The Fibreoptic Bronchoscopy (FOB) is a gold standard tool for visualisation and definitive diagnosis of endobronchial lesions [1,2]. Computed Tomography (CT) prior to FOB provides a roadmap to bronchoscopist to target endobronchial lesions [3]. In clinical practice, those patients who had mismatch between FOB and CT image findings had to undergo further invasive procedure to obtain correct diagnosis. This study compared radiologist’s perspective of CT thorax image findings with that of pulmonologist’s finding at bronchoscopy. Present study was done to evaluate the type of lesions not accurately identified by CT. This will enable bronchoscopists to be more vigilant while planning for diagnostic procedures and prevent repeated invasive investigations, the associated risks and cost. The primary outcome of the study was to analyse the disparity between findings of CT thorax and FOB and secondary outcome was to assess the diagnostic yield of samples obtained by FOB.
Materials and Methods
This study is a cross-sectional retrospective study done in a Tertiary Care Centre in Vydehi Institute of Medical Sciences and Research Centre, Bangalore, India from January 2012 to December 2018. Details were collected from medical records after the study was approved by the Institutional Ethical Committee (EC No. -VIEC/2019/APP/035).
Inclusion criteria: Patients who underwent CT thorax followed by bronchoscopy during January 2012 to December 2018.
Exclusion criteria: Patients who did not undergo CT thorax in our institution.
The number of patients included in the study was 426. Clinical history, clinical examination and details of relevant investigations done were collected. CT thorax was performed for all patients with helical CT with 5 mm cuts with multiplanar reconstruction using Siemen’s SOMATOM definition AS (128 slice), model no. 240 (10141785), Germany, single breath hold, 0.6 mm collimation, 1.2 pitch, 1 mm reconstruction, 80-120 kVp, 90-260/300 mA spanning from T1 vertebra to the domes of diaphragm. Contrast CT was performed using 1 mL/kg of Omnipaque. 352 (82.62%) patients underwent Contrast Enchanced CT (CECT) thorax. With 128 slice images and proper breath-hold technique, all the images were assessed for quality. Two experienced radiologists independently reviewed the reports and a common consensus was reported. FOB was performed using Olympus BF type 1T 150 (Tokyo, Japan). The endobronchial findings on CT thorax imaging and FOB were recorded as normal bronchus, abnormal mucosa, endobronchial mass and extrinsic compression of bronchus. The findings were noted from CT reports and bronchoscopy procedure notes described in records. Cytological and/or histological reports were collected from bronchoscopy register. Working case definitions used in the study were as per [Table/Fig-1] [4-6]. If findings were equivocal, the predominant finding of CT imaging and bronchoscopy were noted. The findings of CT thorax imaging were compared with that of FOB. Bronchoalveolar Lavage (BAL), Endobronchial Biopsy (EBB), and Transbronchial Node Aspiration (TBNA) were done as per case to case basis. EBB was done using Olympus biopsy forceps (Model No. FB-19CR-1). TBNA was done using eXcelon transbronchial aspiration needle (Boston Scientific, Spencer, USA). Accordingly samples obtained from FOB were sent for pathological examination and relevant cultures.
Working case definitions used in the study [4-6].
| Definition in study | CT thorax | Bronchoscopy |
|---|
| 1. Abnormal mucosa | Mucosal nodularity- diffuse/focal. | The presence of one or more of the following findings on FOB- mucosal oedema, mucosal erythema, mucosal friability, mucosal irregularity and loss of bronchial mucosal markings. |
| 2. Mass | Partial or complete occlusion of bronchial lumen and/or the presence of bronchus cut-off sign. | Presence of an endobronchial growth completely or partly occluding the bronchial lumen. |
| 3. Extrinsic compression | Compression of the bronchus due to surrounding anatomical structures without evidence of mucosal involvement. | Bronchial narrowing due to compression of bronchial lumen from surrounding structures and visualised mucosa is apparently normal. |
The pathological diagnosis included malignancy, infections, inflammatory lesions and miscellaneous diseases. The pathological typing of lung cancer was classified as per World Health Organisation (WHO) [7].
