A Rare Case of Malignant Transformation of Keratinous Cyst in Gluteal Region
BS Balapriya1, R Anantharamakrishnan2, K Senthil Kumar3, Femela Muniraj4, Vijayashree Raghavan5
1 Junior Resident, Department of General Surgery, CHRI/CARE, Chennai, Tamil Nadu, India.
2 Professor, Department of General Surgery, CHRI/CARE, Chennai, Tamil Nadu, India.
3 Professor, Department of General Surgery, CHRI/CARE, Chennai, Tamil Nadu, India.
4 Professor, Department of Pathology, CHRI/CARE, Chennai, Tamil Nadu, India.
5 Professor and Head, Department of Pathology, CHRI/CARE, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. K Senthil Kumar, No. 108(3/2)f 2, Sahana Flats, Sayee Nagar, 5th Street, Virugambakkam, Chennai-600092, Tamil Nadu, India.
E-mail: drsenthilchri@gmail.com
Keratinous cyst (Epidermoid cysts) is more common and frequently encountered. It is one of the commonest benign lesion. Malignant transformation of keratinous (epidermoid) cyst is very rare. Epidermal cyst is noted as non-malignant condition. Few cases have shown malignant transformation of keratinous cyst into Squamous Cell Carcinoma (SCC). Here, authors report a rare case of 49-year-old male who presented with long standing keratinous cyst in gluteal region which turned out as SCC 35 years after intial presentation of the leison, and here authors have discussed the clinicopathological features of this rare entity. Hence, any swelling which is long standing, showing sudden increase in size, progressing symptoms, more than 2 cm in diameter, cyst content seen as heterogenous pattern on imaging should be highly suspicious of malignancy.
Epidermoid cyst, Excision, Squamous cell carcinoma
Case Report
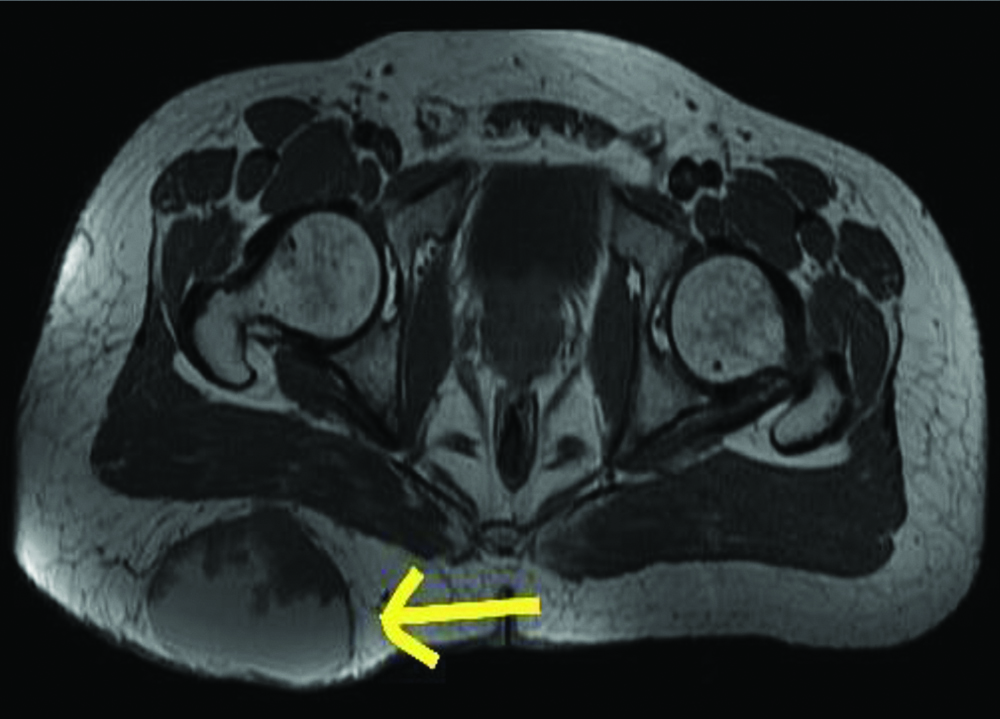
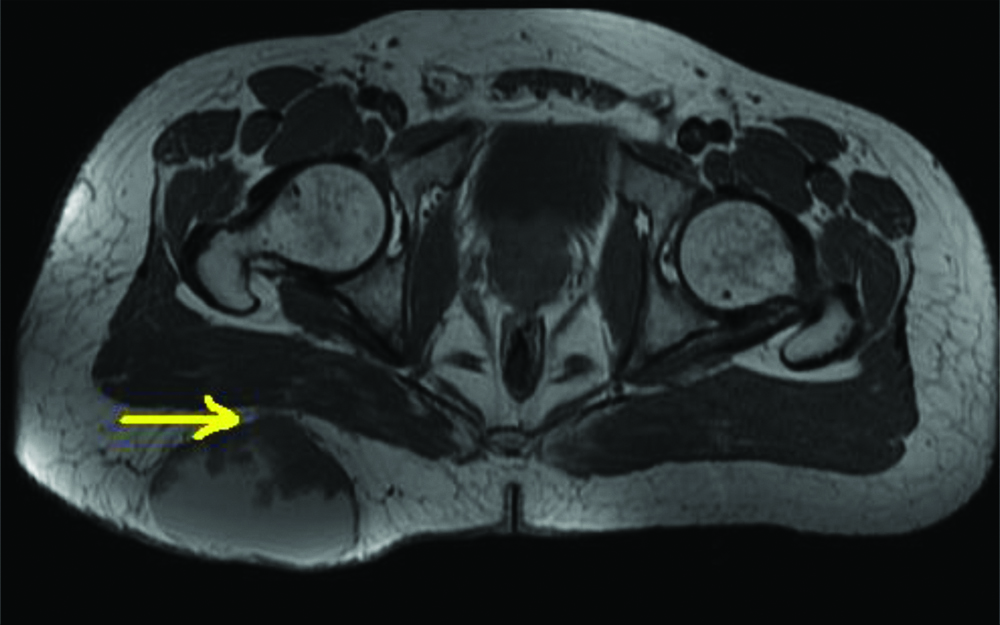
