Locally Advanced Bladder Paraganglioma Managed with Robot-assisted Radical Cystectomy with Intracorporeal Neobladder- A Case Report
Anoop Handa1, Sharat Chandra Dash2, Nimit Solanki3, Gagandeep Singh4
1 Senior Resident, Department of Urology, Army Hospital Research and Referral, New Delhi, India.
2 Consultant, Department of Urology, Army Hospital Research and Referral, New Delhi, India.
3 Consultant, Department of Urology, Base Hospital, Delhi Cantt, New Delhi, India.
4 Consultant, Department of Urology, Command Hospital, Udhampur, Jammu and Kashmir, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anoop Handa, G-23, DLF Capital Greens, Moti Nagar-110015, New Delhi, India.
E-mail: dr.anoop10@gmail.com
Paragangliomas are neuroendocrine tumours of extra-adrenal origin. Primary bladder paragangliomas are rare and have variable functional status, which presents a challenge in their management by minimally invasive surgery. Surgical resection necessitates minimal intraoperative handling of tumour, minimising physiological deterioration. Here in, a case is reported of incidentally detected locally advanced bladder paraganglioma which was managed successfully with robot-assisted radical cystectomy and intracorporeal ileal neobladder formation.
Neuroendocrine tumours, Robotic surgery, Urinary bladder
Case Report
A 36-year-old male with no co-morbidities presented in the Department of Urology, with complaint of left sided flank pain, which lasted for four days. Pain was mild in intensity, colicky and which relieved spontaneously. There was no history of fever, lower urinary tract symptoms, haematuria, syncope, trauma, altered bowel habits, headache or any palpitations. There was no history of any surgical intervention in the past. General physical and systematic examination was unremarkable. Ultrasound abdomen revealed 4×3.9×3.6 cm well-defined lobulated mixed echogenic mass in posterolateral wall of urinary bladder. Urine cytology for malignant cells showed degenerated squamous cells. Contrast Enhanced Computed Tomography (CECT) scan showed 5.2×4.2×5 cm exophytic, enhancing mass lesion in the left posterolateral wall of the urinary bladder.
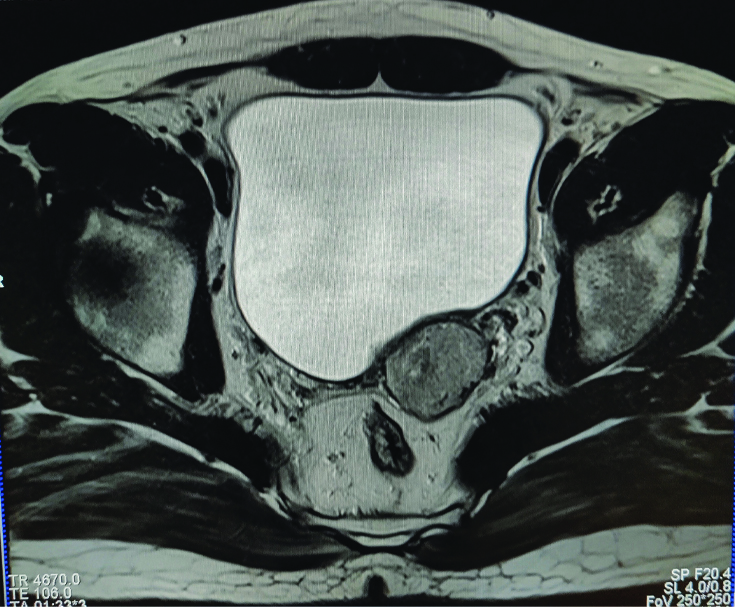
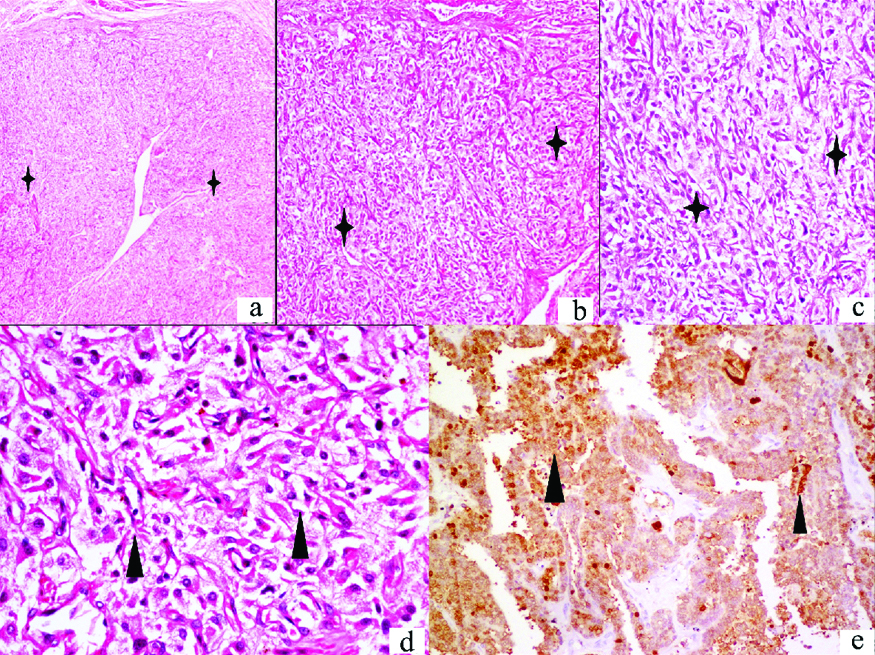
