Non-Hodgkin Lymphoma Presenting with Recurrent Pleural Effusion: A Rare Case Report
Kusum V Shah1, Jerin James Dsilva2, Saket Kumar3, Arti D Shah4, Yash Rana5
1 Professor, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
2 Resident, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
3 Postgraduate Resident, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
4 Professor and Head, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
5 Assistant Professor, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jerin James Dsilva, Resident, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Piparia, Vadodara-391760, India.
E-mail: jeenojames@gmail.com
Non-Hodgkin lymphoma (NHL) is a type of carcinoma which usually begins with lymph nodes. Pathogenesis of pleural fluid formation and reabsorption is also associated with pulmonary lymphatic system. Usually pleural effusions are encountered as complications due to infective aetiologies and non-infective causes. Pleural fluid formation and reabsorption in pulmonary lymphatic system are associated with pathogenesis. Authors present here a case report of a patient who presented with left sided severe chest pain investigated to have recurrent pleural effusion, and different clinico-radiological presentations. Computed Tomography (CT) scan showed a mediastinal mass from which CT guided biopsy was done and suggestive of Lymphoma. The patient responded to pleurodesis and chemotherapy.
Chemotherapy, Chest pain, Mediastinal mass, Pleurodesis
Case Report
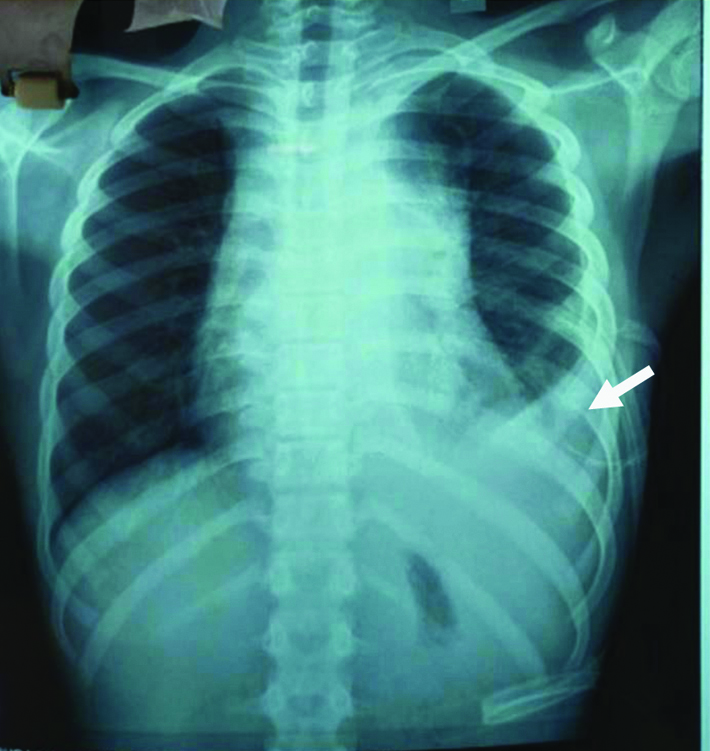
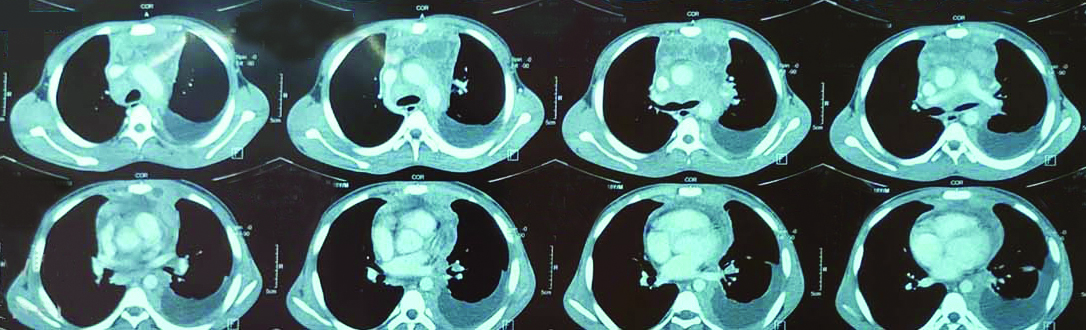
An 18-year-old male, student presented to the Respiratory Medicine Outpatient Department (OPD) with complaints of chest pain, breathlessness, dry cough for past fifteen days and generalised weakness since a month. Patient had past history of dengue fever 8 months back and left sided pleural effusion three months back, underwent pleural tapping in which 500 mL of straw-coloured fluid was tapped. Patient was put on anti-tubercular treatment, which he had continued for a month and then discontinued. Currently, X-ray chest suggestive of left sided mild to moderate pleural effusion with mediastinal widening [Table/Fig-1]. CT thorax was suggestive of anterior mediastinal mass/lymphoma/invasive thymoma with moderate left sided pleural effusion, pericardial effusion, fibrotic changes in upper lobe, possibility of mediastinitis with mediastinal abscess [Table/Fig-2]. Sputum was negative for Acid Fast Bacilli (AFB).