Statistical Analysis
Statistical analysis was done using SPSS 18.0 version (IBM Inc., Armonk, New York, USA). Sensitivity, specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV), diagnostic accuracy, likelihood ratio of a positive test and negative test and Kappa co-efficient were calculated comparing CT thorax imaging with FOB. Yield of EBB and transbronchial node aspiration were represented in percentages.
Results
This study included 426 patients out of which 309 (72.53%) were males and 117 (27.47%) were females. The male:female ratio in the study was 2.6:1. 277 (65.02%) were smokers, out of which 274 (98.91%) were males and 3 (1.08%) were females. Demographic characteristics and indications for performing FOB have been shown in [Table/Fig-2].
Demographic characteristics, presenting complaints of patients and indications for performing FOB.
| Characteristics | Number (%) |
|---|
| Males | 309 (72.53%) |
| Females | 117 (27.47%) |
| Mean age (years) | 49.4 |
| Smokers | 277(65.02%) |
| Presenting complaints |
| Cough | 246 (57.74%) |
| Breathlessness | 232 (54.46%) |
| Chest pain | 217 (50.93%) |
| Hemoptysis | 149 (34.97%) |
| Fever | 162 (38.02%) |
| Loss of appetite and weight | 254 (59.62%) |
| Indications of FOB |
| Suspected infection | 154 (36.15%) |
| Suspected malignancy | 252 (59.57%) |
| Interstitial lung disease | 9 (2.11%) |
| Atelectasis | 8 (1.87%) |
| Administration of drugs | 3 (0.70%) |
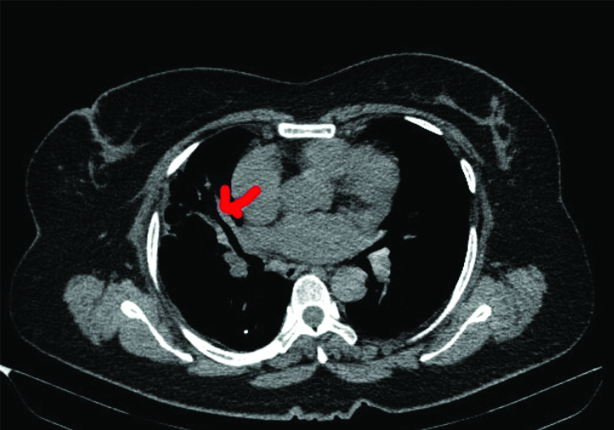
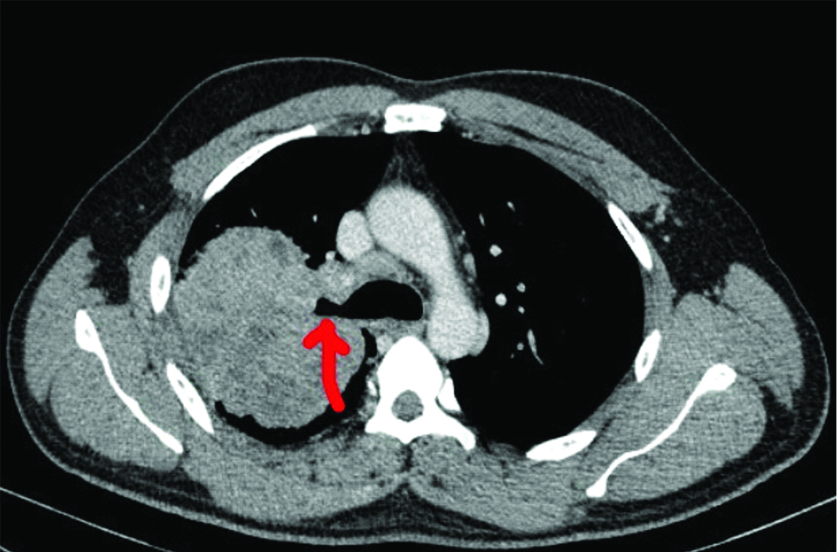
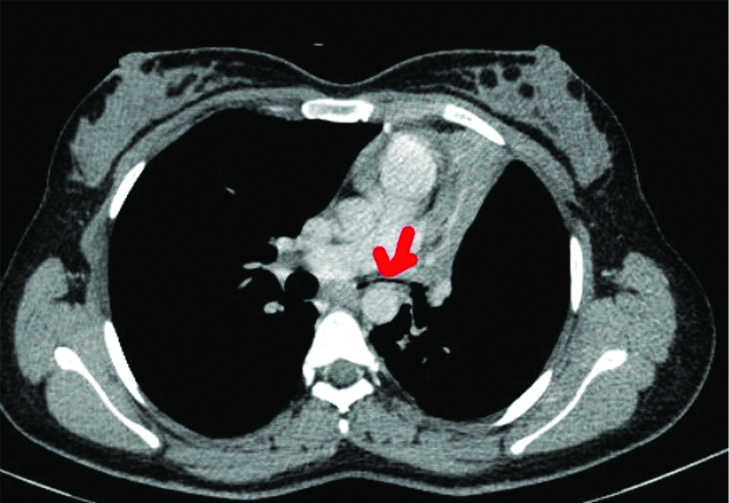
