Introduction
Whilst uncommon, acetabular roof defects are often seen on imaging and considered normal variants, therefore not always reported or commented on. They are often considered incidental to the symptoms which triggered the original imaging referral. Supra-Acetabular Fossa (SAF) can be classified into two types; Type I- Accessory bony fossa in the roof of the acetabulum which is separate from the acetabular fossa and fills with contrast on Magnetic Resonance (MR) arthrogram, and Type II- Accessory bony fossa without contrast filling on MR arthrogram, with the defect lined in cartilage [1].
Here, authors describe five cases with consistent radiological appearances of a defect in the roof of the acetabulum on Magnetic Resonance Imaging (MRI) scan. In each case hip pain was a predominant feature on presentation, of long duration, and sufficiently severe to trigger referral to tertiary services. In the majority of cases, there was no alternate pathology on MRI to explain the symptoms.
Case Series
Case 1
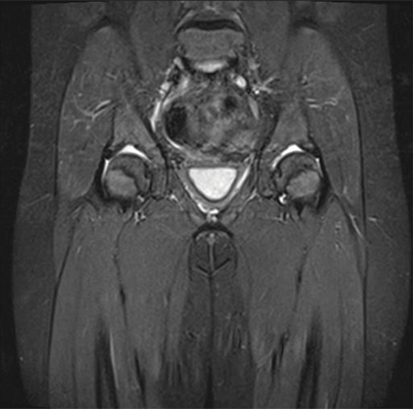
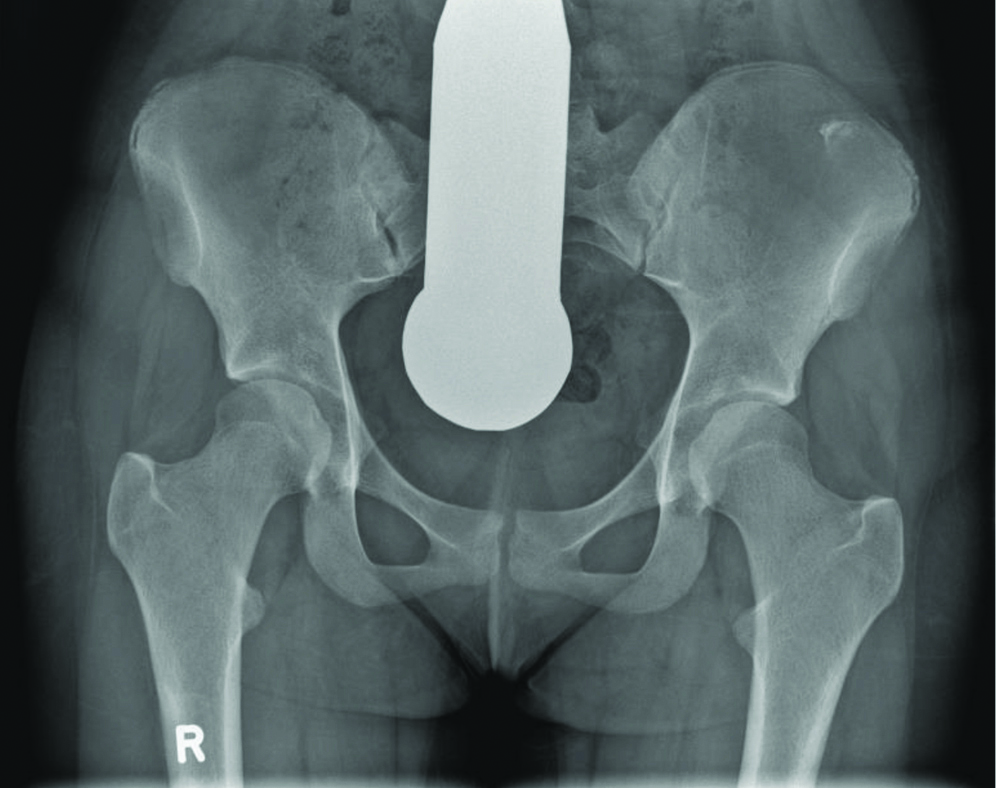
A 14-year-old boy presented with a six month history of a “groin strain” that did not settle with conservative management. He was otherwise fit and well, and a keen sportsman. Clinical examination was normal with full bilateral hip Range of Motion (ROM). Imaging obtained at the time demonstrated bilateral acetabular roof defects, lined with cartilage in keeping with a Type II defect [Table/Fig-1,2 and 3].