A 49-year-old male presented with a swelling on the right gluteal region. It started as a small swelling which progressively increased in size to attain the present size for the past 35 years duration. There was a sudden increase in size for the past one year. Patient had no pain, but had discomfort while sitting. Patient had no known morbidities and no history of previous surgeries. No history of trauma or aggravating factors. Clinical examination revealed a 10×10 cm, soft, cystic swelling in the right gluteal region [Table/Fig-1], which was non tender, non transilluminant with variable consistency and restricted mobility was noted. Overlying skin appeared stretched and shiny. Clinically, differential diagnosis of soft tissue swelling, chronic abscess was made out. Fine Needle Aspiration Cytology (FNAC) smear showed numerous anucleated squamous, cholesterol crystals, many degenerated cells on a proteinaceous background. Also, few viable squamous cells, macrophages, scattered brown black pigments were seen and advised excision biopsy. MRI gluteal region showed a well defined ovoid non-enhancing mixed intensity [Table/Fig-2] (predominantly fluid signal intensity) noted involving the subcutaneous fat plane, abutting the right gluteus maximus [Table/Fig-3]. No suppression of signal on Short Tau Inversion Recovery/Fast Spin Echo (STIR/FSE) was noted. No obvious infiltration of muscular plane was seen, which was highly suspicious of benign aetiology. A clinical diagnosis of right gluteal keratinous cyst was made.
Right gluteal soft tissue swelling.

MRI gluteal region showing soft tissue swelling in the right gluteal region with solid and cystic components.
MRI image showing involvement of subcutaneous fat plane, abutting the right gluteus maximus.