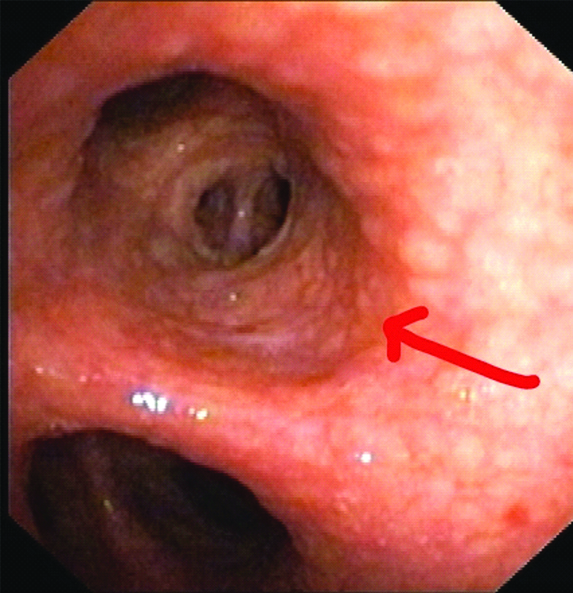
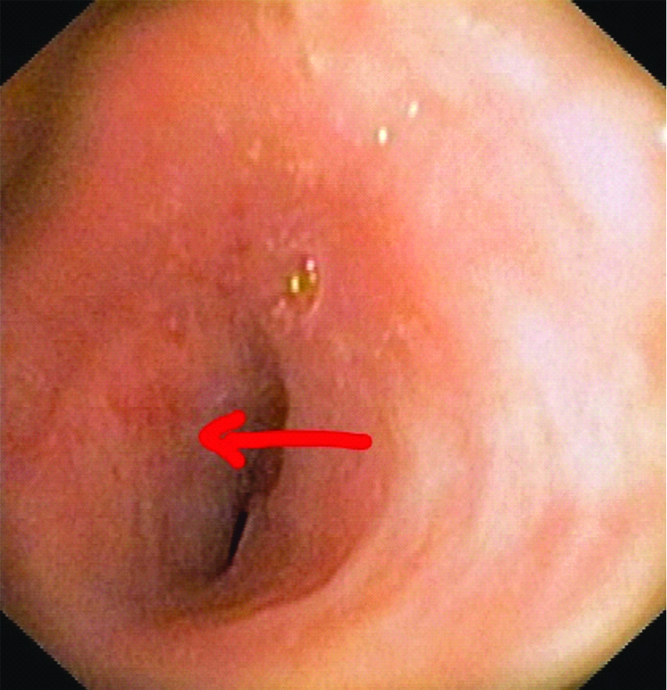
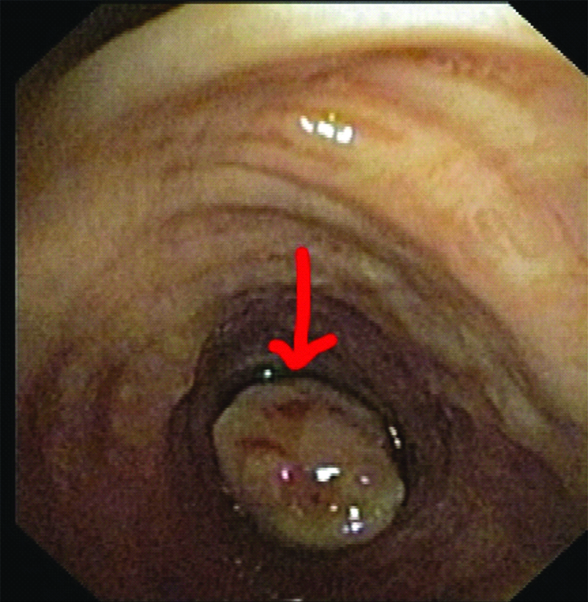
On CT thorax, normal bronchus, abnormal mucosa [Table/Fig-3], endobronchial mass [Table/Fig-4] and extrinsic compression [Table/Fig-5] was found in 242 (56.80%), 17 (3.99%), 122 (28.63%) and 45 (10.56%) patients respectively. Among findings on FOB, normal bronchus, abnormal mucosa [Table/Fig-6], endobronchial mass [Table/Fig-8] and extrinsic compression [Table/Fig-7] was found in 244 (57.27%), 40 (9.3%), 100 (23.47%) and 42 (9.85%) patients respectively [Table/Fig-9]. CT thorax imaging and bronchoscopy reports of 426 patients were compared. The sensitivity of CT for presence of normal bronchus, abnormal mucosa, endobronchial mass and extrinsic compression was 93.03%, 27.50%, 89.00% and 59.52% and specificity was 91.76%, 98.45%, 89.88% and 94.79% respectively [Table/Fig-9].
CT thorax image showing right endobronchial irregularity (Red arrow).
CT thorax image showing right main bronchus “cut-off” sign (Red arrow).
CT thorax image showing extrinsic compression of left main bronchus (Red arrow).
FOB showing irregular(cobble-stone) appearance of endobronchial mucosa (Red arrow).
FOB showing extrinsic compression of bronchus (Red arrow).
FOB showing endobronchial mass lesion (Red arrow).
Diagnostic validity of CT thorax versus FOB in identification of normal bronchus, abnormal mucosa, endobronchial mass and extrinsic compression.
| Normal FOB | Abnormal FOB | Sensitivity | Specificity | Positive predictive value | Negative predictive value |