| Cases | Right | Left | Interventions and follow-up |
|---|
| 1 | MR Acetabular roof defect | MR 5 mm Acetabular roof defect | Physiotherapy with resolution of symptoms |
| 2 | X-ray Acetabular roof irregularity MR Symmetrical superior anterior acetabular pits, devoid of cartilage | X-ray Acetabular roof irregularity MR Symmetrical superior anterior acetabular pits, devoid of cartilage | No orthopaedic follow-up noted |
| 3 | MR Small bilateral acetabular roof defects, confirmed on MR arthrogram | MR Small bilateral acetabular roof defects, confirmed on MR arthrogram | 6 month follow-up |
| 4 | MR Bilateral acetabular roof defects. | MR Bilateral acetabular roof defects. | No orthopaedic follow-up noted |
| 5 | X-ray Deep sockets bilaterallyMR Possible right labral tear, cartilage filled acetabular roof defect | X-ray Deep sockets bilaterallyMR cartilage filled acetabular roof defect | Planned left hip arthrogram |
MR: Magnetic resonance
AP Plain-film radiograph of the pelvis demonstrating bilateral acetabular roof defects.
AP: Antero-posterior

Coronal T1W non-contrast both hips demonstrating bilateral acetabular roof defects lined with cartilage (Type II).

Following a course of physiotherapy (core exercises and targeted hip exercises), his symptoms completely resolved. No further imaging was obtained to establish the evolution of the acetabular roof defects.
Case 2
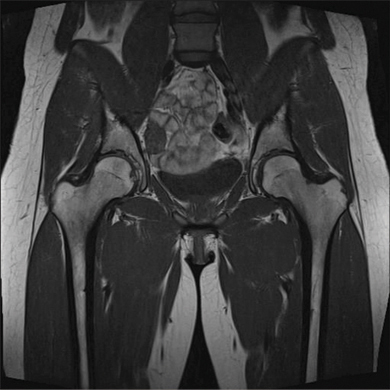
A nine-year-old girl with Down’s syndrome presented with episodic nocturnal pain in her left hip and groin, which did not respond to simple analgesia. She also had swelling of her left ankle. Clinical examination was normal with full ROM in both hips. X-ray demonstrated bilateral acetabular roof irregularities. An MRI revealed bilateral acetabular roof defects devoid of cartilage; Type I [Table/Fig-1,4]. No further orthopaedic intervention was required.
Coronal T2W Fat Sat non-contrast both hips demonstrating bilateral acetabular roof defects devoid of cartilage (Type I).
Case 3
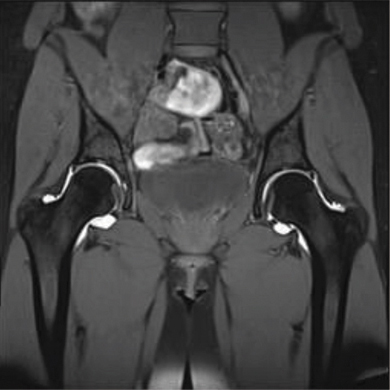
A 17-year-old girl presented with significant bilateral hip pain of two year duration. Her pain was variable in intensity, affecting the anterior aspect of her both hips and radiating round to the buttock, restricting her activities. She avoided physical education and required regular analgesia. She denied any history of trauma and she was otherwise fit and well. Clinical examination revealed a normal gait, full ROM to both hips but painful at extremes of movement. MRI obtained at the time, demonstrated small bilateral acetabular roof defects, Type II [Table/Fig-1,5].
Coronal T1W non-contrast both hips demonstrating small bilateral acetabular roof defects (Type II).
An MRI arthrogram, six months later [Table/Fig-6], showed quite small central acetabular roof defects with a tiny subarticular cyst on the posterior aspect of the head/neck junction on the left side, not requiring any treatment. She was walking normally and managing well with simple analgesia.
Coronal MR arthrogram demonstrating small bilateral acetabular roof defects, not contrast filled (Type II).
