Sciatic Nerve and Lumbar Plexus Block for Below Knee Amputation- Newer Approach for Better Haemodynamic Stability and Patient Safety
Jigisha Bharatbhai Mehta1, Ganesh Naik2, Dinesh Chauhan3
1 Assistant Professor, Department of Anaesthesia, Smt. B.K. Shah Medical Institute and Research Center, Sumandeep Vidyapeeth an Institute Deemed to be University, Vadodara, Gujarat, India.
2 Second Year Resident, Department of Anaesthesia, Smt. B.K. Shah Medical Institute and Research Center, Sumandeep Vidyapeeth an Institute Deemed to be University, Vadodara, Gujarat, India.
3 Professor and Head, Department of Anaesthesia, Smt. B.K. Shah Medical Institute and Research Center, Sumandeep Vidyapeeth an Institute Deemed to be University, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jigisha Bharatbhai Mehta, B/192, Swaminarayan Nagar Society, Nizampura, Vadodara-390024, Gujarat, India.
E-mail: jbmehta.28@gmail.com
Patients undergoing lower extremity amputation may have multiple co-morbid conditions like diabetes, cardiovascular, hepatic and renal disorders and are at risk of perioperative mortality and morbidity. Peripheral nerve blocks are associated with minimal haemodynamic changes, improved regional blood flow and are ideal for high risk patients who cannot tolerate slightest attenuation in haemodynamic response. The present report is of a 50-year-old female patient admitted for below knee amputation surgery. Sciatic nerve and lumbar plexus block were the mode of anaesthesia. It was found that regional anaesthesia in the form of nerve block provided adequate anaesthesia and analgesia, provided greater haemodynamic stability and patient safety.
Amputation surgery, High risk surgeries, Regional anaesthesia, Sciatic nerve block
Case Report
A 50-year-old female patient, weighing 60 kilograms, had complaint of pain and swelling in the right foot since morning. She was diabetic and hypertensive for two years and was on regular medications for the same. She had pain and swelling in right leg since one month which aggravated five days back. Right common femoral embolectomy for right femoral artery thrombosis was done three days back under local anaesthesia. Patient received two doses of Inj. Heparin 5000IU and 2500IU subcutaneously. Patient still complained of pain and swelling in right leg, fever since two days, not relieved by medication and was planned for below knee amputation. Preoperative evaluation of the patient showed hypotension and she had reduced air entry in both lower lobes. Procedure was explained and written consent was obtained under American Society of Anaesthesiology (ASA) grade IIIE. Patients was taken inside operation theatre and 20 G vein flow secured in the right upper limb and I.V fluid Inj. Ringer lactate 500 mL was started. Multipara patient monitor was attached to the patient, vitals were recorded and premedications were given. Under all aseptic conditions, 50 mL local anaesthetic solution (20 mL lignocaine with adrenaline+20 mL bupivacaine +10 mL normal saline) was kept ready. Then sciatic nerve block and lumbar plexus block were performed as follows:
Sciatic Nerve Block
Position: Lateral with the leg to be blocked upward and rolled forward. Heel of the operating leg rest on the knee of non-operative leg (modified sims position) [1].
Landmark: A line was drawn from posterior superior iliac spine to greater trochanter of the femur. A perpendicular line was drawn dividing the first line in two equal parts and extending 5 cm caudal. A second line was drawn from the greater trochanter to sacral hiatus. The crossing point of this line with the perpendicular line indicated the point of needle entry and falls 3-5 cm along the line [Table/Fig-1,2].
Showing sciatic nerve block being performed.

Landmark drawn for lumbar plexus and sciatic nerve block.

Procedure: Insulated 10 cm needle was inserted perpendicular to skin entry point and advanced further till motor response was elicited. Stimulation of the tibial nerve component produces planter flexion and inversion of foot. Common peroneal nerve stimulation produces dorsiflexion and eversion of foot. Stimulation of larger tibial nerve is preferred. After obtaining stimulation at 0.6 mA and disappearance at 0.4 mA, 20 mL of local anaesthetic mixture was given.
Lumbar Plexus Block
Position: Patient was placed in lateral position with hip flex and operative extremity uppermost.
Landmark:
Line 1- Vertical line connecting spinous processes of lumbar vertebrae.
Line 2- Parallel to line1 passing from posterior superior iliac spine.
Line 3- Passing from iliac crests (intercostals line).