|---|
| CT imaging |
| Bronchus |
| Normal | 227 | 15 | 93.03% | 91.76% | 93.8% | 90.76% |
| Abnormal | 17 | 167 | | | | |
| Total | 244 | 182 | | | | |
| Abnormal bronchus | Present on FOB | Absent on FOB | | | | |
| 1) Abnormal mucosa |
| Present | 11 | 6 | 27.5% | 98.45% | 64.71% | 92.91% |
| Absent | 29 | 380 | | | | |
| Total | 40 | 386 | | | | |
| 2) Endobronchial mass |
| Present | 89 | 33 | 89% | 89.88% | 72.95% | 96.38% |
| Absent | 11 | 293 | | | | |
| Total | 100 | 326 | | | | |
| 3) Extrinsic compression |
| Present | 25 | 20 | 59.52% | 94.79% | 55.56% | 95.54% |
| Absent | 17 | 364 | | | | |
| Total | 42 | 384 | | | | |
Patients with abnormal bronchial mucosa (40) and endobronchial mass (100) were subjected to EBB [Table/Fig-9]. Bronchoscopic biopsy was deferred in one patient due to spontaneous bleed from the lesion. Hence, 139 (32.62%), 22 (5.16%) and 211 (49.53%) cases underwent EBB, TBNA and BAL respectively. Out of 22 TBNA cases, 19 were from station seven (subcarinal lymph node) and three from station 4R (right paratracheal lymph node). Out of 139 EBB done, pathological diagnosis was obtained in 135 (97.12%) [Table/Fig-10]. Transbronchial node aspiration yielded results in 12 (54.54%) of 22 cases. The most common pathological finding was malignancy in patients who were subjected for EBB. The most common malignancy was squamous cell carcinoma in 43 (26.54%) patients followed by adenocarcinoma in 32 (19.75%) patients and non-small cell carcinoma (not otherwise specified) in 22 (13.58%) patients [Table/Fig-10].
