, Southeast Nigeria. UNTH is a Federal teaching hospital, MOCSH is a multi-speciality mission hospital, and BASH is a private specialist hospital in general obstetrics and gynaecology. Enugu is the capital city of Enugu State and it is also called the “Coal City” and is one of the states in the South-east geo-political zones of Nigeria. All these study centres are located in Enugu, Nigeria.
Inclusion and Exclusion criteria: All term pregnant women booked for uncomplicated elective caesarean section at the study centres were eligible for the study. Exclusion criteria included women with high-risk pregnancies like pre-eclampsia, placenta previa, placenta abruption, previous history of primary postpartum haemorrhage, etc. Also, pregnant women with features of pre-existing UTI, diabetes mellitus, sickle cell anaemia, and women who had significant bacteriuria on pre-operation urine microscopy and culture were excluded from the study.
Sampling Technique
The participants were selected following a two-staged/multiphase sampling technique. At the primary level, the hospitals were stratified into teaching, private, and mission hospital groups. From these strata, these hospitals were randomly selected for the study. The eligible participants were proportionally selected using randomisation from the strata of participants in the hospitals.
Intervention
Every participant emptied the urinary bladders before the spinal anaesthesia was administered. The group B women received urethral catheterisation using silicone-coated latex 2-way Foley catheter size 16FR/CH (Boenmed, China) on the operating table using an aseptic procedure, and the catheters were removed 24 hours after the surgery. Every participant received intraoperative prophylactic antibiotics 1.2 g of Augmentin (amoxicillin with clavulanic acid). The sample size apportioned to each study centre was calculated at a ratio of 2: 1.5: 1 to the UNTH, BASH, and MOCSH respectively based on the average number of elective caesarean sections carried out at these centres.
Clean catched urine samples were collected from each participant 72 hours after the surgery for urine microscopy and culture. The microbiology study was done by a dedicated laboratory scientist blinded to the group allocation. Caesarean section was carried out using standard technique. Six surgeons including two senior residents and four consultant Obstetrician/Gynaecologist Surgeons were involved in the surgeries.
Outcome Measures
The primary outcome measure was the incidence of significant bacteriuria 72 hours postoperatively, defined as greater than 100,000 bacteria of the same colony per milliliter of urine in a mid-stream urine sample [26]. The secondary outcome measures included incidence of intraoperative bladder injury, urinary retention (defined as difficulty in passing urine with a palpable tender urinary bladder that necessitated catheterisation) [25], and postpartum haemorrhage as a result of bladder atony following urinary retention.
Sample size calculation: Applying a sample size calculation formula for non-inferiority randomised controlled trial design, N=2 {(Z1-α+ Z1-β)/ϓ}2×p×(1-p) [27], and the study designed to identify a risk ratio of 0.1 for the primary outcome measure, a sample size of 132 women per group was adequate for the study. This was based on the incidence of bacteriuria of 11.2% from a related study [28], power of 80% at 95% confidence level, and a dropout rate of 5%.
Randomisation and Sample Recruitment
Participants were randomised into either intervention group (A) to receive no urethral catheterisation and control group (B) to receive urethral catheterisation before elective caesarean section. The randomisation was achieved using two equal sets of computer-generated random numbers (1-264) developed by an independent statistician-each set represented a study group. Opaque envelopes were labelled sequentially from 1 to 264; for each envelope, the corresponding study group (A or B) was concealed in it and sealed. The envelopes were kept by a medical intern (third party), blinded to the study’s objectives. The eligible women were identified at the antenatal clinics and recruited on admission in the antenatal wards of the study centres. Thus, once a woman was deemed eligible and had given written informed consent, she was assigned a sequential study number. The medical intern keeping the random number sequence was contacted to open the envelope corresponding to the participant’s study number; following which the woman was allocated to the study group A or B concealed in the envelope.
Statistical Analysis
The Statistical Package for the Social Sciences (SPSS) version 15.0 for Windows (SPSS Inc., Chicago, Illinois), was used for data analysis. Chi-square tests were used to compare categorical data and Independent t-test for continuous data. A p-value of <0.05 was considered to be statistically significant.