Patient then underwent cystoscopy and bladder mass biopsy under general anaesthesia. Intraoperative findings were solid mass lesion projecting in the posterior wall of the bladder with overlying mucosa intact. During surgery, the patient developed supraventricular tachycardia with ectopics and the Blood Pressure (BP) was 200/130 mmHg. Patient was reverted within 15 minutes. Postoperatively, patient’s recovery was uneventful. Histopathological examination showed tumour cells in zellballen pattern, surrounded by sustentacular cells in muscularis propria extending to serosa. Immunohistochemistry for synaptophysin, chromogranin, CD56 were positive in tumour cells and S100 positive for sustentacular cells. Serum metanephrines were normal, however, 24-hours urinary normetanephrines were found to be high. Magnetic Resonance Imaging (MRI) pelvis showed large lobulated mass lesions in the left posterolateral wall of the urinary bladder which appeared heterogeneously hyperintense on T2 weighted and isointense on T1 weighted images. The lesion involved the left seminal vesicle [Table/Fig-1].
Axial T2W1 imaging showing heterogenous hyperintense lesion approx. 4.2×3.4×3.4 cm lesion in the left posterolateral wall of the urinary bladder with left seminal vesicle involvement.
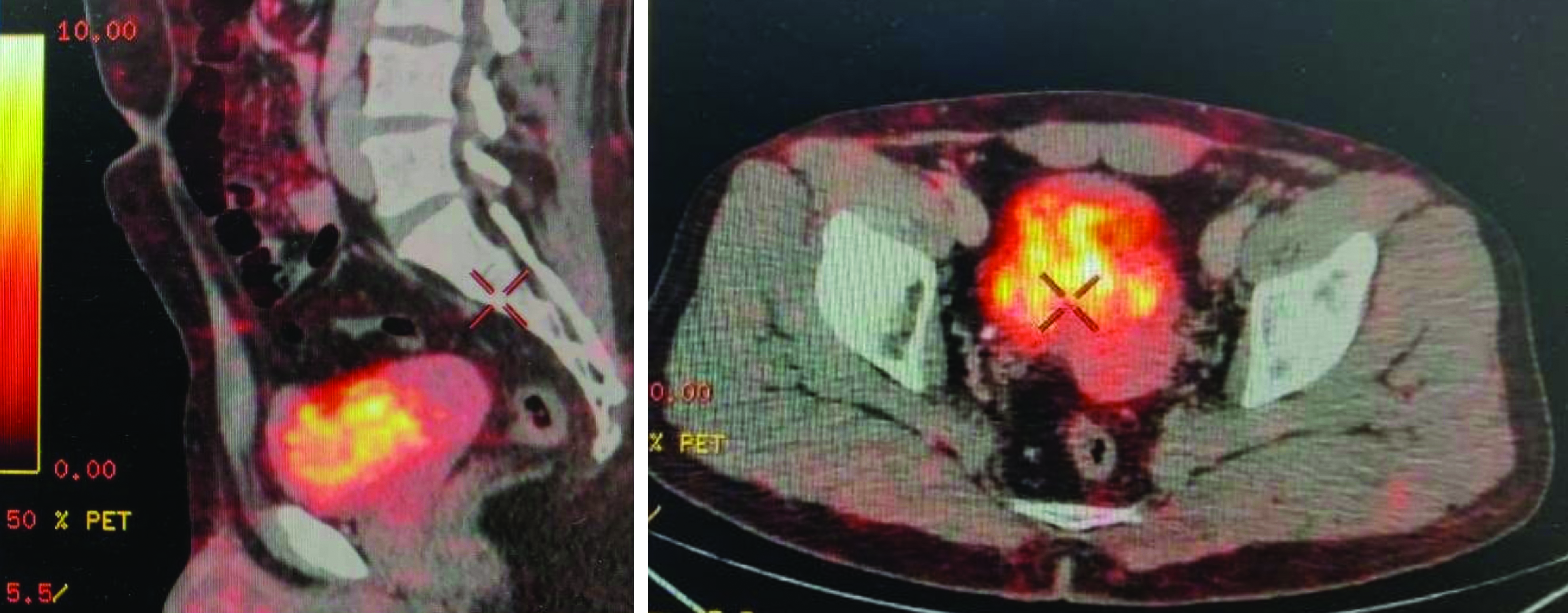
Patient underwent whole body 68Ga-Octreotide Dodecantetraacetic acid Nal3-Octreotide (DOTA NOC) Positron Emission Tomography (PET) scan which showed large DOTA NOC avid arterially enhancing exophytic soft tissue mass lesion involving left posterolateral wall of urinary bladder with infiltration into left seminal vesicle and close abutment of adjacent large bowel loops [Table/Fig-2]. No DOTA NOC avid lesion seen elsewhere in the body. In view of cT4b stage disease, the patient underwent robot-assisted radical cystectomy with intracorporeal ileal neobladder formation and bilateral pelvic lymphadenectomy after adequate alpha blockade. Standard technique with four robotic arms in a steep trendelenburg position was performed. Total operative time was 450 minutes and approx. blood loss during surgery was 250 mL. Patient had one episode of hypertension (BP was 190/110 mmHg) which was managed with intravenous nitroprusside. Immediate postoperative period was uneventful with haemodynamic stability. Pelvic drain was removed on the 5th postoperative day. Patient developed high grade fever on 8th postoperative day, ultrasound showed heterogenous collection in pelvis lateral to neobladder, which was aspirated, and patient became afebrile. Final histopathological report of radical cystectomy showed bladder paraganglioma with all margins free of tumour and negative nodal status [Table/Fig-3]. Patient is continent and asymptomatic at six-month follow-up. Urine normetanephrines levels were normal and no evidence of any recurrence was seen on imaging.
Sagittal and axial section of DOTA NOC PET scan showing DOTA avid large growth in the urinary bladder.
