The Cholangiocarcinoma (CCA) is the second most common primary liver tumour worldwide, after hepatocellular carcinoma [1]. Most of the CCA patients appear in advanced stage and often presents with MBO [2,3] in which the pancreatic cancer and CCA are the leading cause [4]. Curative resection is the primary goal of diagnosis and treatment, but the patients rarely achieve these options because 70% of them present with metastatic disease at the time of diagnosis [3,5,6]; thus, the prognosis of MBO is poor, with 5-year OS rates of 4.1% for unresectable group [7].
Malignant Biliary Obstruction (MBO) is often associated with recurrent cholangitis, pruritus, loss of appetite, nausea, and renal failure [3,4]. In this setting, the palliative treatment using biliary drainage is strongly recommended to relieve these symptoms, and improve the Quality of Life (QOL) [8-10]. Endoscopic Retrograde Cholangiopancreatography (ERCP) is the standard procedure used for relief of MBO [3,10]. However, the failed ERCP is common even when performed by skilled endoscopists, and overall Adverse Event (AE) rates have been reported as high as 36% [10,11]. Percutaneous Transhepatic Biliary Drainage (PTBD) and other surgical interventions are the alternative procedures after failed ERCP, however those methods often relate with high AEs and prolong hospitalisation [9,12].
Endoscopic Ultrasound-guided Biliary Drainage (EUS-BD) has been increasingly utilised as an alternative procedure to achieve successful biliary drainage, particularly in cases of failed or unfeasible ERCP. EUS-BD allows the direct visualisation and access to the biliary duct through sonographic guidance. In addition, this procedure is less invasive than the PTBD and other surgical interventions [2,9,11,12].
Most of the previous studies commonly reported long term outcomes in term of comparing stent patency and AEs [13-16]. The data of survival rate of EUS-BD patient is still scarce. A study reported that the EUS-BD was superior to the PTBD in OS for the resectable extrahepatic CCA with MBO [10], and another reported that the patient’s survival rate was higher with ERCP trans papillary stent compared with EUS-BD [17]. Conversely, a meta-analysis study showed that PTBD was superior to EBD in terms of success rate [18] with combined Odd Ratio (OR) of 2.18 (95%CI: 0.73-6.47). A recent meta-analysis study reported that EUS and ERCP had comparable result and is safe for primary treatment for MBO [11,15]. However, some studies with small number of patients reported the controversial long term outcomes of EUS-BD, especially the mortality rates. Therefore, the aim of this study was to compare mortality rates of MBO patients with EUS-BD versus non-EUS-BD patients.
Materials and Methods
This retrospective cohort study enrolled 132 MBO patients receiving palliative treatment between January 2014 to August 2020 at Thabo Crown Prince Hospital, Nong Khai, Thailand. The study protocol was approved by Nong Khai Province Ethics Committee for Human Research. The use of patients’ files and database was approved by Director of Thabo Crown Prince Hospital, Nong Khai, Thailand. The written informed consent for operation was obtained from all patients before the surgery.
Inclusion criteria: All patients in this study were diagnosed as having inoperable malignant obstructive jaundice, based on their clinical symptom (jaundice, dark-coloured urine, and pale stool), laboratory examination (elevated bilirubin level, alkaline phosphatase level, and gamma glutamyl transferase level), and imaging examination including transabdominal ultrasound, Computerised Tomography (CT) scan, and Magnetic Resonance Cholangiopancreatography (MRCP).
Exclusion criteria: Patients with benign pathology, severe coagulopathy, severe thrombocytopenia, and incomplete data were excluded.
The patients were divided into two groups; the patients from January 2014 to 31 March 2017 who were treated in non-EUS era by ERCP, TPBD or surgical interventions, and the EUS era group from 1 April 2020 to August 2020 only the EUS-BD patients were enrolled into the study.
The primary outcome of this study was to compare the OS rate, that defined as the time from treatment until death of the patients, in EUS-BD era (group I) and non-EUS-BD era (group II). Patients who were alive or lost to follow-up at the end of study period were considered as censor outcome in statistical analysis.
The data of the enrolled patients were collected by reviewing the hospital’s electronic medical records, including demographic data (age, gender), the type of treatment (non-EUS era or EUS era), primary disease, history of having previous ERCP or TPBD, type of stent, and follow-up times (person-months). All patients were followed until death or the end of study on 15 August 2020, with a minimum follow-up of two months. The mortality data was retrieved from medical records and national death registration.
