Impact of Electrotherapy or Muscle Training on Quality of Life in Urinary Incontinence of Male Geriatric Population- A Protocol
Ashish Wasudeorao Bele1, Mohd Irshad Qureshi2
1 Associate Professor, Department of Community Health Physiotherapy, Ravi Nair Physiotherapy College, DMIMS (DU), Wardha, Maharashtra, India.
2 Professor, Department of Neuro Physiotherapy, Ravi Nair Physiotherapy College, DMIMS (DU), Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mohd Irshad Qureshi, Professor, Department of Neuro Physiotherapy, Ravi Nair Physiotherapy College, DMIMS (DU), Sawangi (Meghe), Wardha-442004, Maharashtra, India.
E-mail: irshadphysio@rediffmail.com
Introduction
Urinary Incontinence (UI) is the involuntary loss of urine with social alienation, loss of sexual activity and other psychosocial issues which may affect the Quality of Life (QOL) and psychosocial well-being of patients. Electrotherapy may play an important role in the treatment of incontinence by means of stimulating the weakened structures which helps in control of micturition. Various electrotherapeutic currents including Faradic, Galvanic, Inferential Therapy (IFT), Russian currents along with the pelvic floor muscles strength training may be helpful in UI.
Aim
To find the impact of electrotherapy or training of muscle on QOL in male geriatric population of incontinence of urine.
Materials and Methods
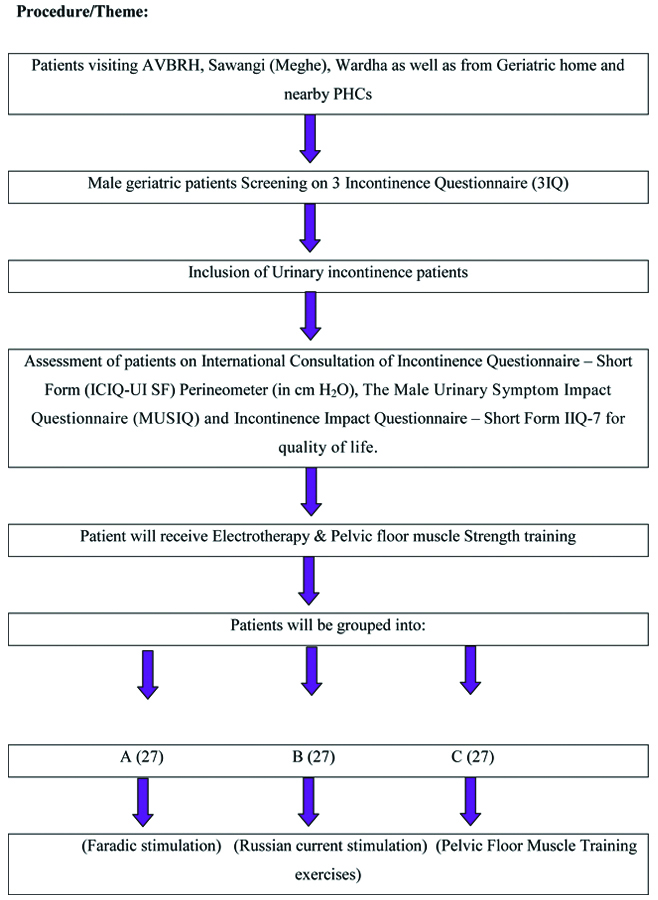
This randomised controlled trial will be carried out on geriatric male patients attending Acharya Vinoba Bhave Rural Hospital, Sawangi (Meghe), Wardha as well as on patients from geriatric homes and nearby PHCs. They will be screened for UI. The participants will be divided into three groups each of which will receive Faradic stimulation, Russian current stimulation and Pelvic Floor Muscle Training (PFMT) exercises respectively. The study will be carried out between October 2020 to October 2022. The data will be collected and analysed utilising inferential and descriptive statistics by using Chi-Square test and student’s t-test (unpaired and paired) and software for analysis will be SPSS 22.0 version and Graph pad prism 6.0 version and level of significance will be considered as p<0.05 and results will be obtained.
Conclusion
In male geriatric population, muscle strength training or electrotherapy can reduce urine incontinence.
Exercises, Faradic current, Men, Older adults, Russian current
Introduction
Urinary incontinence is a common disorder among elder people which is associated with dementia [1]. UI exists in 14% to 25% of older adults living in the community. The International Continence Society (ICS 1976) describes incontinence as “involuntary urine failure which is a social or hygienic issue and scientifically demonstrable” which involves urinary stress incontinence, urinary impulse incontinence, mixed UI, enuresis, nocturnal enuresis, persistent UI and certain forms [2]. The signs of incontinence are characterised by leakage detected during inspection and may be found as urethral or extraurethral [3].
The incidence of male UI is less than that of female [4]. It has been found that, average rate of incidence of the male UI is 3 to 11 percent [5]. Among all the types of UI in male, urge UI includes the symptoms of leakage combined with a forceful, frequently immediate, emergency to void and being found in 40 to 80 percent of patients [6]. Mixed UI is a leakage syndrome which includes the symptoms of both urge and stress UI. Symptoms of Stress UI are leakage, synonymous with elevated intra-abdominal pressure by sneezing, coughing or laughing; which accounts for less than 10% of incontinence. Male UI increases with age, which tends to rise more slowly than women [7]. UI induces social alienation, loss of sexual activity and other psychosocial issues; it may dramatically affect the QOL and psychosocial well-being of patients [8].