Case 4
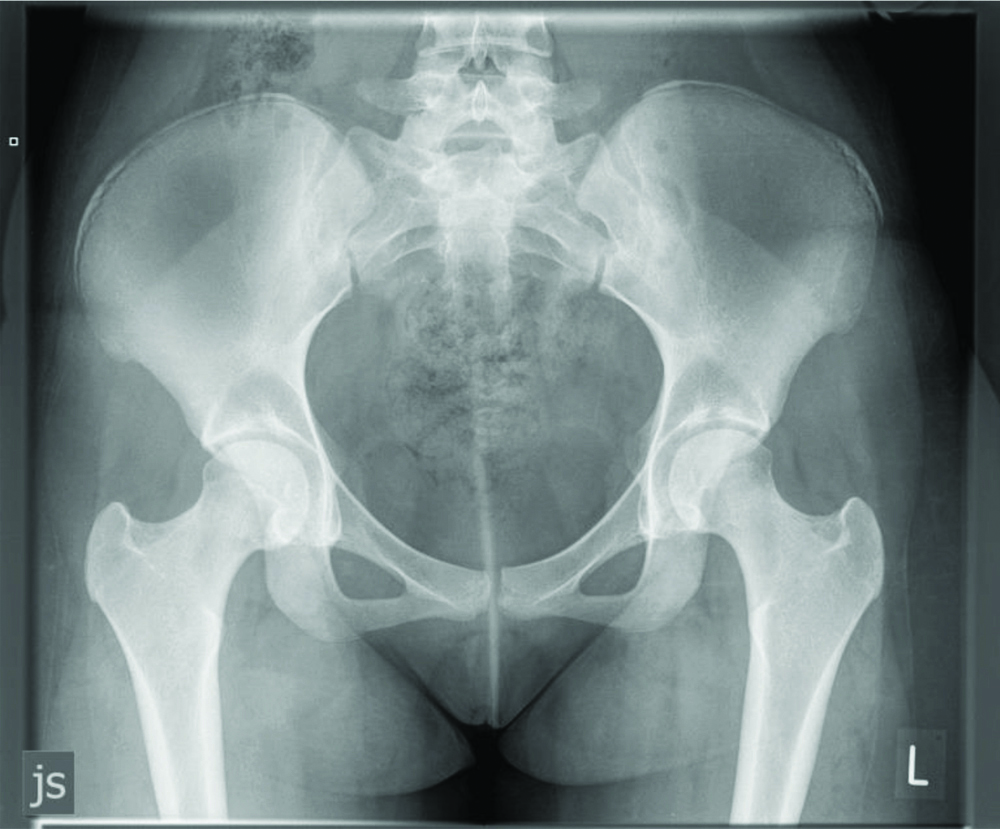
A 12-year-old girl presented with exertional pain, although no clear pattern. Clinical examination was normal. No further orthopaedic intervention was noted following MR demonstrating bilateral acetabular roof defects, which were devoid of cartilage (Type I). Subsequent X-ray imaging, obtained over the period of 2 years, showed no further abnormality other than the bilateral acetabular roof defects, although over time, the defects appear to reduce in size with sclerosis present [Table/Fig-1,7,8].
AP Plain-film radiograph of the pelvis demonstrating bilateral acetabular roof defects.
AP: Antero-posterior
AP Plain-film radiograph of the pelvis demonstrating bilateral acetabular roof defects, now with evidence of sclerosis.
