Dry eyes is increasing at an appalling rate all over the world and is one of the most frequent diagnosis especially in the field of ophthalmology [1]. Tear film and ocular surface society dry eye workshop II defines DED as a multifactorial disease of the ocular surface characterised by a loss of homeostasis of the tear film, causing increased evaporation and reduced tear production, accompanied by ocular discomfort and visual disturbances [2]. Prevalence of DED is 18.4% to 54.3% in India, 11% for men and 17% for women worldwide [3]. Symptoms includes a dry gritty feeling in the eyes that is often accompanied by burning, redness, and the sensation of a foreign object in the eye.
The tear film is composed of three layers, the outermost lipid layer secreted by meibomian glands, middle aqueous layer produced by lacrimal gland and innermost is the mucin layer formed by the goblet’s cells of conjunctiva. When there is a dysfunction of the meibomian glands, changes are observed in the lipid composition leading to increased viscosity and decreased gland outflow, causing thinning of the tear film layer and increasing its evaporation time [4]. Surgeons are at a higher risk as most of their training occurs inside the Operating Room (OR), where the ventilation environment is enclosed and the use of a microscope requires greater concentration and fixation on fine details, decreasing the blink rate, causing damage to the ocular surface and affecting quality of life [5]. Therefore, the presence of prompt factors affects the performance of the physician-in-training because of how it impacts visual function and general welfare.
The present study helps to understand the burden of DED in medical field and analyses multiple variants of DED in the surgical and non-surgical residents based on their lifestyle habits and advice appropriate management to curb its exponential rise in a tertiary care hospital Vadodara, Gujarat, India.
Materials and Methods
The present study was an observational single centric cross-sectional study which was carried out in the Department of Ophthalmology from April 2020 to June 2020, to assess the prevalence of dry eyes in postgraduate students of tertiary care hospital. All participants were assessed on a number of variables, that is duration of residency, smoking, use of cosmetics, screen time and distance of screen from eyes. The study was initiated after Institutional Ethics Committee (IEC) approval (Certificate No: SVIEC/ON/Medi/SRP/20009).
Inclusion criteria: A total of 132 postgraduate students of 24 to 30 years of age belonging to 1st to 6th year of residency were included in the study.
Exclusion criteria: Postgraduate students who had a history of pre-existing ocular surface disorder, prior ocular surgery or trauma, topical or systemic drugs affecting ocular surface, any autoimmune disease, use of contact lens and any drug addiction were excluded from the study.
After enrolling in the study and obtaining consent, a detailed demographic, personal and lifestyle history was taken and recorded in a predefined proforma. Then they underwent following DED evaluation;
Schirmer test
TBUT test
MGD grading
Conjunctival staining
Schirmer test [5]
The test was performed using Whatman no. 41 strip after instilling 0.5% paracaine eye drops and readings were observed after 5 minutes. Positive findings were documented if strip wetting was less than 10 mm in 5 minutes. Readings were categorised as mild (11-15 mm), moderate (6-10 mm) and severe (<5 mm).
TBUT [6]
Fluorescein strip was applied on ocular surface of patient and asked not to blink while the tear film was observed under a broad beam of cobalt blue illumination till the first dry area was noted. A TBUT <10 seconds was defined as presence of dry eyes and >10 seconds was normal. Readings were categorised as mild (11-15 seconds), moderate (6-10 seconds) and severe (<5 seconds).
MGD grading [7]
Quality of meibum was assessed in each of the eight glands of the central third of the lower lid, on a 0-3 scale for each gland:
0=clear meibum
1=cloudy meibum
2=cloudy with debris (granular)
3=thick like toothpaste.
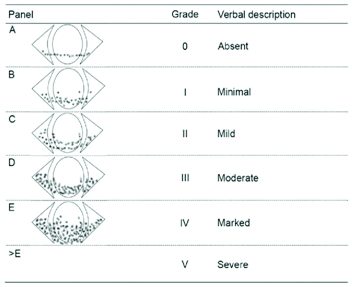
Conjunctival Staining (Oxford schema) [8]
Staining the lower tarsal conjunctiva with fluorescein strip which is represented by punctate dots on a series of panels (A-E). Staining ranges from 0-5 for each panel and 0-15 for the total exposed inter-palpebral conjunctiva and cornea. The dots are ordered on a log scale and graded [Table/Fig-1].