Results
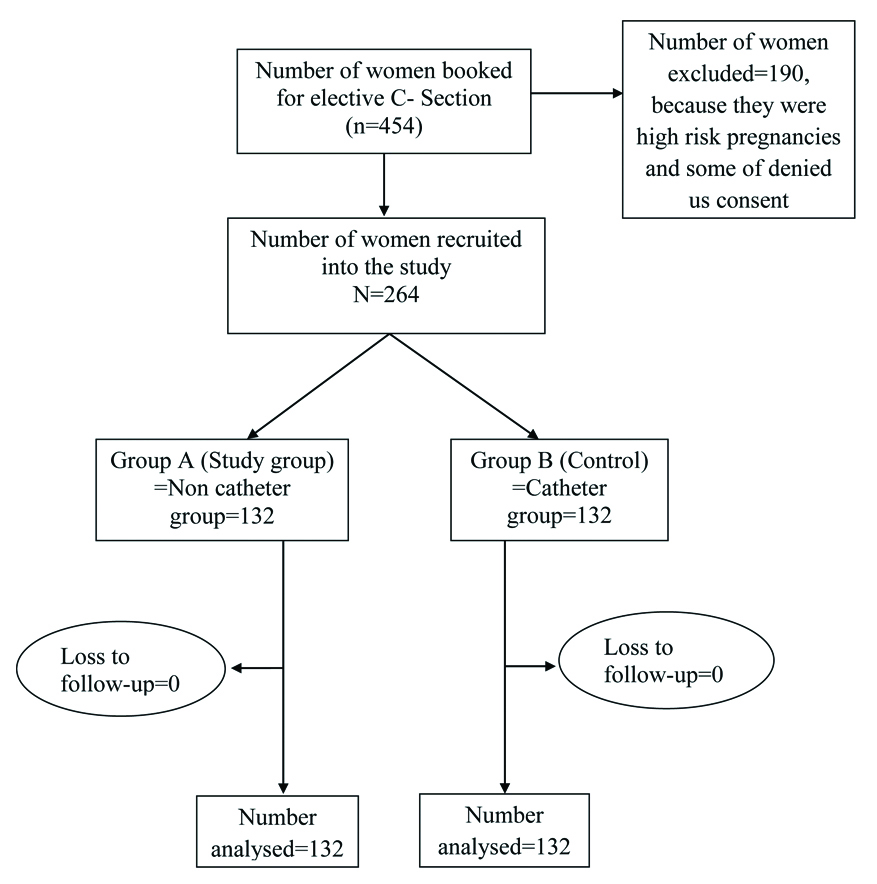
Out of a total of 454 participants who were booked for elective caesarean section and assessed for eligibility, 264 participants met the study criteria. The remaining 190 participants were excluded because they were having either high-risk pregnancies (178) or some eligible participants (12) refused to give consent to participate in the study. None of the participants were lost to follow-up. Therefore, a total of 264 pregnant women who met the study criteria were randomised into intervention (non-catheterisation) group (n=132) and control (catheterisation) group (n=132), and intention-to-treat analysis was applied (data of both groups were completely captured). [Table/Fig-1] shows the flow chart. The recruitment for the study participants ended when the calculated sample size was attained.
Randomisation flow chart.
Basic characteristics of participants were not significantly different between the intervention and control groups; the mean age of the women was 31.2 (SD 4.85) (range=20-45) years for the intervention group and 31.4 (SD 4.56) (range: 19-45) years for the catheter group (p-value=0.745). A majority of the women were multiparous and within 30-39 years age group [Table/Fig-2].
Basic characteristics of study participants.
| Characteristics | Sub-group | Non-catheter (n=132) | Catheter (n=132) | p-value |
|---|
| Frequency n (%) | Frequency n (%) |
|---|
| Age (years) | <20 | 3 (2.3%) | 1 (0.8%) | |
| 20-29 | 40 (30.3%) | 42 (31.8%) |
| 30-39 | 79 (59.8%) | 82 (62.1%) |
| ≥40 | 10 (7.6%) | 7 (5.3%) |
| Mean (SD) | 31.2 (4.85) | 31.4 (4.56) | 0.745 |
| Parity | Para 0 | 22 (16.8%) | 18 (13.6%) | |
| 1 | 13 (9.8%) | 20 (15.2%) |
| 2-4 | 90 (68.1%) | 87 (65.9%) |
| ≥5 | 7 (5.3%) | 7 (5.3%) |
| Mean (SD) | 2.2 (1.42) | 2.3 (1.44) | 0.768 |
| Educational status | Primary | 11 (8.3%) | 15 (11.4%) | 0.631 |
| Secondary | 56 (42.4%) | 61 (46.3%) |
| Tertiary | 64 (48.5%) | 56 (42.3%) |
| No formal education | 1 (0.8%) | 0 (0.0%) |
Independent t-test was used; SD: Standard deviation
The indications for the caesarean delivery for both groups were many and varied. The most common indication for both groups was two or more previous caesarean sections (37.8%, 50/132 versus (39.4%, 52/132, p-value=0.9) [Table/Fig-3].
Indication for caesarean section.
| Indication for caesarean section | Non-catheter group (n=132) | Catheter group (n=132) |
|---|
| n (%) | n (%) |
|---|
| One previous C-section | 19 (14.3) | 26 (19.7) |
| More than two previous C-section | 50 (37.8) | 52 (39.4) |
| Abnormal lies | 11 (8.2) | 17 (12.8) |
| Patient’s request | 10 (7.5) | 8 (6.1) |
| Foetal anomaly† | 0 (0.0) | 2 (1.6) |
| Placenta praevia | 1 (0.7) | 2 (1.6) |
| Foetal macrosomia | 3 (2.8) | 1 (0.7) |
| Elderly primigravida | 1 (0.7) | 1 (0.7) |
| *Others | 37 (28.0) | 23 (17.4) |
*these included higher order multifoetal gestation, prolonged infertility with pregnancy achieved through Assisted Reproductive Technology (ART), fibroid occupying the lower uterine segment, Rhesus Isoimmunisation. †Foetal Anomaly: Anomalies neck tumours and hydrocephaly; c-section: Caesarean section
Nine (6.8%) women in the non-catheter group had significant bacteriuria as against 17 (12.9%) women in the control group. The observed difference was not statistically significant {Relative Risk (RR)=0.5 (95%CI: 0.24-1.14), p-value=0.098} [Table/Fig-4].