AP: Antero-posterior
Case 5
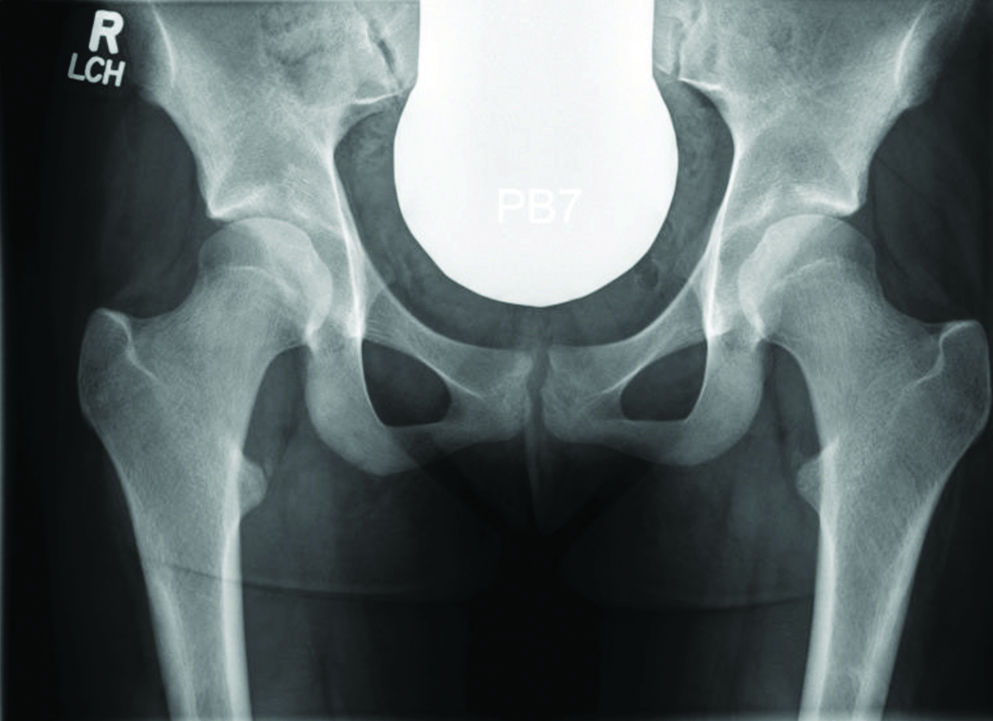
A 14-year-old girl was referred with a one year history of bilateral worsening hip pain, the right being worse. Physiotherapy gave little benefit. Her mother had a congenital hip problem. X-ray demonstrated bilateral acetabular roof defects [Table/Fig-1,9].
AP Plain-film radiograph of the pelvis demonstrating bilateral acetabular roof defects.
AP: Antero-posterior
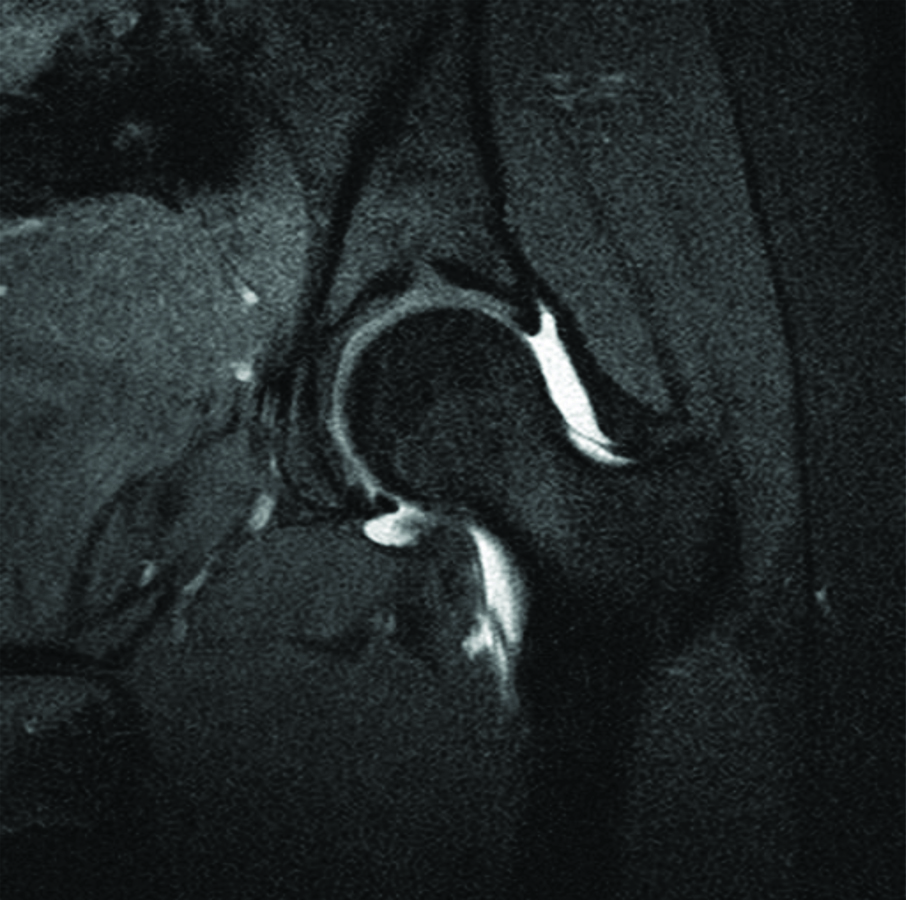
On examination, she had bilateral positive impingement sign with the left being at the 12 o’clock position and the right around the 10:30 position. She was referred for a left hip arthrogram, years years later, due to worse pain on the left and previous imaging findings of possible labral tear. Subsequent MR arthrogram of the left hip found no labral tear, although it did confirm a cartilage filled central acetabular roof defect, Type II [Table/Fig-10]. She was referred for an Ultra sonography guided local anaesthetic injection for symptomatic relief.
