A Structured Maternity Case Record to Improve Quality of Documentation in a Tertiary Care Hospital, Delhi
AG Radhika1, Chetna Dengri2, Abhishek Kumar3, Shalini Singh4
1 Consultant, Department of Obstetrics and Gynaecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
2 Undergraduate Student, Department of Obstetrics and Gynaecology, University College of Medical Sciences and Guru Teg Bahadur Hospital, Delhi, India.
3 Scientist-B, Division of Reproductive Biology Maternal and Child Health, Indian Council of Medical Research, HQRS, V. Ramalingaswami Bhawan, Ansari Nagar, New Delhi, India.
4 Scientist-F, Division of Reproductive Biology Maternal and Child Health, Indian Council of Medical Research, HQRS, V. Ramalingaswami Bhawan, Ansari Nagar, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: AG Radhika, Consultant, Department of Obstetrics and Gynaecology, 7th Floor, MCH Block, GTB Hospital, Delhi, India.
E-mail: raradhikaag@gmail.com
Introduction
India contributes to about 18% of global maternal deaths and 22.6% of still births. Efforts to improve the quality of care are challenged by the lack of reliable documentation of data. Hence, a concise, structured maternity case sheet (PrasavRecord) was designed with the aim to bring about an improvement in documentation of treatment and events related to woman in labour from the time of admission till her discharge from the hospital.
Aim
To study the improvement in quality of documentation from the time of admission till discharge of a woman in labour with the help of structured format i.e., PrasavRecord.
Materials and Methods
The study was conducted in February 2017. A quasi experimental study design was used, and the completeness of data recorded by the resident doctors in the existing hospital case sheet (control group) with those recorded in PrasavRecord (intervention group) were assessed in a total of 65 deliveries in each arm. Details of the patient from admission to the labour room followed by the entire sequence of events during labour as well as hospital stay in postpartum period were recorded over 130 parameters under different sections in PrasavRecord. Statistical analysis was done by using SPSS version 21.0.
Results
Completeness of the documentation in terms of history, investigations and findings at examination including those at labour, nearly, 92% of the doctors rated PrasavRecord as “good and very good” for appearance, recommended its routine use, and 75% agreed that the format will be useful for conversion to electronic medical record. There was highly significant difference between the average percentage of completeness in PrasavRecord 75.8 {95% CI (74.2-77.4)} and hospital case sheets 42.2 {95% CI (40.9-43.6)} i.e., z=5.38 p-value <0.001.
Conclusion
PrasavRecord is a simple, acceptable and user-friendly data entry format which improves the quality of documentation of the processes and practices during childbirth. Larger trials are required to finetune it to facilitate its widespread use thereby, ensuring a uniform documentation process of labour and postpartum.
Childbirth, Hospital case records, Maternity care, Prasav record
Introduction
India contributes to about 18% of global maternal deaths and 22.6% of still births [1]. To bring about an improvement in the present situation, determinants of maternal and neonatal morbidity and mortality, need to be identified and tackled on priority basis. Maternal and perinatal death reviews and audits are promising strategies to identify health systems deficiencies and quality of care that women receive during childbirth [2]. However, due to incomplete and non-uniform documentation in health facilities, there is lack of reliable maternal and neonatal data in our country [3].
This study was based on the conceptual framework which was developed by Donabedian A in 1966 for examining health services and evaluating quality of healthcare [4]. The framework uses three elements of quality (structure, process and outcome). Structure influences process, and in turn, process influences outcome. Structure denotes the attributes of the settings in which care occurs. This includes the attributes of material resources (such as infrastructure, equipment and supplies), human resources (number, variety and qualifications of personnel), and organisational structure. Process denotes what is done in providing and receiving care including the practitioner’s activities in establishing a diagnosis, recommending or implementing treatment. Outcome is the effect of care on the health status of patients and populations.
Currently, patient details in most healthcare facilities in India are maintained in the form of hand-written notes in case sheets. In this unstructured format, there are frequent inadvertent omissions of vital information or the handwriting is illegible. To simplify documentation from admission to labour room till discharge of mother baby pair, the team at GTB Hospital with Indian Council of Medical Research (ICMR), designed a simple tool -PrasavRecord.