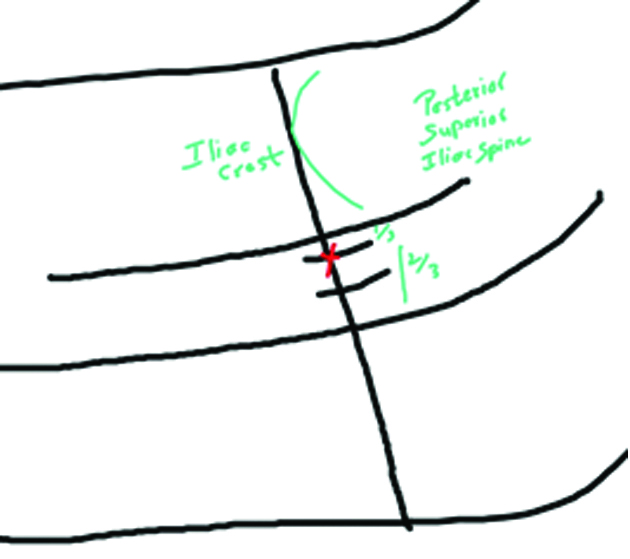
Needle entry point: Part of the line 3 between line 1 and 2 was divided in 3 parts and needle was inserted at the junction of lateral 1/3rd and medial 2/3rd [Table/Fig-2,3].
Landmark for lumbar plexus block. Red cross mark indicates point of insertion of needle.
Procedure: A 10 cm insulated needle was advanced perpendicular to skin entry site until it contacted the 5th lumbar transverse process. The needle was redirected cephalict ill the end of transverse process. The lumbar plexus was identified by elicitation of quadriceps motor response and after negative aspiration 30 mL of local anaesthetic was injected.
Complete anaesthesia was achieved in 22 minutes after the blocks. Intraoperative vitals were recorded throughout surgery and surgery completed without any complication. Patient required no additional sedation or analgesia. She had total recovery of motor functions and sensory function without any complication after eight hours. She was followed-up for identification of complications and was discharged on 7th postoperative day.
Discussion
The neuraxial anaesthesia in the form of subarachnoid block has been considered the gold standard for lower extremity surgeries [1]. However, it is not safe to perform neuraxial blocks on high risk patients with deranged coagulation profile [2]. Most common problem associated with neuraxial anaesthesia (mainly spinal anaesthesia and less with epidural anaesthesia) is sympathetic blockade leading to hypotension which is better tolerated by young, healthy patients without co-morbidities, but elderly patients or patients with multiple co-morbidities cannot tolerate hypotension. Peripheral nerve blocks avoid sympathectomy associated with neuraxial blocks and therefore are advantageous when shift in haemodynamic could be deleterious. In addition, when patients have coagulation disorders or on anticoagulants neuraxial block cannot be given due to risk of haematoma formation and spinal cord compression but peripheral nerve blocks can be given without risk.
Based on a trial done by Rodgers A et al., which included 141 trials covering 9559 patients neuraxial anaesthesia reduced mortality by one third as compared to mortality by general anaesthesia [3]. Peripheral neuraxial block give greater haemodynamic stability than any other anaesthetic techniques [4]. In this case, recommended peripheral neuraxial block was lumbar plexus block along with sciatic nerve block. The lumbar plexus blockade blocks the femoral, obturator and lateral femoral cutaneous nerve.
At present, ultrasound guided nerve block is being widely used for achieving successful nerve blocks [5]. Usage of ultrasound guidance helps in the visualisation of nerves and distribution of local anaesthetics. It improves the success rate and requires lower volume of drug to attain the desired nerve block and prevents Local Anaesthetic Systemic Toxicity (LAST) [6-8]. In contrast to the ultrasound guided technique, peripheral nerve block with aid of Peripheral Nerve Stimulator (PNS) relies on landmark identification and physiological response of nerve stimulation and provides comparable efficacy in attaining adequate regional anaesthesia with comparable side effects as with ultrasound guided technique. Anaesthetists must be trained for achieving regional blocks without ultrasound guidance which is very useful where facilities are less or unavailable in the time of need [9,10]. Diwan S et al., reported a case series on combined lumbar and sacral plexus block in geriatric high risk patients undergoing repair of inter trochenteric femur fracture [11]. They concluded that combine lumbar and sacral plexus block provides a unique, unilateral and uncomplicated regional anaesthesia for the high risk geriatric patients posted for hip surgeries. Penafrancia Catangui C in a case report of a 64-year-old diabetic female with multiple co-morbidities posted for knee amputation showed similar benefit of peripheral nerve block in the form of haemodynamic stability and lower postoperative analgesics requirement [12].