Microphotographs of H&E stained sections of urinary bladder mass show an encapsulated lesion with underlying zellballen pattern (star) separated by segmented bands of prominent fibrovascular network (a; 40x, b; 100x, c; 200x). These large polygonal cells have abundant granular eosinophilic cytoplasm and central nuclei with mild nuclear atypia (arrowheads d; 400x). Tumour cells show cytoplasmic immunopositivity for synaptophysin (arrowhead e; 200x).
Discussion
Paragangliomas are extra-adrenal neoplasms derived from neural crest cells. Genitourinary paragangliomas are rare and constitute less than 1% of all pheochromocytomas. Urinary bladder is the most common genitourinary organ involved by these tumours followed by the urethra, renal pelvis and ureter. Bladder paragangliomas are rare tumours accounting for approximately 0.06% of bladder tumours [1]. These are usually derived from embryonic rests of chromaffin cells in the detrusor sympathetic plexus.
The age range is wide at 10-78 years, with female preponderance. Most of these tumours are sporadic in nature, few cases can occur in settings of familial syndrome such as Von Hippel-Lindau, Multiple Endocrine Neoplasia Type 2, neurofibromatosis or tuberous sclerosis. Bladder paraganglioma can be functional (catecholamine secreting) or non-functional [2].
Symptomatic patients present with adrenergic symptoms of paroxysmal hypertension, headaches, palpitations or sweating with the act of micturition. Non-functional bladder paragangliomas are often diagnosed during resection of mass lesion that is found in routine imaging, leading to a potentially life-threatening cardiovascular event during surgery [3]. In present case, the patient was diagnosed incidentally as a case of bladder tumour during imaging for flank pain and had cardiovascular deterioration during the biopsy.
Paragangliomas are of mesenchymal origin and can occur at any location in the bladder wall. Leiomyoma, rhabdomyosarcoma and neurofibromatosis are various mesenchymal tumours, which can be considered as differential diagnosis. The variable symptomatic presentation, age predilection, invasiveness and different imaging characteristics help in distinguishing these tumours from paraganglioma. Mesenchymal tumours should also be differentiated from urothelial tumours. The former appear as intramural lesions with smooth margins and latter as irregular, pedunculated or sessile growth. Paragangliomas appear hyperintense on both T1 and T2-weighted images, whereas, urothelial carcinomas appear hypointense on T1-weighted images and intermediate signal intensity with early enhancement on T2-weighted images [4].