Earlier, the ICMR had designed a concise, structured hospital case sheet -Prasavsheet© (‘prasav’ means labour in Hindi) using formative research and inputs from subject experts to record maternal and foetal/neonatal parameters during labour and delivery which has been adapted by Government of India for use in the district health system [5]. The design of “Prasavsheet©” allows encircling of common pre-printed entities and has blank spaces for making patient specific entries as well. It also overcomes issues of inadvertent incomplete entries or data recorded in illegible handwriting and facilitates computerisation of data, if needed. This study evaluated the documentation of maternal and neonatal parameters during labour and postpartum stay which comes under “process” in the quality of care framework. Following the earlier experience of designing Prasavsheet (unpublished) which focused on improving the documentation in labour room, it was realised that inclusion of details of stay in the hospital would ensure completeness of the patient record from the time of admission till discharge.
In this study, additional details were added to Prasavsheet© to capture mother and baby details during hospital stay in postpartum period till discharge. Details of the mother baby pair to be recorded in the postpartum period till discharge were added to the Prasavsheet (which had details to be filled during labour and immediate postpartum only).
The aim of the study was to explore the possibility of improvement in quality of documentation from the time of admission till discharge of a woman in labour with the help of a structured format i.e., PrasavRecord and its acceptance by healthcare providers in tertiary care public hospital in Delhi, India.
Materials and Methods
A quasi-experimental study was conducted in February 2017, after Approval from the Institutional Review Board of Guru Teg Bahadur Hospital, Delhi (IEC-HR/2017/29/11) which is a government referral hospital and medical college with 18000 labour room deliveries per annum. This study was conducted to evaluate the frequency of patient related parameters recorded in the control and intervention arms. The control arm filled the hospital case sheets already in use. These have unstructured entries, except, for the front sheet which contains details of patient identification. Two labour rooms in the Department of Obstetrics and Gynaecology, GTB Hospital were chosen for the study. Each labour room has a team of four resident doctors on eight hours shift. Due to the heavy workload in the labour rooms, it was planned to have PrasavRecord filled for the first two new cases admitted in the labour room in each shift i.e., a total of six PrasavRecords were filled per day upto a total of 65 sheets in each arm.
Sample Size Calculation
Pre-testing of the tool (PrasavRecord) for 20 cases was done in November 2016. It was also found that only 23% of total 130 parameters were complete in the currently used hospital records. Expecting an improvement of atleast 60% with the use of PrasavRecord; p=0.60, Z=1.65 i.e., 90% confidence interval and margin of error as 10%. Thus, the required sample size of case records for the study was determined by using the formula given below:
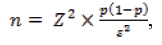
where, n is the sample size, Z is the Z-score, p is the estimate of population proportion, ε is the margin of error to be tolerated.
Hence, sample size obtained was 65 case records in each arm (control and intervention arm).
The PrasavRecord was used per mother baby pair from admission in labour room to the postnatal ward till discharge (intervention) while the existing hospital case sheets were used for the other arm (control). The intervention tool was self-explanatory and no formal training was imparted to the resident doctors for using it. Both types of sheets i.e., the completed PrasavRecord and equal number of completed hospital case sheets were assessed after patient discharge for completeness and uniformity. At the end of study, the resident doctors were requested to complete a questionnaire based on a five-point Likert scale, for assessing the acceptability of the intervention tool [Annexure].
Statistical Analysis
Data extracted from the study tools was analysed in SPSS version 21.0 (IBM SPSS Statistics 21.0). Data was reported as simple statistics, including number (percentage). The average percentage of completeness along with its 95% confidence interval was reported for both the groups. The average proportion of completeness was compared using two samples z-test for proportion considering average completeness as proportion. The p-value less than 0.05 were considered as significant.
Results
Completeness of parameters recorded in the currently used hospital case sheets (Control) and PrasavRecord (Intervention) are shown in the [Table/Fig-1,2 and 3]. While the very first examination findings at admission were found complete, subsequent noting recorded the parameters specifically being monitored for progress of labour. Recording of investigations (haemoglobin, blood group, Rhesus (Rh) factor, Veneral Disease Research Laboratory (VDRL), Human Immunodeficiency Virus (HIV), Hepatitis B surface Antigen (HBsAg) and ultrasound findings) were similar in the two arms [Table/Fig-4]. An important observation regarding the hospital case sheet was the haphazard entries of notes. The chronological sequence was frequently missing making it difficult to follow the sequence of events or treatment. Addition of new sheets of paper, inter-departmental referrals, hand drawn tables for recording patient progress resulted in interruption of the sequence while understanding the events through PrasavRecord was effortless and fast.