Interventions for palliative care of unresectable Malignant Biliary Obstruction (MBO) in Tha-Bo Hospital consisted of: Surgery (palliative resection or bypass), PTBD, ERCP and EUS-BD. All procedures were performed by three surgeons in our hospital. The EUS-BD has three different locations of the stent replacement including; Hepaticogastrostomy (HGS), Hepaticoduodenostomy (HDS) or Choledochoduodenostomy (CDS). Each drainage procedure was selected individually for the patients, based on their clinical presentation and the location of lesions by patient’s imaging.
Statistical Analysis
The sample size was determined for binary covariate cox regression analysis by formula according to Schmoor C et al., [19]. Setting power at a 0.05 significance level to detect a Hazard Ratio (HR) of 2.0, assumed that the mortality rate was 0.75. Categorical data were presented as number and percentages. Fisher’s-exact test was used to compare categorical variables between groups. Continuous data was presented as mean and standard deviation or median and interquartile range depending on data distribution. The normality of data was tested by Skewness and Kurtosis test. The Student’s t-test or Wilcoxon’s rank-sum test was used to compare continuous variables. All tests were two-side and considered to be statistically significant when p-value <0.05.
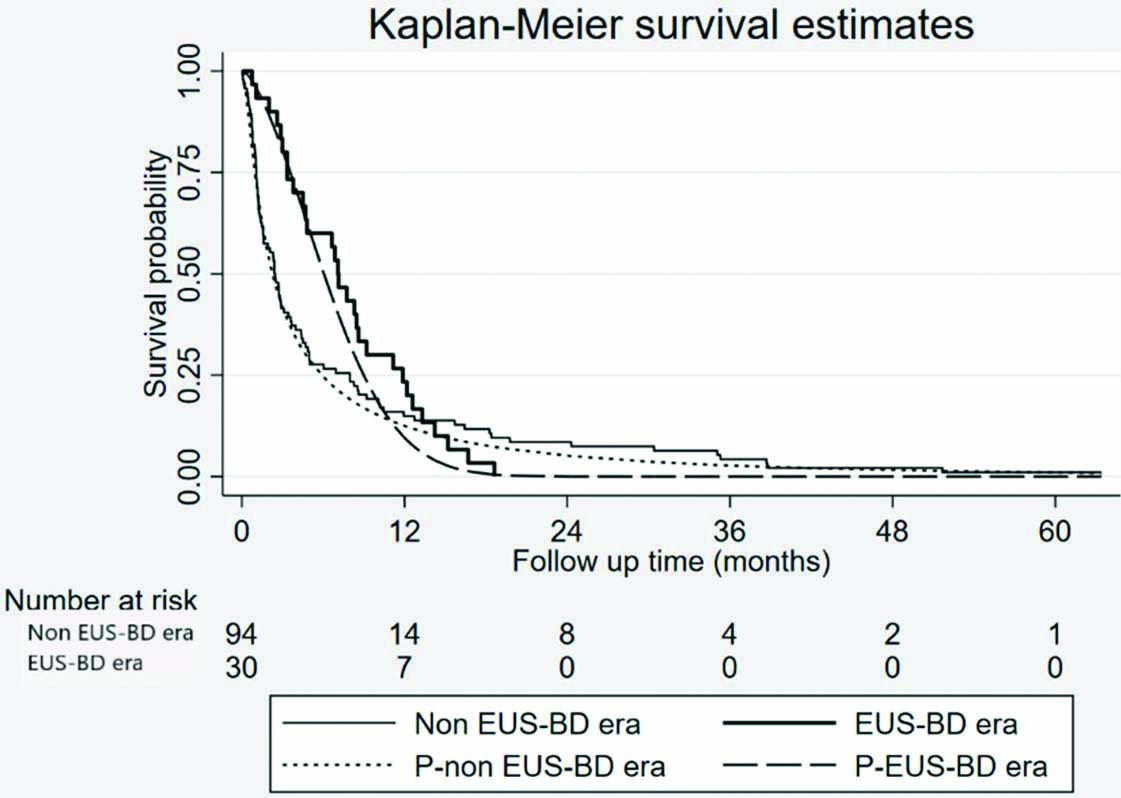
The Overall Survival (OS) rates were compared using both parametric Kaplan-Meier methods and Cox proportional hazard regression. Likewise, Kaplan-Meier (KM) was visualised. Due to the imbalance of follow-up time between the two groups, to quantify treatment effect, HR were estimated from Cox proportional hazard model with restricted mean difference of 12-month- follow-up adjusted by other covariates and were reported 95% confidence intervals and p-value. All statistical analyses were done using Stata version 13.0 (Stata Corp, College Station, TX, United States).