The diagnosis of bladder paraganglioma is dependent on both the functional status of tumour and the imaging. Tumours present in 60% cases with increased metabolites of catecholamines, however, these surges in blood levels of these amines can be transient with acts of micturition. The DOTA NOC PET and Iodine-123 Metaiodobenzylguanidine (MIBG) scan offer the advantage of identifying the functional tumours of neuroendocrine origin. 68Ga DOTA NOC PET/CT has a high accuracy of around 98% in identifying the neuroendocrine tumours and presently is the imaging modality of choice for staging [5].
These tumours are managed with surgical excision either with open approach or laparoscopic/robotic approach. The functional status of a tumour often presents a challenge in managing by minimal invasive approach. Options for definitive surgical resection of bladder paragangliomas include bladder preserving approaches such as Transurethral Resection (TUR) or partial cystectomy and bladder removal approaches such as radical cystectomy. Owing to the rare presentation and uncertain malignant potential of these tumours, there is little evidence in demonstrating the equivalence of bladder sparing surgeries and radical approaches. Therefore, an individualised case-based approach is warranted.
The anaesthetic considerations in robotic surgery of steep trendelenburg position and cardiopulmonary compromise due to pneumoperitoneum in functional tumours are also of paramount importance. Robotic surgery offers an opportunity to tackle the enlarged feeding vessels first, without any manipulation of the tumour. This case had only one episode of intraoperative hypertensive crisis and can be a feasible option in management of these tumours. The robot-assisted resection of a paraganglioma has been reported in many series [6]. This is the first case to report a robot-assisted radical cystectomy with intracorporeal ileal neobladder in locally advanced bladder paraganglioma.
The contemporary review of literature has suggested similar management approaches in locally advanced bladder paragangliomas, although few authors managed it with partial cystectomy. The uniqueness of the index case was the formation of intracorporeal neobladder following radical cystectomy using robotic assisted surgery; while majority of the surgeons used ileal conduit [7]. Despite long duration associated with the formation of intracorporeal neobladder, the patient had favourable intraoperative and postoperative outcomes. Robotic surgery, in authors experience, can be safely used in the management of these tumours.
Conclusion(s)
Being a rare entity with diverse clinical presentation, paragangliomas are challenging to diagnose and treat. The current case report stresses the safety and feasibility of minimal invasive surgery in locally advanced malignancy with minimum physiological and haemodynamic jeopardy.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 04, 2020
Manual Googling: Jan 16, 2021
iThenticate Software: Jan 20, 2021 (21%)
[1]. Beilan JA, Lawton A, Hajdenberg J, Rosser CJ, Pheochromocytoma of the urinary bladder: A systematic review of the contemporary literatureBMC Urol 2013 13(1):2210.1186/1471-2490-13-2223627260 [Google Scholar] [CrossRef] [PubMed]
[2]. Wong-You-Cheong JJ, Woodward PJ, Manning MA, Sesterhenn IA, From the Archives of the AFIP: Neoplasms of the urinary bladder-radiologic-pathologic correlationRadioGraphics 2006 26(2):553-80.10.1148/rg.26205517216549617 [Google Scholar] [CrossRef] [PubMed]
[3]. Lu H, Male M, Jiang K, Ye Z, Song D, Xia D, Clinical significance of functional and anatomical classifications in paraganglioma of the urinary bladderUrol Oncol 2019 37(6):35410.1016/j.urolonc.2019.01.02730799087 [Google Scholar] [CrossRef] [PubMed]
[4]. Loveys FW, Pushpanathan C, Jackman S, Urinary bladder paraganglioma: AIRP best cases in radiologic-pathologic correlationRadio Graphics 2015 35(5):1433-38.10.1148/rg.201514030326284302 [Google Scholar] [CrossRef] [PubMed]
[5]. Han S, Suh CH, Woo S, Kim YJ, Lee JJ, Performance of 68Ga-DOTA-conjugated somatostatin receptor-targeting peptide PET in detection of pheochromocytoma and paraganglioma: A systematic review and meta-analysisJ Nucl Med 2019 60(3):369-76.10.2967/jnumed.118.21170630030341 [Google Scholar] [CrossRef] [PubMed]
[6]. Alanee S, Williamson SR, Gupta NS, A rare case of non-functioning bladder paraganglioma treated with robotic assisted partial cystectomyUrol Case Rep 2019 26:10095010.1016/j.eucr.2019.10095031312604 [Google Scholar] [CrossRef] [PubMed]
[7]. Wang EY, Pak JS, Virk RK, Anderson CB, Healy KA, Lee JA, Bladder preservation for patients with bladder paragangliomas: Case series and review of the literatureUrology 2020 143:194-205.10.1016/j.urology.2020.04.09832437773 [Google Scholar] [CrossRef] [PubMed]