Conjunctival Staining (Oxford Schema) [8].
Statistical Analysis
All data were analysed by statistical software SPSS Version 20.0. Chi-square test for Goodness of Fit was used to analyse the data and p-value <0.05 was considered significant.
Results
The present study enrolled total 132 (264 eyes) postgraduate students from tertiary care hospital. Prevalence of DED was more in surgical field (62.67%) compared to non-surgical (37.33%) residents based on TBUT with an OR of 3.35, p-value <0.0001 and risk ratio of 1.67 [Table/Fig-2].
Prevalence of DED in surgical and non-surgical residents.
| Speciality | DED present in number of eyes | % | DED absent in number of eyes | % | Total number of eyes | Odds ratio | Risk ratio | p-value |
|---|
| Surgical | 94 | 62.67 | 38 | 33.33 | 132 | 3.35 | 1.67 | <0.0001 |
| Non-surgical | 56 | 37.33 | 76 | 66.67 | 132 |
| Total | 150 | 100.00 | 114 | 100.00 | 264 |
(Chi-square test used); p<0.05 significant
There were 60 females and 72 males with a prevalence of DED which was found to be high in surgical field.
Smokers were at higher risk of developing DED compared to non-smokers with a significant p-value of 0.001. Also, residents who spent long hours on screen (>4 hours/day) and at a distance of more than arm-forearm length had a higher prevalence of DED with a significant p-value of 0.001 and 0.002 [Table/Fig-3]. More number of smokers were from surgical residents (p-value-0.020) [Table/Fig-4].
Presence of dry eyes based on TBUT using different variables.
| Risk factors | TBUT (<10 seconds)N (%) | TBUT (>10 seconds)N (%) | Total (eyes) | p-value |
|---|
| 1st year residents | 58 (70.73%) | 24 (29.27%) | 82 | 0.001* |
| 2nd year residents | 46 (56.10%) | 36 (43.90%) | 82 | 0.269 |
| 3rd year residents | 34 (44.74%) | 42 (55.26%) | 76 | 0.358 |
| 4th year residents | 8 (80%) | 2 (20%) | 10 | 0.057 |
| 5th year residents | 2 (25%) | 6 (75%) | 8 | 0.157 |
| 6th year residents | 2 (33.34%) | 4 (66.67%) | 6 | 0.414 |
| Smoker | 48 (75%) | 16 (25%) | 64 | 0.001* |
| Non-smoker | 102 (51%) | 98 (49%) | 200 | 0.777 |
| Users of hormonal contraceptive | 2 (33.34%) | 4 (66.67%) | 6 | 0.414 |
| Non-users of hormonal contraceptive | 62 (24.03%) | 196 (75.96%) | 258 | 0.001* |
| Users of make up | 48 (60%) | 32 (40%) | 80 | 0.038* |
| Non-users of make up | 16 (8.69%) | 168 (91.30%) | 184 | 0.001* |
| Screen time (1-2 hours/day) | 2 (33.34%) | 4 (66.67%) | 6 | 0.414 |
| Screen time (3-4 hours/day) | 38 (65.52%) | 20 (34.48%) | 58 | 0.018* |
| Screen time (>4 hours/day) | 128 (64%) | 72 (36%) | 200 | 0.001* |
| Distance from screen (<Arm forearm length) | 10 (33.34%) | 20 (66.67%) | 30 | 0.067 |
| Distance from screen (>Arm forearm length) | 140 (59.38%) | 94 (40.17%) | 234 | 0.002* |
*Statistically significant p-value; (Chi-square test used)
Prevalance of DED in surgical and non-surgical residents with risk factors who had a TBUT of <10 seconds.