Coronal MR arthrogram of the left hip demonstrating cartilage lined acetabular roof defect (Type II).
For the five cases studied, mean age at first presentation was 13.2 years (range 9-14 years). Four patients were female. Two patients had a Type I defect and three patients had a Type II acetabular roof defect.
Discussion
Although these lesions have been described previously, they have not been associated with clinical symptoms and, as such, have been labelled benign normal anatomical variants.
Several studies clearly describe similar radiological appearances [1-4]. Each author has used slightly different descriptive terminology, but the appearances are consistent. There are general classifications of defect; stellate crease, superior acetabular notch, and supra-acetabular fossa. Johnstone W et al., reported these defects in 1982, and did not find a direct cause of these findings [2]. The authors compared specimens with imaging and found that the acetabular accessory fossa was determined to be an anatomical variant.
Mafart B reported a variant from their study on samples from historical population (hip bones from historical burial site) [3]. They described an anterosuperior linear crease on the surface of the acetabulum. It appears to be a stable anatomical trait with no predominant side and no correlation with sex. No specific dysplastic or degenerative acetabular lesions were found in association. Durur-Subasi I et al., also briefly mention SAF as a benign normal variant among other major joint osteochondral lesions [4].
Dietrich T et al., evaluated the frequency of the SAF (pseudo defect of acetabular cartilage) at MR arthrography of the hip and compared the MR findings with those from arthroscopy [1]. This study is frequently cited by authors describing SAF. Variants of the acetabular roof are described in the literature as mimickers of acetabular cartilage defects. SAF are usually located in the acetabular roof near the 12 o’clock position in coronal and sagittal imaging planes of MRI. Stellate crease, an area deficient of hyaline cartilage located above the acetabular notch, in continuity with the notch, is also seen. The SAF addressed in the study is completely separate from the acetabular notch. A popular online radiology resource describes these as normal variants and therefore not to be confused with pathology [5].
Dietrich T et al., found SAF Type I is more common in younger patients (average age 20.1 years) and therefore, assume some remodelling with time to SAF type II [6]. Although there was a high frequency of SAF on MR arthrogram (10%), only a small proportion of defects were found to be Type I (1.6%). Their conclusion was that the absence of subchondral reaction and the absence of cartilage defects at arthroscopy implied that SAF represented a variant. The authors state that SAF should not be interpreted as a cartilage defect or as an osteochondral lesion at MR arthrography. The study does not give the indication for the MR arthrograms analysed, and therefore it may be assumed that the patients were, in fact, symptomatic. Fortun C et al., agreed with Dietrich T et al., in that without subchondral reaction or cartilage defect the SAF should be considered a normal variant [6,7]. Boutris N et al., also studied the prevalence of SAF in patients presenting with hip pain [8]. They found a prevalence of 12.6% and also that a Type I was found in a younger population than a Type II. Once again, it is stated that this should not be confused with an osteochondral defect and therefore the cause for the patient’s symptoms.
Although Agten C et al., describe SAF as a normal variant to be excluded, they detail an 18-year-old with hip pain who was found to have a Type 1 defect which is shown to be filled in after follow-up imaging [9]. Nguyen M et al., also describes SAF in a 15-year-old, with absence of cartilage defect and normal bone marrow signal [10]. Both of these articles use cases from a younger population, and therefore supports the conclusion that this is more prevalent in this age group. It is not stated in either why the patients presented for MR imaging and therefore, may have been symptomatic.