Percentages of parameters recorded for investigations and in early labour.
| Parameters | Records studied | Hospital case sheet (control arm) | PrasavRecord (intervention arm) |
|---|
| N (%) | N (%) |
|---|
| Admission finding | Fundal height | 11 (16.9) | 65 (100.) |
| Multiple pregnancy | 0 (0.0) | 64 (98.5) |
| Lie | 53 (81.5) | 50 (76.9) |
| Presentation | 45 (69.2) | 50 (76.9) |
| Liquor | 40 (61.5) | 35 (53.8) |
| Duration of contraction | 0 (0.0) | 28 (43.1) |
| Fetal heart rate | 37 (56.9) | 59 (90.8) |
| Investigation | Cardiotocograph findings | 0 (0.0) | 18 (27.7) |
| Systemic examination | 6 (9.2) | 65 (100.0) |
| Haemoglobin | 65 (100.0) | 64 (98.5) |
| Blood group | 65 (100.0) | 62 (95.4) |
| Rh factor | 65 (100.0) | 62 (95.4) |
| VDRL | 65 (100.0) | 61 (93.8) |
| HIV | 65 (100.0) | 61 (93.8) |
| HBsAg | 65 (100.0) | 61 (93.8) |
| Urine albumin and sugar | 16 (24.6) | 43 (66.2) |
| Blood sugar | 16 (24.6) | 43 (66.2) |
| Ultrasound | 62 (95.4) | 64 (98.5) |
Rh factor: Rhesus; VDRL: Veneral disease research laboratory; HIV: Human immunodeficiency virus; HBsAg: Hepatitis B surface antigen
Percentages of parameters recorded during active labour and immediately after delivery (third stage) in both arms.
| Parameters | Records studied | Hospital case sheet (control arm) | PrasavRecord (intervention arm) |
|---|
| N (%) | N (%) |
|---|
| During active labour | Temperature | 7 (10.8) | 58 (89.2) |
| Pulse | 7 (10.8) | 58 (89.2) |
| Blood pressure | 9 (13.8) | 58 (89.2) |
| Uterine contractions | 10 (15.4) | 58 (89.2) |
| Duration of contraction | 10 (15.4) | 58 (89.2) |
| Foetal heart rate | 10 (15.4) | 58 (89.2) |
| Cervical dilation | 11 (16.9) | 58 (89.2) |
| Membranes | 7 (10.8) | 58 (89.2) |
| Drugs given | 7 (10.8) | 58 (89.2) |
| During third phase of labour | Genital injuries | 0 (0.0) | 65 (100) 92.3 |
| Misoprostol | 2 (3.1) | 25 (38.5) 36.9 |
| ANTI D | 0 (0.0) | 17 (26.2) |
| Family planning method | 19 (29.2) | 40 (61.5) |
| Breastfeeding | 0 (0.0) | 37 (56.9) |
Percentages of maternal parameters recorded on first postpartum day.
| Post partum condition of mother and baby | Hospital case sheet | PrasavRecord |
|---|
| N (%) | N (%) |
|---|
| Complaints | 26 (40.0) | 42 (64.6) |
| Temperature | 27 (41.5) | 52 (80.0) |
| Pulse | 43 (66.2) | 52 (80.0) |
| Blood pressure | 43 (66.2) | 52 (80.0) |
| Pallor | 39 (60.0) | 52 (80.0) |
| Oedema | 39 (60.0) | 52 (80.0) |
| Icterus | 11 (16.9) | 52 (80.0) |
| Breast | 8 (12.3) | 45 (69.2) |
| Systemic examination | 9 (13.8) | 45 (69.2) |
| Abdomen | 8 (12.3) | 45 (69.2)64.6 |
| Bleeding PV | 40 (61.5) | 65 (100.0) |
| Episiotomy | 9 (13.8) | 65 (100.0) |
| Passed urine | 34 (52.3) | 65 (100.0) |
| Passed stool | 29 (44.6) | 65 (100.0) |
[Table/Fig-4,5] describe the Likert scale rating of thirteen resident doctors regarding their perception on the different attributes of the PrasavRecord and the existing hospital case sheet was rated as “good and very good” by 69.2% and 23.%, respectively and usefulness of PrasavRecord for recording labour processes was rated also as “good and very good” by 69.2% and 23.%, respectively versus 38.4% as good, none as very good for appearance of hospital case sheets. Ease of recording without missing details in PrasavRecord was recorded as ‘good’ and ‘very good’ by 61.5% and 23%, respectively, while that for hospital records 23% (good) and none (very good). Majority agreed that PrasvRecord would facilitate electronic medical record keeping during childbirth (38.4% ‘good’ and ‘very good’ each). Most of the participants agreed that the PrasavRecord is useful for recording labour processes, post-partum condition of mother and newborn. Overall rating for hospital records was average by 76.9% and good by 15.5%, none rated it as “very good” compared to 92.3% (good) and 7.6% (very good) for PrasavRecord. Two of the residents expressed that complete sentences in hospital records did contribute to better understanding. The only reservation expressed with PrasavRecord was the constraint of space for recording comments or other observations.