Results
Of the 132 patients, eight patients were excluded due to incomplete data. Of these, 124 were included in the analysis and were divided into two groups, 30 patients to EUS era (group I) and 94 patients to non-EUS era (group II). There were no significant differences in the patient clinical characteristics between two treatment groups except history of ERCP, metallic stent used and follow-up time. The number of patients having previous ERCP in group I was less than group II (87.0% vs 100%; p=0.003), but the patients in group I were used metallic stent more than group II (97.0% vs 46.0%; p<0.001). Similarly, group I had significant follow-up time more than group II (7.12 vs 2.43 person-months; p=0.001) [Table/Fig-1].
Clinical characteristic between groups.
| Variables | EUS-BDeraN=30 | Non-EUS-BDeraN=94 | p-value |
|---|
| Age (year), Mean±SD | 62.0 (±11.2) | 64.5 (±11.3) | 0.290 |
| Gender, n (%) |
| Female | 12 (40) | 36 (38) | 1 |
| Male | 18 (60) | 58 (62) | |
| Diagnosis, n (%) |
| CCA | 29 (97) | 94 (100) | 0.240 |
| CA head of pancreas | 1 (3) | 0 (0) | |
| History of ERCP | 26 (87) | 94 (100) | 0.003 |
| History of PTBD | 12 (40) | 33 (35) | 0.391 |
| Plastic stent used | 13 (43) | 23 (24) | 0.042 |
| Metallic stent used | 29 (97) | 43 (46) | <0.001 |
| Follow-up time (months), Median (IQR) | 7.12 (3.33-11.87) | 2.43 (1.07-7.97) | <0.001 |
EUS-BD: Endoscopic ultrasound guided biliary drainage; SD: Standard deviation; IQR: Interquartile range; CA: Cancer; ERCP: Endoscopic retrograde cholangio-pancreatography; PTBD: Percutaneous transhepatic biliary drainage; IQR: Inter quartile range; Fisher’s-exact test was used to compare categorical variables between groups and the Student’s t-test was used to compare continuous variables
Due to imbalance of follow-up time between groups, this study used the median follow-up time between two groups for analysis. The restricted mean difference at 12 months in group I was 6.70 person-months (IQR:5.30-8.11) and group II was 4.47 person-months (IQR:3.63-5.32). The OS rate of group II was significantly higher than group II (mean difference=2.23; 95%CI: 0.54-3.92; p=0.010). The parametric-Cox proportional hazard model showed that the 1-year mortality of patients in group I were 63% less than those in group II (HR=0.37; 95%CI:0.14-0.97; p=0.043) [Table/Fig-2]. However, the OS using Kaplan-Meier curve with log rank test showed no significant difference in the occurrence of mortality rates (p=0.168) [Table/Fig-3].
Parametric survival and restricted mean difference at 12 months adjusted by age, gender, PTBD used, plastic stent used and metallic stent.
| Variables | Hazard ratio | 95% CI | p-value |
|---|
| EUS-BD era over non-EUS-BD era group | 0.37 | 0.14-0.97 | 0.043 |
| Variables (at follow-up time 12 months) | Median survival time (months) | 95% CI | p-value |
| Group 1 | 4.47 | 3.63-5.32 | <0.001 |
| Group 2 | 6.70 | 5.30-8.11 | <0.001 |
| Restricted mean difference at 12 months | 2.23 | 0.54-3.92 | 0.010 |
EUS-BD: Endoscopic ultrasound guided biliary drainage; PTBD: Percutaneous transhepatic biliary drainage; CI: Confidence interval
Kaplan-Meier curve of overall mortality comparing between non EUS-BD era and EUS-BD era comparing between Kaplan-Meier and parametric model.
Kaplan-Meier model, p=0.168 analysed by log rank test; Parametric model, p=0.043
Discussion
The cause of MBO may originate from CCA, pancreatic cancer, gallbladder cancer or metastatic cancer. In Thailand, most common cause of MBO is CCA. Because of the delay in diagnosis, patients usually come with unresectable stage, so palliative care of these patients, especially biliary drainage, play a major role in patient care. In this study, authors evaluated the emerging of EUS-BD effect to the result of treatment in MBO patients. Sangchan A et al., reported median survival time of patients who were performed ERCP with metallic stent and plastic stent of 126 days and 49 days, respectively [2], while this study reported longer median survival time of those patients performed EUS-BD and non-EUS-BD at 4.47 and 6.70 months, respectively. Park DH et al., study reported EUS-BD in MBO with mean survival in the patients using the covered and uncovered type wall stent were 209 days (range, 2-667) and 207.2 days (range, 2-935) days respectively [20].