Operative Findings
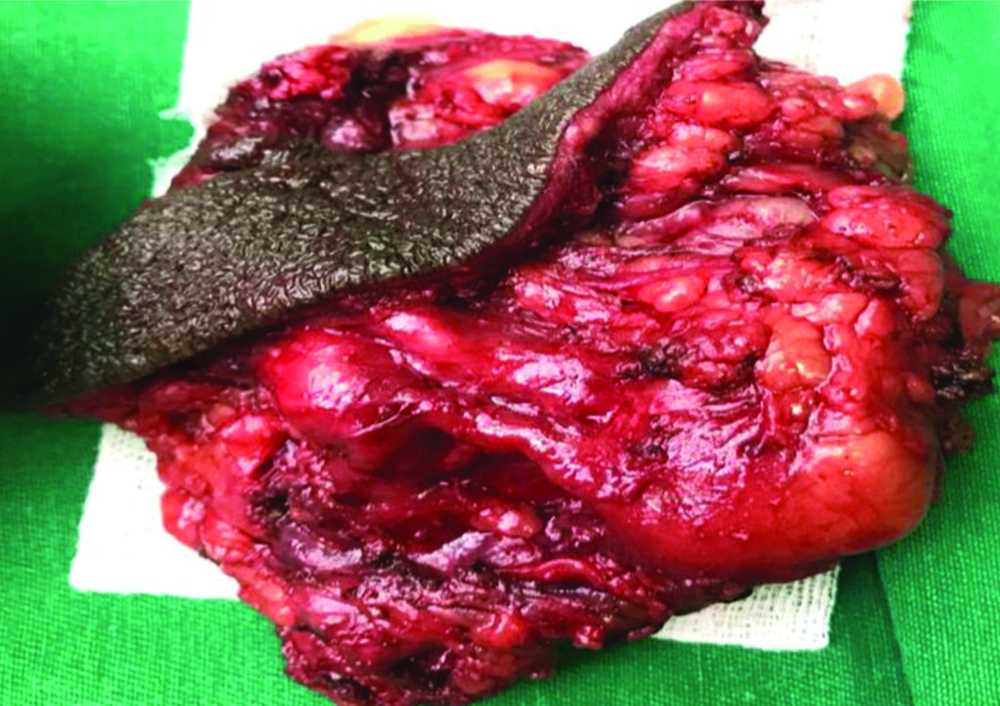
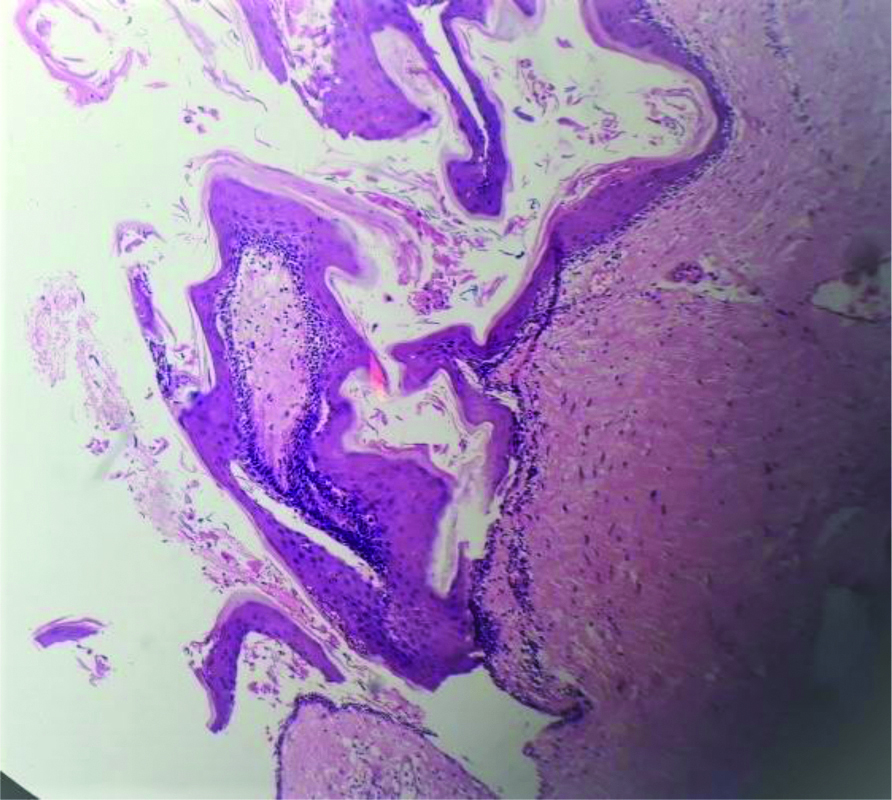
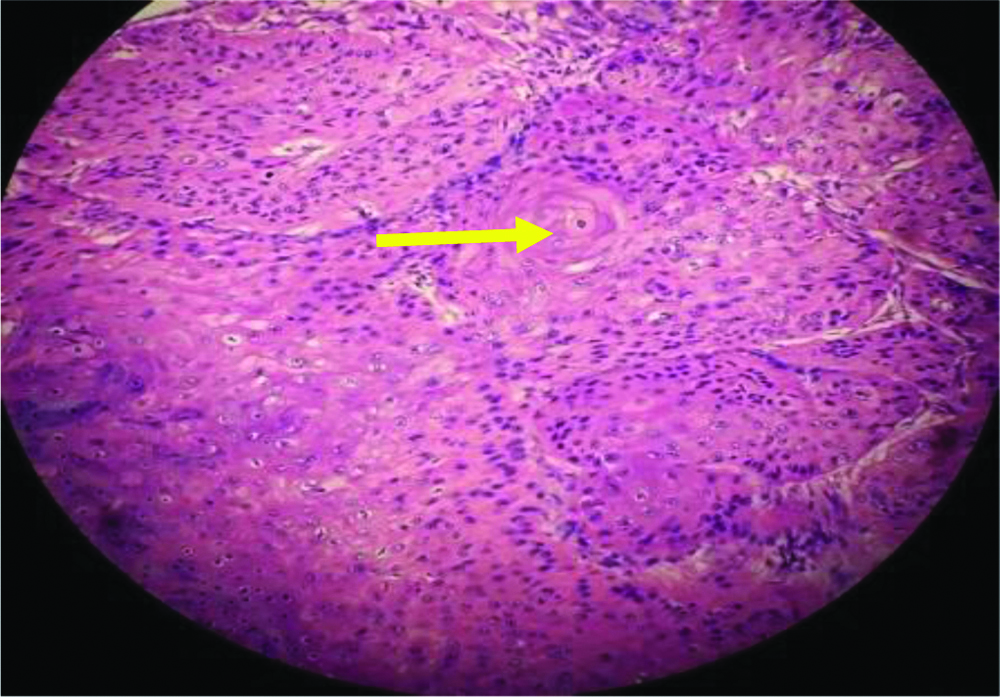
A cystic swelling of size 10×10 cm was noted, haemorrhagic fluids with few clots with necrotic material was noted as content. Swelling was found to be adherent to the deep fascia and few areas of adhesions noted over the gluteus maximus muscle fiber. After dissecting, the cyst wall was excised in totol along with the involved muscle and fascia [Table/Fig-4,5]. Specimen was sent for histopathology. Drain was kept and wound closed in layers. Postoperative period was uneventful. On inspecting the gross specimen the differential diagnosis of cavernous haemangioma was made out. But Histopathological Examination (HPE) showed solid nest of atypical squamous cells with marked pleomorphism, squamous eddies, keratin masses, keratin pearls invaginating into the dermis and subcutaneous fat. Few normal mitotic figures were seen. The deep dermis was lined by stratified squamous epithelium exhibiting focal dysplasia. All the margins were clear. Foreign body gaint cell reaction with intracellular pigment was seen adjacent to the tumour. The HPE report was concluded as Keratinous cyst [Table/Fig-6] with SCC-well differentiated type [Table/Fig-7]. Since the features were more in favour of SCC other diseases were ruled out. Patient was referred for further adjuvant therapy to medical oncologist.
Image showing swelling in the right gluteal region taken during dissection.

Postoperative image showing complete cyst wall along with fibro fatty tissue with surrounding skin.
Keratinous cyst lined by keratinous granular stratified squamous epithelium without any atypia. (Haematoxylin and Eosin stain, 4x magnification).
Microscopy showing atypical squamous cell, pleomorphism, keratin pearls suggestive of Sqamous Cell Carcinoma (SCC). (Haematoxylin and Eosin stain, 40x magnification).