Performance of PrasavRecord on Likert scale as rated by the doctors.
| Attributes | Very poor | Poor | Average | Good | Very good |
|---|
| N (%) | N (%) | N (%) | N (%) | N (%) |
|---|
| Appearance | 0 (0.0) | 1 (7.6) | 0 (0.0) | 9 (69.2) | 3 (23.0) |
| Adequate space for recording parameters | 0 (0.0) | 1 (7.6) | 4 (30.7) | 8 (61.5) | 0 (0.0) |
| Ease of recording without missing details | 0 (0.0) | 1 (7.6) | 1 (7.6) | 8 (61.5) | 3 (23.0) |
| Comprehension of instructions | 0 (0.0) | 0 (0.0) | 1 (7.6) | 9 (69.2) | 3 (23.0) |
| Usefulness to record labour processes | 0 (0.0) | 0 (0.0) | 1 (7.6) | 10 (76.9) | 2 (15.3) |
| Usefulness to record postpartum condition of mother | 0 (0.0) | 0 (0.0) | 1 (7.6) | 9 (69.2) | 3 (23.0) |
| Usefulness to record newborn’s condition | 0 (0.0) | 0 (0.0) | 0 (0.0) | 8 (61.5) | 5 (38.4) |
| Facilitates uniform recording | 0 (0.0) | 0 (0.0) | 1 (7.6) | 8 (61.5) | 4 (30.7) |
| Will facilitate electronic medical record keeping during childbirth | 0 (0.0) | 0 (0.0) | 3 (23.0) | 5 (38.4) | 5 (38.4) |
| Overall rating | 0 (0.0) | 0 (0.0) | 0 (0.0) | 12 (92.3) | 1 (7.6) |
Performance of hospital case record on Likert scale as rated by the doctors.
| Attributes | Very poor | Poor | Average | Good | Very good |
|---|
| N (%) | N (%) | N (%) | N (%) | N (%) |
|---|
| Appearance | 2 (15.3) | 1 (7.6) | 5 (38.4) | 5 (38.4) | 0 (0.0) |
| Adequate space for recording parameters | 0 (0.0) | 2 (15.3) | 2 (15.3) | 8 (61.5) | 1 (7.6) |
| Ease of recording without missing details | 0 (0.0) | 3 (23.0) | 7 (53.8) | 3 (23.0) | 0 (0.0) |
| Comprehension of instructions | 1 (7.1) | 3 (21.4) | 7 (50.0) | 1 (7.1) | 1 (7.1) |
| Usefulness to record labour processes | 0 (0.0) | 5 (38.4) | 5 (38.4) | 2 (15.3) | 1 (7.6) |
| Usefulness to record postpartum condition of mother | 0 (0.0) | 3 (23.0) | 6 (46.1) | 3 (23.0) | 1 (7.6) |
| Usefulness to record newborn’s condition | 1 (7.6) | 6 (46.1) | 3 (23.0) | 3 (23.0) | 0 (0.0) |
| Facilitates uniform recording | 2 (15.3) | 1 (7.6) | 7 (53.8) | 2 (15.3) | 1 (7.6) |
| Will facilitate electronic medical record keeping during childbirth | 0 (7.6) | 4 (30.7) | 8 (61.5) | 0.0 | 1 (7.6) |
| Overall rating | 1 (7.6) | 0.0 | 10 (76.9) | 2 (15.5) | 0.0 |
The average percentage of completeness in PrasavRecord was 75.8 (95% CI: 74.2-77.4) and for hospital cases sheet was 42.2 (95%CI: 40.9-43.6). Using these average percentages as proportion in z-test, the result revealed a highly significant difference between these two records (z=5.38; p<0.001) [Table/Fig-6].