This case series agreed with Dietrich T et al., with both type I and type II defects present on MRI and MR arthrogram [1,6]. We also found that patients with Type I were younger, age 9-12 years compared with age 14-17 years, although not statistically significant in this small sample size. We found it unclear if SAF contributes to clinical symptoms of the hip or if it represents an incidental finding without clinical relevance. Patients often undergo further diagnostic investigations to evaluate symptomatic benefit or physiotherapy with and without benefit. SAF was found to evolve over time with subsequent sclerotic change in this study. Without another explanation for the cause of hip pain, or resolution of symptoms following orthopaedic intervention, the SAF should be considered as the cause of pain. Whilst the literature supports SAF as an anatomical normal variant, there is no evidence to conclusively define these as asymptomatic. Many of the studies are retrospective and review patients who have already presented with hip pain.
It is not possible to formulate an effective treatment plan for these patients until the natural history is more clearly defined. It may be that symptoms do not resolve until fully evolved into a Type II SAF, where the development of cartilage resolves the defect. Our case series is retrospective and therefore, future studies would benefit from longer-term follow-up as symptoms resolve.
Conclusion(s)
Through this case series, author highlight the unusual anatomical feature to the paediatric orthopaedic and radiology community. An increased awareness may lead to further studies and research, that may help us to reassure these young people with problematic hip pain.
[1]. Dietrich T, Suter A, Pfirrmann C, Dora C, Fucentese S, Zanetti M, Supraacetabular Fossa (Pseudodefect of Acetabular Cartilage): Frequency at MR arthrography and comparison of findings at MR arthrography and arthroscopyRadiology 2012 263(2):484-91.10.1148/radiol.1211139722416250 [Google Scholar] [CrossRef] [PubMed]
[2]. Johnstone W, Keats T, Lee M, The anatomic basis for the superior acetabular roof notch? Superior acetabular notch?Skeletal Radiology 1982 8(1):25-27.10.1007/BF003613647079779 [Google Scholar] [CrossRef] [PubMed]
[3]. Mafart B, Description, significance and frequency of the acetabular crease of the hip boneInternational Journal of Osteoarchaeology 2005 15(3):208-15.10.1002/oa.770 [Google Scholar] [CrossRef]
[4]. Durur-Subasi I, Durur-Karakaya A, Yildirim O, Osteochondral lesions of major jointsThe Eurasian Journal of Medicine 2015 47(2):138-44.10.5152/eurasianjmed.2015.5026180500 [Google Scholar] [CrossRef] [PubMed]
[5]. Dixon A, Supra-acetabular fossa | Radiology Reference Article | Radiopaedia.org [Internet]Radiopaedia.org. 2020 [cited 16 December 2020]. Available from: https://radiopaedia.org/articles/supra-acetabular-fossa?lang=gb [Google Scholar]
[6]. Dietrich T, Suter A, Pfirrmann C, Dora C, Fucentese S, Zanetti M, Supraacetabular fossa (pseudo-defect of acetabular cartilage): Morphology at MR-arthrography and correlation with conventional radiographsSkeletal Radiology 2011 40(6):793-814.22416250 [Google Scholar] [PubMed]
[7]. Fortun C, Streit J, Patel S, Salata M, Cartilage defects in the hipOperative Techniques in Sports Medicine 2012 20(4):287-94.10.1053/j.otsm.2012.10.003 [Google Scholar] [CrossRef]
[8]. Boutris N, Gardner S, Yetter T, Delgado D, Pulido L, Harris J, MRI prevalence and characteristics of supraacetabular fossae in patients with hip painHIP International 2018 28(5):542-47.10.1177/112070001775256629756502 [Google Scholar] [CrossRef] [PubMed]
[9]. Agten C, Sutter R, Buck F, Pfirrmann C, Hip imaging in athletes: sports imaging seriesRadiology 2016 280(2):351-69.10.1148/radiol.201615134827429142 [Google Scholar] [CrossRef] [PubMed]
[10]. Nguyen M, Kheyfits V, Giordano B, Dieudonne G, Monu J, Hip anatomic variants that may mimic pathologic entities on MRI: Nonlabral variantsAmerican Journal of Roentgenology 2013 201(3):W401-08.10.2214/AJR.12.986123971471 [Google Scholar] [CrossRef] [PubMed]