PA view showing left sided pleural effusion.
CT Thorax-suggestive of left-sided pleural effusion and showing mediastinal mass.
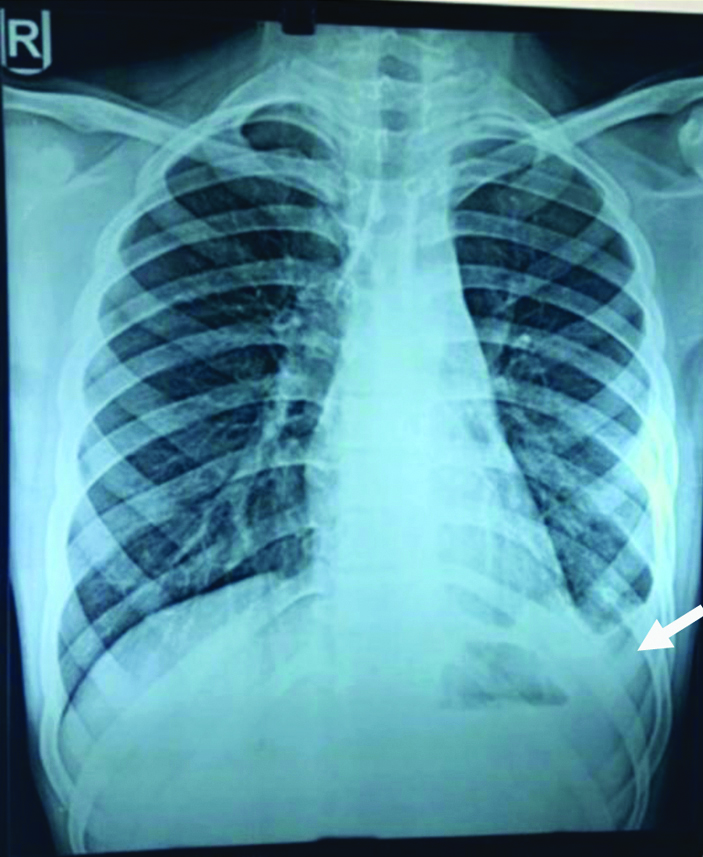
On his stay in hospital, he underwent pleural tapping in which 950 cc of straw-coloured fluid was tapped. Subsequent chest X-rays showed refilling of the effusion, so an intercostal drainage was inserted in the left pleural space and 1100 cc of sero- sanguinous fluid was drained. The pleural fluid was exudative according to routine microscopy, cytology of the pleural fluid showed predominantly lymphocytes and 25% mesothelial cells. The case was further investigated by performing a CT guided biopsy from the mediastinal mass which gave a diagnosis of Non-Hodgkin lymphoma (NHL), the international prognostic score was 1, which was low International Prognostic Index (IPI) group [1]. Pleurodesis done using injection doxycycline and also started on chemotherapy. On follow-up after 1 month in Respiratory Medicine Department, he showed clinico-radiological improvement [Table/Fig-3]. He was continuing his chemotherapy on follow-up.
PA view showing improvement after one month of treatment.
Discussion
Pleural effusions can be one of the most common presentation of tuberculosis, but Malignant Pleural Effusions (MPE) always create an alarm to investigate further and look for intra or extrathoracic malignant lesion which helps to make the perfect diagnosis. More than 75% of MPEs are caused by carcinomas of the lung, breast, ovaries, or by lymphomas [2-7].
Symptomatic intrathoracic disease and pleural effusion is a troublesome and often misleading complication of malignant lymphoma. Lymphomatous effusions are usually exudative. Pathogenesis of pleural fluid formation guides the management of recurrent pleural effusion. In metastatic carcinoma the most common cause of effusions is pleural seeding associated with malignan cells.
Incidence of pleural effusion in cases of NHL is 20% [8]. Pleural effusion if associated with NHL, signifies wide spread disease. The effusion presents unilaterally and bilaterally. Most common symptoms observed are dyspnoea, cough, and chest pain. In the present case the patient presented with dyspnea, dry cough, chest pain and left sided pleural effusion.
Isolated pleural involvement in Diffuse Large B-Cell Lymphoma (DLBCL) is a rare and underdiagnosed entity and should be suspected in patients with non-resolving pleural effusions. Immunohistochemistry for CD20 can be helpful in differentiating primary pleural lymphoma from DLBCL with secondary pleural involvement especially in immunocompetent hosts and has treatment implications.