Comparison of completeness of documentation in hospital case sheets and PrasavRecord.
| Type of case record | Completeness (n, %) |
|---|
| Hospital case sheets | 27, 42.2% (95% CI 40.9-43.6) |
| PrasavRecord | 50,75.8% (95% CI: 74.2-77.4) |
(Z=5.38; p<0.001); two samples z test used
Discussion
This project was planned to explore if user friendly structured case record from the time of admission to discharge would result in better documentation. This study demonstrated that documentation of patient details and labour room events were much better with PrasavRecord than that seen in the case sheets presently in use. Clinical records of 1239 births in public healthcare facilities in Madhya Pradesh were reviewed to study the quality of documentation. Only 1.9% records documented advice at discharge, 13.8% had postnatal blood pressure and 35.3% documented fetal heart rate [6]. An observational study of 1479 women in labour indicated partograph plotting in only 15.8% of deliveries [7]. A cross-sectional survey conducted in healthcare facilities of Punjab and North West Frontier province in Pakistan, to assess Emergency Obstetric Care (EmOC) services indicated that problems such as incompleteness, inaccuracy and duplication of data made it difficult for researchers to identify and define problems accurately and reliably. They also reported that, there is lack of motivation among health service personnel, since they rarely receive feedback on the data reported to higher levels and, little incentive to ensure the quality of data collected [8,9].
Proper documentation of clinical records is important in assigning cause for maternal and perinatal morbidity and mortality. Lack of basic health data makes it difficult to formulate policy for appropriate and rational resource allocation for patient care and disease prevention [10]. Collating of data from hospitals on standard indicators of quality of patient care that report maternal deaths is presently not followed in India therefore, little information can be gathered about the exact causes of maternal deaths [11]. Presently, the Health Ministry in India is working to setup an Integrated Health Information Platform (IHIP) [12].
To enable creation of inter-operable health records with the objective to replace existing paper records, as storing unstructured medical records on computer, is a difficult and impractical exercise. The electronic records, besides eliminating difficulties of deciphering poor handwriting or lost medical records, would allow accessibility by a wider group of care givers such as clinicians, pharmacists in different clinics and the patients’ themselves [13].
Structured ward round proforma improves documentation, communication, and overall quality of care. This was demonstrated in the studies focussing on ward rounds and surgical admissions [14,15]. Filling the forms was found to be very comfortable by all the participants though initially it took time to fill the same and 77% doctors expressed that PrasavRecord will facilitate electronic medical record keeping.
This study demonstrates that a well-made structured proforma can significantly enhance the quality of documentation. As an indirect benefit, the new proforma also improved the way in which patients in labour and postpartum were clinically assessed as it also served as a checklist. The long-term vision is to incorporate this proforma into an electronic medical record, which is believed to provide superior results to handwritten records [16].
In this study, all doctors agreed that the existing unstructured hospital case sheets are not suitable for electronic medical record keeping. The marked improvement of recording of various patient parameters in PrasavRecord shows changes in “process” of documentation. Introduction of PrasavRecord will act as a preliminary step in structuralising the paper-records of labour and peurperium and help in effective auditing. In addition, PrasavRecord can be converted easily into electronic format which will substantially improve the documentation and assist in addressing lacunae in healthcare delivery in India.
Limitation(s)
The design of this study focussed only on quality of documentation, clinical outcomes were not compared. In addition, while the authors relied heavily on the documentation for proof of clinical assessments and treatment, the authors were able to observe that a large amount of clinical activity took place in an undocumented fashion also e.g., more frequent patient monitoring, counselling etc. This came to light during conversation with few residents who had participated in the study. This is the first step towards further improvement of the hospital case records. The study was not blinded for duration of professional experience i.e., more experienced care givers might have better unstructured notes. An important drawback of using a proforma is the increased time initially required for its proper completion because of the learning curve involved in such a change of practice.
Conclusion(s)
PrasavRecord is a particularly useful simplified form of recording of the longitudinal progress from admission till discharge of the mother and newborn. The acceptance of this simple to use proforma among the resident doctors was high thereby confirming its utility.