Relationship between the occurrence of significant bacteriuria, postoperation urinary retention and use of catheter among the study participants.
| Variable | Subcategory | Catheter use | p-value |
|---|
| No (%) | Yes (%) |
|---|
| Significant bacteriuria | Yes | 9 (6.8) | 17 (12.9) | 0.098 |
| No | 123 (93.2) | 115 (87.1) |
| Postoperation urinary retention | Yes | 14 (10.6) | 0 (0) | <0.001 |
| No | 118 (89.4) | 132 (100) |
p<0.05 considered significant
Postoperation urinary retention was observed in 14 (10.6%) women in the non-catheterisation group, thereby requiring postoperative catheterisation; there was no case of urinary retention in the catheterisation group (p<0.001; risk difference=10.6). Intraoperative bladder injury did not occur in any of the study participants. Also, there was no case of postpartum haemorrhage among participants who had postoperation urinary retention.
Discussion
This study assessed the effect of non-catheterisation of the urinary bladder during an elective caesarean section on the incidence of significant bacteriuria and other urinary bladder complications. There was no case of intraoperative bladder injury in this study which is similar to findings from previous studies [9,12,28]. Availability of good surgical skills, including the routine formation of bladder flap during caesarean section at the study centres as well as routine preoperative voiding of urine by participants before spinal anaesthesia administration might have contributed to the absence of injury to the bladder during the study. The practice of voiding urine before the caesarean operation gives an opportunity for the incision at the uterine lower segment to be accomplished before the bladder starts refilling.
Though, the incidence of significant bacteriuria in the non-catheterisation group was about half of that for participants in the catheterisation group, the difference was not statistically significant. This finding conforms with the reports of a related study in Onile TG et al., Southwest Nigeria [28]. However, it differs from previous studies that reported significantly increased UTI in the catheterisation group [13,29]. The observed confidence interval of the significant bacteriuria risk ratio estimate suggests low study precision, which is expected to improve with a larger sample size. Thus, a multicentre larger sample size trial is recommended.
With respect to postoperative urinary retention, this study showed that the non-catheterisation group had 14 cases of urinary retention while the catheterisation group had none. The difference in the incidence of urinary retention, though a secondary outcome of the study, was expectedly significant because of factors that include pregnancy state itself, caesarean section, regional anaesthesia, and the use of postoperative opioid analgesia [30-32]. The urinary retention incidence of 10.6% in the non-catheterisation group in this study was similar to the 13.3% reported in a related study from Pakistan [25]. Nevertheless, the later study [25], also observed a 3.3% incidence of urinary retention in the catheterisation group unlike in this study where urinary retention was not observed in a similar group. The findings of the catheterisation group are also in keeping with the results of a related study from Iran [9]. The Pakistan study removed the urethral catheter from participants after 12 hours postoperation, which might explain the occurrence of urinary retention unlike in this study where the catheter was removed after 24 hours postoperation. To prevent urinary retention after caesarean section and its complications, development and compliance with postoperative void review protocol are encouraged [33,34].
On the other hand, postpartum haemorrhage due to bladder atony was not observed in this study, probably due to the small number of participants who had urinary retention.
Limitation(s)
The study was limited by the inevitable use of prophylactic antibiotics for the elective caesarean section which could have masked the development of significant bacteriuria. Furthermore, the restriction of the study to uncomplicated elective cases might have contributed to the absence of bladder injury because it has been shown that the risk of urinary bladder injury is higher during emergency caesarean section when compared to elective caesarean section [35].
Conclusion(s)
Non-catheterisation of the urinary bladder during elective caesarean section had no significant relationship with the incidence of significant bacteriuria among women in Enugu, Nigeria. However, when compared with women who were catheterised up to 24 hours after caesarean section, non-catheterised women seemed to have a higher risk of developing postoperative urinary retention requiring urethral catheterisation. Therefore, because of the rising caesarean section rate in the study environment, lack of association between urethral non-catheterisation with significant bacteriuria, and higher risks of urinary retention in non-catheterised participants, the practice of preoperative urethral catheterisation and removal after 24 hours should be encouraged, especially in settings where compliance with postoperative void review protocol are likely to be sub-optimal for reasons including inadequate nursing staff.
Independent t-test was used; SD: Standard deviation
*these included higher order multifoetal gestation, prolonged infertility with pregnancy achieved through Assisted Reproductive Technology (ART), fibroid occupying the lower uterine segment, Rhesus Isoimmunisation. †Foetal Anomaly: Anomalies neck tumours and hydrocephaly; c-section: Caesarean section
p<0.05 considered significant