Conclusion(s)
Peripheral nerve blocks for lower extremities must be considered in high risk patients. It provides better haemodynamic stability compared to central neuraxial block and avoid other risks related to general anaesthesia. This case study showed that successful peripheral neuraxial blockade could reliably provide stable haemodynamic, along with adequate anaesthesia and analgesia throughout the operation. The patient also required lower analgesic dose in the postoperative period and no postoperative side effects were seen.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 30, 2020
Manual Googling: Jan 09, 2021
iThenticate Software: Feb 17, 2021 (16%)
[1]. Memtsoudis SG, Sun X, Chiu YL, Stundner O, Liu SS, Banerjee S, Perioperative comparative effectiveness of anaesthetic technique in orthopedic patientsThe Journal of the American Society of Anaesthesiologists 2013 118(5):1046-58.10.1097/ALN.0b013e318286061d23612126 [Google Scholar] [CrossRef] [PubMed]
[2]. Horlocker TT, Regional anaesthesia in the patient receiving antithrombotic and antiplatelet therapyBritish Journal of Anaesthesia 2011 107(suppl 1):i96-106.10.1093/bja/aer38122156275 [Google Scholar] [CrossRef] [PubMed]
[3]. Rodgers A, Walker N, Schug S, McKee A, Kehlet H, Van Zundert A, Reduction of postoperative mortality and morbidity with epidural or spinal anaesthesia: Results from overview of randomised trialsBMJ 2000 321(7275):149310.1136/bmj.321.7275.149311118174 [Google Scholar] [CrossRef] [PubMed]
[4]. Yazigi A, Madi-Gebara S, Haddad F, Hayeck G, Tabet G, Intraoperative myocardial ischemia in peripheral vascular surgery: General anaesthesia vs combined sciatic and femoral nerve blocksJournal of Clinical Anaesthesia 2005 17(7):499-503.10.1016/j.jclinane.2004.11.00616297748 [Google Scholar] [CrossRef] [PubMed]
[5]. Clendenen SR, Robards CB, The role of ultrasound and regional anaesthesiaInternational Anaesthesiology Clinics 2010 48(4):13-20.10.1097/AIA.0b013e3181f89b8120881523 [Google Scholar] [CrossRef] [PubMed]
[6]. Marhofer P, Harrop-Griffiths W, Kettner SC, Kirchmair L, Fifteen years of ultrasound guidance in regional anaesthesia: Part 1British Journal of Anaesthesia 2010 104(5):538-46.10.1093/bja/aeq06920364022 [Google Scholar] [CrossRef] [PubMed]
[7]. Griffin J, Nicholls B, Ultrasound in regional anaesthesiaAnaesthesia 2010 65:01-02.10.1111/j.1365-2044.2009.06200.x20377542 [Google Scholar] [CrossRef] [PubMed]
[8]. Abrahams MS, Aziz MF, Fu RF, Horn JL, Ultrasound guidance compared with electrical neurostimulation for peripheral nerve block: A systematic review and meta-analysis of randomized controlled trialsBritish Journal of Anaesthesia 2009 102(3):408-17.10.1093/bja/aen38419174373 [Google Scholar] [CrossRef] [PubMed]
[9]. Tsui B, Ultrasound-guidance and nerve stimulation: Implications for the future practice of regional anaesthesiaCanadian Journal of Anaesthesia 2007 54(3):16510.1007/BF0302263517331926 [Google Scholar] [CrossRef] [PubMed]
[10]. Tornero CT, Font LA, Training on regional anaesthesia- From neurostimulation to ultrasoundTechniques in Regional Anaesthesia and Pain Management 2012 16(3):131-35.10.1053/j.trap.2013.03.003 [Google Scholar] [CrossRef]
[11]. Diwan S, Pradhan C, Patil A, Puram C, Sancheti P, Combined lumbar and sacral plexus block in geriatric high-risk patients undergoing an awake repair of fracture intertrochanteric of femurJournal of Anaesthesia and Critical Care Case Reports 2018 4(1):21-30. [Google Scholar]
[12]. Penafrancia Catangui C, Nerve stimulator guided lumbar plexus and parasacral sciatic nerve block for above knee amputation in a high-risk patient: A case reportJournal of Clinical Anaesthesia and Pain Management 2020 4(1):101-13.10.36959/377/339 [Google Scholar] [CrossRef]