A retrospective study done on NHL with 86 patients, including 16 subjects with intrathoracic disease. The most common manifestations were paratracheal, mediastinal and hilar lymphadenopathy followed by pulmonary lesions and pleural effusions [8]. In the present case, the patient had left sided pleural effusion and CT Thorax finding of fibrotic changes in left upper lobe and left subsegmental atelectiasis.
Thoracocentesis is the first diagnostic and therapeutic choice in patients with pleural effusion with or without a mass in the mediastinum, respiratory distress. Cytological analysis of pleural fluid and other ancillary studies support the fluid analysis and give quick diagnosis and prognostically significant information for classifying lymphoma or any other disease, its grade and immunophenotype, tumour lysis syndrome, absence or presence of viral DNA should be also seen [9]. In present case, pleural fluid was exudative, borderline ADA, 25% mesothelial cells and had sero-sanguinous appearance, fluid culture was negative and no AFB was detected in pleural fluid.
Thus, pleural fluid analysis had not yield favourable results. Hence, CT guided biopsy from the mediastinal mass was performed and histopathology report was suggestive of NHL.
In a study by Celikoglu F et al., on pleural effusion in NHL, 19 effusion analysis reports were exudative. In three patients, the pleural fluid was milky with an elevated triglyceride level and chylomicrons fulfilling the definition of a chylous effusion. None of the patients reported significantly decreased glucose level. All pleural fluid cultures for routine pathogens and AFB were negative [10].
In the present case after adequate cycles of chemotherapy and Pleurodesis the patient showed clinico-radiological improvement on successive visits.
Conclusion(s)
Pleural effusion may be a predominating sign of NHL. The diagnosis can be obtained in majority of patients by thoracocentesis, needle biopsy, and immunophenotypic marker studies of the pleural fluid. CT scan of the thorax and abdomen is much more revealing compared to conventional roentgenographic techniques in identifying other sites of disease available for establishment of the diagnosis of NHL. Pleural effusion in patients with NHL is usually due to direct involvement of the pleura by lymphoma.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 06, 2020
Manual Googling: Nov 23, 2020
iThenticate Software: Dec 24, 2020 (3%)
[1]. The International Non-Hodgkin’s Lymphoma Prognostic Factors ProjectA predictive model for aggressive Non-Hodgkin’s lymphomaN Engl J Med 1993 329(14):987-94.10.1056/NEJM1993093032914028141877 [Google Scholar] [CrossRef] [PubMed]
[2]. Henschke CI, Yankelevitz DF, Davis SD, Pleural diseases: multimodality imaging and clinical managementCurr Probl Diagn Radiol 1991 20:155-81.10.1016/0363-0188(91)90021-S [Google Scholar] [CrossRef]
[3]. Anderson CB, Philpott GW, Ferguson TB, The treatment of malignant pleural effusionsCancer 1974 33:916-22.10.1002/1097-0142(197404)33:4n%#x003C;916::AID-CNCR28203304054n%#x003E;3.0.CO;2-U [Google Scholar] [CrossRef]
[4]. Storey DD, Dines DE, Coles DT, Pleural effusion. A diagnostic dilemmaJAMA 1976 236:2183-86.10.1001/jama.236.19.2183989808 [Google Scholar] [CrossRef] [PubMed]
[5]. Martinez-Moragon E, Aparicio J, Sanchis J, Menendez R, Cruz Rogado M, Sanchis F, Malignant pleural effusion: Prognostic factors for survival and response to chemical pleurodesis in a series of 120 casesRespiration 1998 65:108-13.10.1159/0000292409580921 [Google Scholar] [CrossRef] [PubMed]
[6]. Skok K, Hladnik G, Grm A, Crnjac A, malignant pleural effusion and its current management: A reviewMedicina (Kaunas) 2019 55(8):490Published 2019 Aug 1510.3390/medicina5508049031443309 [Google Scholar] [CrossRef] [PubMed]
[7]. Dawe CJ, Woolner LB, Parkhill EM, McDonald JR, Cytologic studies of sputum, secretions and serous fluids in malignant lymphomaAmerican Journal of Clinical Pathology 1955 25(5):480-88.10.1093/ajcp/25.5.48014361345 [Google Scholar] [CrossRef] [PubMed]
[8]. Manoharan A, Pitney WR, Schonell ME, Bader LV, Intrathoracic manifestations in non-Hodgkin's lymphomaThorax 1979 34:29-32./10.1136/thx.34.1.29441997 [Google Scholar] [CrossRef] [PubMed]
[9]. Das DK, Serous effusions in malignant lymphomas: A reviewDiagn Cytopathol 2006 34(5):335-47.10.1002/dc.2043216604559 [Google Scholar] [CrossRef] [PubMed]
[10]. Celikoglu F, Teirstein AS, Knellenstein DJ, Strauchen JA, Pleural effusion in non-Hodgkin’s lymphomaChest 1992 101(5):1357-1360.10.1378/chest.101.5.13571582297 [Google Scholar] [CrossRef] [PubMed]