Pathological diagnosis of lesions detected on FOB.
| Pathological diagnosis | Abnormal mucosa (%) | Endobronchial mass (%) | Transbronchial node aspiration (%) |
|---|
| Adenocarcinoma | 11 (27.50%) | 19 (19.00%) | 2 (9.09%) |
| Squamous cell carcinoma | 11 (27.50%) | 30 (30.00%) | 2 (9.09%) |
| Small cell carcinoma | 5 (12.50%) | 8 (8.00%) | 0 |
| Non- small cell carcinoma (not otherwise specified) | 3 (7.50%) | 18 (18.00%) | 1 (4.54%) |
| Poorly differentiated carcinoma | 5 (12.50%) | 8 (8.00%) | 1 (4.54%) |
| Inconclusive | 1 (2.50%) | 3 (3.00%) | 12 (54.54%) |
| Miscellaneous tumours | 3 (7.50%) | 7 (7.00%) | 0 |
| Infections | 0 | 6 (6.00%) | 0 |
| Inflammation | 1 (2.50%) | 0 | 4 (18.18%) |
| Deferred | 0 | 1 (1.00%) | 0 |
| Total | 40 | 100 | 22 |
Discussion
Despite an era of rapidly progressing interventional pulmonology, there is no substitute till date to initial assessment of bronchial tree by CT thorax. Present study compared radiologist’s perspective of CT thorax endobronchial findings with that of pulmonologist’s finding on bronchoscopy. Disparity between endobronchial findings of CT thorax and FOB have been noted in day to day practice. Hence, this study was designed to shed light on the diagnostic validity of CT in the epoch of advanced CT imaging, by comparing it with findings on FOB in identifying endobronchial lesions.
Computed Tomography is the first investigation when endobronchial disease is suspected clinically and on chest radiograph, before fibre-optic bronchoscopy. CT thorax helps to increase the diagnostic yield of bronchoscopy by targeting the suspicious lesions, staging in cases of malignancy and follow-up of patients [8-10]. CT helps in detection of extraluminal abnormalities and detection of distant disease which is not visualised on FOB [11,12]. FOB is the gold standard for the investigation of endobronchial diseases [1,2]. FOB allows direct visualization of tracheo-bronchial tree and to collect biological specimens from suspicious areas thereby helping in establishment of diagnosis. It is also useful for staging of lung malignancies [8].
The present study was an attempt to know the type of lesions which are misinterpreted on CT scan, so that pulmonologists could be more careful while selecting patients for bronchoscopy and it’s related interventions. CT imaging done prior to FOB will guide the bronchoscopist regarding the need of subjecting the patient for FOB depending on the bronchoscopic accessibility of the lesion and if accessible, to know the most appropriate technique to achieve sample for definitive diagnosis. As per Laroche C et al., performing bronchoscopy after CT scan of thorax improved the accuracy of diagnosis significantly, avoids an invasive procedure in 7% of patients and prevents another invasive investigation in 10% of patients [8]. FOB is usually an effective and safe procedure, yet it is not without any complications especially in the debilitated, elderly and those with co-morbidities such as obstructive airway diseases and cardiac diseases [13]. The attributable mortality rate of fibreoptic bronchoscopy has been <0.1%-0.5% and complication rate has been 0.739% and 0.5-0.8% [6,12,14-18]. Therefore, appropriate selection of patients for bronchoscopy would avoid not only the discomfort, cost and complications of an invasive procedure like bronchoscopy but also prevent the brunt of second invasive procedure to achieve the diagnosis if bronchoscopy is inconclusive.