| Risk factors | SurgicalN (%) | Non-surgicalN (%) | Total | p-value |
|---|
| 1st year residents | 36 (62.07%) | 22 (37.93%) | 58 | 0.066 |
| 2nd year residents | 28 (60.87%) | 18 (39.13%) | 46 | 0.140 |
| 3rd year residents | 20 (58.82%) | 14 (41.18%) | 34 | 0.303 |
| 4th year residents | 6 (75%) | 2 (25%) | 8 | 0.157 |
| 5th year residents | 2 (100%) | 0 | 2 | NA |
| 6th year residents | 2 (100%) | 0 | 2 | NA |
| Smoker | 32 (66.67%) | 16 (33.34%) | 48 | 0.020* |
| Non-smokers | 62 (60.78%) | 40 (39.21%) | 102 | 0.029* |
| Users of hormonal contraceptive | 0 | 2 (100%) | 2 | NA |
| Non-users of hormonal contraceptive | 38 (61.29%) | 24 (38.71%) | 62 | 0.075 |
| Make up users | 18 (37.5%) | 30 (62.5%) | 48 | 0.083 |
| Non-makeup users | 6 (37.5%) | 10 (62.5%) | 16 | 0.317 |
| Screen time (1-2 hours/day) | 0 | 2 (100%) | 2 | NA |
| Screen time (3-4 hours/day) | 28 (71.05%) | 10 (28.94%) | 38 | 0.009* |
| Screen time (>4 hours/day) | 78 (60.94%) | 50 (39.06%) | 128 | 0.013* |
| Distance from screen (<Arm forearm length) | 2 (20%) | 8 (80%) | 10 | 0.06 |
| Distance from screen (>Arm forearm length) | 92 (65.71%) | 48 (34.29%) | 140 | 0.002* |
*Statistically significant p-value; (p-value is calculated from each year of residency); (Chi-square test used)
The overall p-value was significant amongst the postgraduates and surgical and non-surgical residents as 0.004 and 0.043, respectively by using Chi-square test [Table/Fig-5]. The DED was categorised on the basis of schirmer’s II test, TBUT, MGD grading, Conjunctival staining. According to the results obtained from these tests number of residents with mild DED were more than severe form of disease [Table/Fig-6].
Distribution of surgical and non-surgical residents based on TBUT readings.
| Residents | Surgical residents | Non-surgical residents |
|---|
| TBUT (<10 seconds)n (%) | TBUT (>10 seconds)n (%) | TBUT (<10 seconds)n (%) | TBUT (>10 seconds)n (%) |
|---|
| 1st year residents | 36 (81%) | 8 (19%) | 22 (57%) | 16 (43%) |
| 2nd year residents | 28 (66.67%) | 14 (33.33%) | 18 (45%) | 22 (55%) |
| 3rd year residents | 20 (55%) | 16 (454%) | 14 (35%) | 26 (65%) |
| 4th year residents | 6 (100%) | 0 | 2 (50%) | 2 (50%) |
| 5th year residents | 2 (100%) | 0 | 0 | 6 (100%) |
| 6th year residents | 2 (100%) | 0 | 0 | 4 (100%) |
*p-value of 1st, 2nd and 3rd year residents was 0.004 while of 4th, 5th and 6th year was 0.043. Both are statistically significant when comparing with surgical and non-surgical residents; (Chi-square test used)
Panel of other tests in residents who had DED.
| Test | Mild DED n (%) | Moderate DED n (%) | Severe DED n (%) |
|---|
| Schirmer’s II (mm) (Mean±SD) | 201 (76.13%) 12.65±1.58 | 43 (16.28%) 8.98±1.58 | 20 (7.57%) 2.83±0.47 |
| TBUT (sec) (Mean±SD) | 214 (81.06%) 12.12±0.67 | 29 (10.98%) 7.83±1.49 | 21 (7.95%) 1.53±0.79 |
| MGD grading | 220 (83.33%) | 26 (9.8%) | 18 (6.81%) |
| Conjunctival staining | 224 (84.84%) | 26 (9.8%) | 14 (5.30%) |
n= number of eyes, the dry eye disease is categorised on the basis of schirmer’s II test, TBUT, MGD grading, Conjunctival staining, according to results obtained from these tests number of residents with mild DED were more than severe form of disease
In present study, no residents were using contraceptives, hence results were inconclusive and 48 were using cosmetics which also affected ocular surface causing DED (p-value=0.083).