The well-established main therapeutic procedure of MBO is ERCP, when the curative surgery is not possible [21,22]. The EUS-BD has previously been used as a rescue option when the ERCP was failed [11,14,23]. Several previous studies investigated the efficacy of ERCP versus EUS-BD showing some different results [11,12,14,23].
The main results from this cohort study showed longer median survival time of the non-EUS era patients (2.23 person-months; 95%CI: 0.54-3.92) with 63% less mortality when compared with those in EUS era. The OS of EUS in this study appeared close to the patients who received Self-Expandable Metal Stent (SEMS) of a previous study in Thailand [2] and a recent meta-analysis study [10] which reported that EBD was superior OS rate than PTBD in the resectable extrahepatic CCA with biliary obstruction patients (HR=0.76; 95%CI:0.59-0.84; p=0.002). A meta-analysis study by Jin Z et al., reported that EUS-BD and ERCP have similar OS for primary palliation of distal MBO [15]. However, there were significant differences of regional, countries and other prognostic factors among different studies [24].
Sarkaria S et al., reported that EUS-BD has several advantages over both TPBD and other surgical procedures [24]. The EUS-BD provides internal drainage which improves the patients’ QOL, that oppose to external biliary drain by PTBD. In addition, the benefit of EUS-BD is the avoidance of papillary manipulation which may reduce the complication, such as pancreatitis [14,25].
Contrast to this study, Puga M et al., reported that the ERCP patients with transpapillary stent had significant longer OS than those with EUS-guided stents [Table/Fig-4] [17]. The explanation might be the result of the stent design. The transpapillary stent has a tubular designed shape that might be more physiological drainage, whereas the majority of transmural EUS-BD stents are Lumen-Apposing Metal Stent (LAMS), with design less analogous to anatomy and causes possible occlusion risk.
Overall survival of EUS-BD versus non EUS-BD from published literature.
| Variables | Hazard ratio | 95% CI | p-value |
|---|
| EUS-BD era over non EUS-BD era group (Present study) | 0.37 | 0.14-0.97 | 0.043 |
| EUS-BD over PTBD group [10] | 0.70 | 0.59-0.84 | 0.002 |
| EUS similar to ERCP [15] | 1.00 | 0.66-1.51 | 0.860 |
| Follow-up time [2,17] | Median survival time (months/day) | 95% CI | p-value(mean difference) |
| Present study |
| Non-EUS-BD era | 4.47 | 3.63-5.32 | <0.001 |
| EUS-BD era | 6.70 | 5.30-8.11 | <0.001 |
| Sangchan A et al., [2] |
| EUS-BD with SEMS | 5.13 | 3.58-6.63 | 0.002 |
| EUS-BD with plastic stent | 1.44 | 0.63-2.87 | |
| Puka M et al., [17] |
| ERCP | 250 | 131-403 | 0.007 |
| EUS-BD | 67 | 24.55-91.48 | |
SEMS: Self-expanding metal stent
The OS outcome using KM methods with log rank test in this study showed no significant differences in the occurrence of mortality rates between two groups. The explanation might be due to this limited number of patients in EUS group. Therefore, a prospective larger sample size study is recommended for further investigation.
Limitation(s)
The present study had retrospective nature of data collection, the imbalance of follow-up time between group, and small number of patients in EUS era. There may be some selection biases or other confounders by indication which were not recorded in hospital medical records. Small sample size affected the comparative OS by log rank test which might be due to the low power of test.
Conclusion(s)
From this study, the EUS-BD had better one year OS rates in the MBO patients when compared with conventional methods. However, for conclusive finding, increasing both numbers of subjects and follow-up time in EUS-BD with a multicentre Randomised Control Trial should be considered.
EUS-BD: Endoscopic ultrasound guided biliary drainage; SD: Standard deviation; IQR: Interquartile range; CA: Cancer; ERCP: Endoscopic retrograde cholangio-pancreatography; PTBD: Percutaneous transhepatic biliary drainage; IQR: Inter quartile range; Fisher’s-exact test was used to compare categorical variables between groups and the Student’s t-test was used to compare continuous variables
EUS-BD: Endoscopic ultrasound guided biliary drainage; PTBD: Percutaneous transhepatic biliary drainage; CI: Confidence interval
SEMS: Self-expanding metal stent