Naidich DP et al., did a retrospective study with a sample size of 102 patients and concluded that there is good overall statistical correlation between axial CT and FOB in identification of focal bronchial abnormality [5]. Out of 64 cases, 59 who were earlier diagnosed as abnormal on CT were confirmed on performing FOB. CT predicted normal bronchus in 35 out of 38 cases which were normal on FOB. The authors inferred that axial CT was inaccurate in predicting whether a given focal abnormality will be endobronchial, submucosal or extrinsic [5].
Finkelstein SE et al., studied on 44 patients and inferred sensitivity of super high-resolution CT in predicting mucosal abnormality, mass and extrinsic compression was 16%, 90% and 100%, respectively, while present study showed the sensitivity of CT for presence of normal bronchus, abnormal mucosa, mass and extrinsic compression was 93.03%, 27.50%, 89.00% and 59.52%, respectively. Authors did not mention about specificity of CT with respect to type of endobronchial lesions. CT sensitivity to detect extrinsic compression was 100% against the present study value of 59.52%. This disparity could be due to large variation in sample size between present study and of Finkelstein et al. [19].
One finding common between present study and those of Naidich DP et al., and Finkelstein SE et al., is sensitivity of CT imaging in predicting mucosal abnormalities is low [5,19].
As per study done by Lee et al., with respect to location of the lesion (submucosal, endobronchial or peribronchial), in 23 (77%) out of 30 patients FOB corresponded with CT [2].
Present study showed overall PPV of 93.8%, NPV of 90.76% and diagnostic accuracy of 92.49% of CT thorax in detection of endobronchial disease. Bungay HK et al., in their study revealed PPV of 85% and NPV of 78% of axial CT in detection of endobronchial mass lesion. Overall better PPV and NPV in present study are probably due to usage of advance CT imaging. Bungay HK et al., did not take into consideration abnormal mucosa and extrinsic compression of bronchus. They found sensitivity of 60.6% and specificity of 86.2% in detection of endobronchial mass by CT [12].
The secondary outcome of the present study was to analyse the pathological diagnosis of samples and conclusive result was achieved in 135 (97.12%) of 139 cases. Though bronchoscopy is an operator-dependent procedure which has led to success rate of diagnosis of lung cancer varying between 50-86%, present study achieved diagnosis in 97.12% of cases [12,20,21]. In present study, 43 (26.54%) of patients had squamous cell carcinoma followed by adenocarcinoma in 32 (19.75%) patients and non-small cell carcinoma (not otherwise specified) in 22 (13.58%) patients. Higher percentage of squamous cell carcinoma presenting as endoscopically visible growth was also seen in studies done by Gao L et al., Kumar V et al., and Parvathi BKL et al. [22-24].
To our best knowledge after literature search, present is the only study with a large sample size of 426 patients done exclusively by pulmonologists till now to evaluate the discrepancy between CT and FOB.
Limitation(s)
It is a retrospective study done in a single centre and the exact time interval between CT thorax scan and FOB could not be retrieved from records.
Conclusion(s)
CT thorax imaging has good sensitivity and specificity to detect endobronchial mass but has poor sensitivity for detection of extrinsic compression and mucosal abnormalities in bronchi. Squamous cell carcinoma was the most common pathological diagnosis.
Future research direction is to do a large scale prospective study assessing whether advanced CT imaging techniques inclusive of real-time virtual bronchoscopy (VB) with FOB provides guidance to pulmonologists regarding best sampling technique to achieve diagnosis.