Rh factor: Rhesus; VDRL: Veneral disease research laboratory; HIV: Human immunodeficiency virus; HBsAg: Hepatitis B surface antigen
(Z=5.38; p<0.001); two samples z test used
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 30, 2020
Manual Googling: Jan 04, 2021
iThenticate Software: Jan 23, 2021 (8%)
[1]. Registrar General of India. Special Bulletin on Maternal Mortality in India: 2007-09. Sample Registration System; 2013 [Google Scholar]
[2]. Broek NR van den, Graham WJ, Quality of care for maternal and newborn health: The neglected agendaBJOG 2009 116(Suppl. 1):18-21.10.1111/j.1471-0528.2009.02333.x19740165 [Google Scholar] [CrossRef] [PubMed]
[3]. Mann R, Williams J, Standards in medical record keepingClinical Medicine 2003 3(4):329-32.10.7861/clinmedicine.3-4-32912938746 [Google Scholar] [CrossRef] [PubMed]
[4]. Donabedian A, The quality of care. how can it be assessed?JAMA 1988 260(12):1743-48.10.1001/jama.260.12.17433045356 [Google Scholar] [CrossRef] [PubMed]
[5]. https://main.icmr.nic.in/sites/default/files/annual_repoorts/ICMR_AR_English_2018_19.pdf [Google Scholar]
[6]. Chaturvedi S, Randive B, Raven J, Diwan V, Costa AD, Assessment of the quality of clinical documentation in India’s JSY cash transfer program for facility births in Madhya PradeshInternational Journal of Gynecology and Obstetrics 2016 132(2):179-83.10.1016/j.ijgo.2015.07.01626810337 [Google Scholar] [CrossRef] [PubMed]
[7]. Singh S, Kashyap JA, Chandhiok N, Kumar V, Singh V, Goel R, Labour & delivery monitoring patterns in facility births across five districts of India: A cross-sectional observational studyIndian J Med Res 2018 148(3):309-16.10.4103/ijmr.IJMR_103_1830425221 [Google Scholar] [CrossRef] [PubMed]
[8]. Ali M, Kuroiwa C, Accurate record keeping in referral hospitals in Pakistan’s North West Frontier Province and Punjab: A crucial step needed to improve maternal healthJournal of Pakistan Medical Association 2007 57(9):443-46. [Google Scholar]
[9]. Bali A, Bali D, Iyer N, Iyer A, Management of medical records: Facts and figures for surgeonsJ Maxillofac Oral Surg 2011 10(3):199-202.10.1007/s12663-011-0219-822942587 [Google Scholar] [CrossRef] [PubMed]
[10]. Rajivlochan M, Clinical audits and the state of record keeping in IndiaAnnals of Neurosciences 2015 22(4):197-98.10.5214/ans.0972.7531.22040226527163 [Google Scholar] [CrossRef] [PubMed]
[11]. Bramley S, Medical records and the lawBJU International 2000 86(3):286-90.10.1046/j.1464-410x.2000.00294.x10930933 [Google Scholar] [CrossRef] [PubMed]
[12]. https://www.nhp.gov.in/integrated-health-information-platform-(ihip)_ms accessed on 15/7/2020 [Google Scholar]
[13]. Electronic Patient Record (EPR) Benefits Realisation Case Study. https://www.ouh.nhs.uk/patient-guide/documents/epr-case-study.pdf. Accessed on 30/12/19 [Google Scholar]
[14]. Wright DN, Does a post-take ward round proforma have a positive effect on completeness of documentation and efficiency of information management?Health Informatics J 2009 15:86-94.https://doi.org/10.1177/146045820910297010.1177/146045820910297019474222 [Google Scholar] [CrossRef] [PubMed]
[15]. Ehsanullah J, Ahmad U, Solanki K, Healy J, Kadoglou N, The surgical admissions proforma: Does it make a difference?Ann Med Surg (Lond) 2015 4:53-57.https://doi.org/10.1016/j.amsu.2015.01.00410.1016/j.amsu.2015.01.00425750727 [Google Scholar] [CrossRef] [PubMed]
[16]. Zegers M, de Bruijne MC, Spreeuwenberg P, Wagner C, Groenewegen PP, van der Wal G, Quality of patient record keeping: An indicator of the quality of care?BMJ Qual Saf 2011 20:314-18.https://doi.org/10.1136/bmjqs.2009.03897610.1136/bmjqs.2009.03897621303769 [Google Scholar] [CrossRef] [PubMed]