Discussion
Keratinous cyst arising from skin are very frequent but the malignant transformation occurs occasionally [1,2]. Incidence ranges from 0.011-0.045% [3]. This type of malignant transformation is seen in 70% of male gender and between 20-80 years of age. Even keratinous cysts are more prevalent, changing into malignant picture like SCC is rare. Malignant transformation of keratinous cyst to SCC was reported commonly in head and neck region, compared to trunk [4]. Few cases reported with such kind of malignant transformation in the areas like scrotum, labia majora, and vulva [5]. Differential diagnosis for these type of cyst include soft tissue swelling, chronic abscess, trichilemmal proliferation cyst, pseudocarcinamatous hyperplasia, a cyst which has already ruptured. The clinical diagnosis of soft tissue swelling was ruled out, as the lesion was cystic microscopically and was keratinous in nature. There was no inflammation which ruled out the possibility of chronic abscess. The cyst was lined by stratified squamous epithelium with epidermal type keratinisation and hence trichilemmal proliferation cyst was ruled out. Malignant tumour was seen continuous with the keratinous cyst and there was no pseudocarcinomatous hyperplasia. The cyst was not a simple keratinous cyst and there was no rupture. The possible aetiology include human papilloma virus infection, skin exposed to Ultraviolet (UV) radiation [6]. This type of change in an epidermal cyst to SCC usually has low malignant potential for metastasis. However, metastasis was noted in three cases and death occurs in a period of 5 to 10 months [7]. Clinically, it is difficult to differentiate between a benign and malignant cystic lesion. It can be diagnosed using radiological imaging like ultrasound, MRI, and HPE. Few reported cases discuss the subtypes of SCCs arising from epidermal cysts. Thus, the clinical course, prognosis, approach, and optimal management of this disease entity are not well established. Sabhlok S et al., describes that lesion is usually of 5 cm in size if it is more than 5 cm it is known as gaint epidermal cyst [8]. In this case, the size was 15 cm and duration was 35 years, representing a lesion with the largest size and longest duration of all well documented case reports. Although it has been advocated that malignant transformation should be suspected in large epidermal cysts with rapid growth, ulceration or fistulas were not observed in index case. Novelty of this case highlights that all excised lesion should be subjected to histological examination and to yield the correct diagnosis [1]. This type of malignant transformation has poor prognosis [9].
Conclusion(s)
SCC arising in an epidermal cyst is rare. The clinical course, prognosis, approach and optimal management of this entity are not well established. Author would like to emphasise that all soft tissue lesion more than 5 cm with variable consistency and restricted mobility should undergo frozen section examination intraoperatively to decide the surgical clearance and further treatment.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 28, 2020
Manual Googling: Feb 03, 2021
iThenticate Software: Feb 06, 2021 (5%)
[1]. Faltaous AA, Leigh EC, Ray P, Wolbert TT, A rare transformation of epidermoid cyst into squamous cell carcinoma: A case report with literature reviewAm J Case Rep 2019 20:1141-43.10.12659/AJCR.91282831375657 [Google Scholar] [CrossRef] [PubMed]
[2]. Kshirsagar AY, Sulhyan SR, Deshpande S, Jagtap S, Malignant change in an epidermal cyst over gluteal regionJournal of Cutaneous and Aesthetic Surgery 2011 4(1):48-50.10.4103/0974-2077.7919521572684 [Google Scholar] [CrossRef] [PubMed]
[3]. Ziadi S, Trimeche M, Hammedi F, Squamous cell carcinoma arising from an epidermal inclusion cyst: A case reportNorth American Journal of Medical Sciences 2010 2(1):46-47. [Google Scholar]
[4]. Frank E, Macias D, Hondorp B, Kerstetter J, Inman JC, Incidental squamous cell carcinoma in an epidermal inclusion cyst: A case report and review of the literatureCase Rep Dermatol 2018 10:61-68.10.1159/00048779429681810 [Google Scholar] [CrossRef] [PubMed]
[5]. Park BS, Shin DH, Kim SH, Perineal squamous cell carcinoma arising from an epidermal cyst: A case reportWorld J Surg Onc 2018 16:15510.1186/s12957-018-1442-230055637 [Google Scholar] [CrossRef] [PubMed]
[6]. Yeh L-P, Liao K-S, Squamous cell carcinoma arising from an epidermal cyst of the scrotumTzu Chi Medical Journal 2013 25:117-18.10.1016/j.tcmj.2012.08.009 [Google Scholar] [CrossRef]
[7]. Tokunaga M, Toya M, Endo Y, Fujisawa A, Tanioka M, Kato M, A case of an undifferentiated squamous cell carcinoma arising from an epidermal cystCase Rep Dermatol Med 2013 2013:01-04.10.1155/2013/46951623476821 [Google Scholar] [CrossRef] [PubMed]
[8]. Sabhlok S, Kalele K, Phirange A, Kheur S, Congenital giant keratinous cyst mimicking lipoma: Case report and reviewIndian J Dermatol 2015 60(6):63710.4103/0019-5154.16916026677303 [Google Scholar] [CrossRef] [PubMed]
[9]. Ding S, Jin Y, Jiang J, Malignant transformation of an epidermoid cyst in the temporal and prepontine region: Report of a case and differential diagnosisOncol Lett 2016 11:3097-100.10.3892/ol.2016.436827123070 [Google Scholar] [CrossRef] [PubMed]