Discussion
The present study was performed in a tertiary care hospital on a total of 132 residents (264 eyes) which included 66 (132 eyes) from surgical and 66 (132 eyes) from non-surgical fields with an average age of 28.2 years. Overall prevalence of DED was 56.81% in the medical field. There were 60 females and 72 males with a prevalence of DED more in surgical (62.67%) compared to medical (37.33%) residents based on TBUT with an odds ratio of 3.35, p-value <0.0001 and risk ratio of 1.67. Most residents had a multiscreen lifestyle spent on mobiles, tablets and laptops while surgeons had additionally increased screen time due to spending long hours in the OR with prolonged microscopic exposure [5].
Smokers were at higher risk of developing DED compared to non-smokerss with a significant p-value of 0.001. Also, more smokers were from the surgical residents (p-value-0.020). In a meta-analysis conducted by Xu L et al., it is suggested that there was a significant association between smoking and DED with an OR of 1.05 and p-value of 0.016 [9].
Also, residents who spent long hours on screen (>4 hours/day) and at a distance of more than arm-forearm length had a higher prevalence of DED with a significant p-value of 0.001 and 0.002, respectively. Surgical residents spent long screen hours in contrast to non-surgical residents (p-value 0.013). Similar to a study by Abudawood GA et al., where in the duration of study along with screen brightness and distance from screen was statistically significant risk factor (p-value 0.02) [10].
A study by Hassan A and MMK B studying Computer Vision Syndrome (CVS) in medical students deduced results based on level of screen and duration of students with adequate breaks in between which was significant for symptoms such as redness and burning, a limitation that was not considered in present study [11]. While, in a study conducted in suburban Chennai it was concluded that CVS was higher in engineering (81.9%) compared to medical (78.6%) students with increased development of redness, burning sensation and blurred vision [12].
In the present study it was found that prevalence of DED was more amongst the first year residents which may be attributable to long waking hours and extensive paperwork duties based on TBUT results with a significant p-value of 0.001, respectively. The overall p-value was significant amongst the postgraduation and super specialty residents as 0.004 and 0.043, respectively. In a study by Castellanos-González JA et al., significant DED was found in first and fourth year residents (p=0.003; p=0.001, respectively) [5].
Based on the results of all the conventional tests performed, most of the residents had mild DED by MGD grading (83.3%) and conjunctival staining (84.84%), respectively followed by moderate to severe category. In a study by Tong L et al., conducted in a tertiary referral clinic, Singapore, most of his patients (200 participants) had a mixed variety of DED, i.e., evaporative and aqueous deficient, based on MGD grading and fluorescein staining was most severe in central and inferior corneas when graded by Oxford Schema method [13].
The DED was more in females (58.29%) as compared to males (41.71%), in accordance to a study by Sullivan DA et al., which suggested that androgen absence in females, Sjogren’s syndrome and ageing was the cause of DED in them [14]. Also, oestrogen helps in smooth functioning of lacrimal gland, maintaining the ocular surface in good health but contraceptives can lead to a hormonal imbalance [15]. In present study, not many residents were using contraceptives, hence, results were inconclusive. In present study, 48 females were using cosmetics which also affected ocular surface causing DED (p-value=0.038). A study by Wang MT and Craig JP showed that eyeliners causes tear film contamination and its debris blocks the ducts of meibomian glands [16].
Limitation(s)
In the present study, DED evaluation was based on conventional test such as TBUT, Schirmer, Conjunctival staining pattern and MGD grading, but many newer tests like tear film inferometry, non-contact meibography, tear osmolality assessment and tests that measure MMP 9 are available and needs extensive research. These are automated non-invasive tests that quantify the disease severity, which was a limitation in present study.
Conclusion(s)
Overall prevalence of DED was 56.81% in the medical field amongst residents. Surgeons have a 3.35 chance greater than non-surgical residents for development of DED. Hence, early diagnosis and curbing the modifiable risk factors can reduce the burden of DED and improve the quality of life.
(Chi-square test used); p<0.05 significant
*Statistically significant p-value; (Chi-square test used)
*Statistically significant p-value; (p-value is calculated from each year of residency); (Chi-square test used)
*p-value of 1st, 2nd and 3rd year residents was 0.004 while of 4th, 5th and 6th year was 0.043. Both are statistically significant when comparing with surgical and non-surgical residents; (Chi-square test used)
n= number of eyes, the dry eye disease is categorised on the basis of schirmer’s II test, TBUT, MGD grading, Conjunctival staining, according to results obtained from these tests number of residents with mild DED were more than severe form of disease