Conservative modalities to treat UI include physiotherapy, including PFMT along with or without Biofeedback (BFB), non-invasive Electrical Stimulation (ES) of pelvic floor [9]. Conservative treatment, in healthy and motivated individuals, require primarily bladder retraining and Pelvic Floor Rehabilitation (PFR) (BFB, pelvic floor exercises and ES), which is the first-line choice at the initial stage of treatment [10,11].
Electrotherapy plays an important role in the treatment of UI. Electrotherapeutic currents including Faradic, Galvanic, IFT have proved to be effective in the treatment of incontinence. ES is a choice of treatment for UI patients. Stimulation by Russian current has been widely used to improve strength of muscles in healthy athletes. Russian current encourages improved muscle strength and hypertrophy. Russian current was promoted for use in enhancing muscle strength [12-16].
Exercises of pelvic floor muscles are routine maximal voluntary contractions and relaxation. In order to have a conditioning impact, the muscles must be ‘overloaded’, i.e., they must act faster and/or consistent than they usually do. PFMT is intended to maximise muscle power and hypertrophy and thereby, increases urethral support and compression but, can required several months to accomplish this. This may decrease the amount of leaking but not necessarily the number of incontinence events. PFMT is often the center of PFR for affluent elderly people [11,17,18].
Most of the studies were on the prevalence and effect of management of UI on QOL. There are substantially lesser studies on rural men from India. Various studies [9-11] used a combination of PFMT and ES. The current study will introduce Russian current to stimulate pelvic floor muscles as it has a strengthening effect on muscles. The primary aim of this study is to find and compare the effect of electrotherapy and muscle training on QOL in UI geriatric population.
Materials and Methods
The randomised controlled trial will be conducted in Physiotherapy Department of Acharya Vinoba Bhave Rural Hospital and Ravi Nair Physiotherapy College, Sawangi (Meghe), Wardha, Maharashtra, India; Geriatric home and nearby PHCs by Doctor of Philosophy in Physiotherapy (PhD in Physiotherapy) scholar under the monitoring and guidance of PhD guide. This study will start from 1st October 2020. The study is approved by Institutional Ethics Committee of Datta Meghe Institute of Medical Sciences (Deemed to be University) with the letter number: IEC/May-2020/8791, dated 20th May 2020. The study will be started after explaining the nature of the study in participant’s language and an informed consent will be signed. Confidentiality regarding the identity and privacy of each participant will be maintained strictly.
Sample size calculation: The sample size for the present study was calculated by using formula:
The reported sample size was 81 which will be divided into three groups i.e., 27 participants in each group. The theme of conducting the study is shown in [Table/Fig-1].
Showing theme of conducting the current study.
The geriatric male participants with UI, which will be diagnosed on the basis of clinical assessment and 3 Incontinence Questionnaires (3IQ), above the age of 60 years will be included in the study. Participants with postprostatectomy, history of an uncontrolled hypertension, recent acute Myocardial Infarction, artificial pacemaker, bleeding from the urinary bladder or the digestive tract, polyuria, uncontrolled diabetes mellitus, urinary tract infection, neurologic conditions affecting coordination and balance will be excluded.
Data Collection Tools
All the study participants after fulfilling the inclusion criteria will be assessed by 3IQ, ICIQ-UI SF, Perineometer (in cm of H2O), MUSIQ and IIQ-7.
1. 3 Incontinence Questionnaire (3IQ) [19]
A 3IQ is brief, self-administered questionnaire which is used to distinguished stress, urge and mixed UI. It includes three questions which are based on the symptoms of types of UI.
2. Perineometer
To evaluate the Pelvic Floor Muscular Strength (PFMS) a Perineometer (Enraf-Nonius Myomed 134 - Version II) will be used. It is a device that measures the anal pressure (in cm of H2O), which is an indirect measure of the pelvic floor muscle strength. Along with assessment of pressure, it is also used in teaching the exercises of muscle of the pelvic floor hence, it is also called as Pressure feedback.
3. The International Consultation of Incontinence Questionnaire- Short Form (ICIQ-UI SF) [20]
ICIQ-SF consists of six items of which four items mainly rate the UI symptoms for past four weeks. The scores are taken from the 3, 4 and 5 items. A 1 and 2 items are demographic and the last item is self-diagnostic used to identify the UI type. The severity of urinary loss and QoL for UI is measured subjectively with the ICIQ-SF. Score ranges were 1 to 5 (slight), 6 to 12 (moderate), 13 to 18 (severe) and 19 to 21 (very severe).
4. The Male Urinary Symptom Impact Questionnaire (MUSIQ) [21]
The MUSIQ includes 32 items that exactly indicates level to which lower urinary tract symptoms affect the emotional status and the various functions, relationships and roles. The 4-point scale which ranges from 0 (not at all) to 3 (greatly) is used to record the responses.
5. Incontinence Impact Questionnaire-Short Form IIQ-7 [22]
IIQ-7 includes seven items, records the accidental urine loss that could affect the activities of individuals, their relationships and feelings. 1 and 2 items indicates physical activity; 3 and 4 items indicates travel; fifth item related with social/relationships; 6 and 7 items indicates emotional health. Item feedbacks obtain from assigned values of 0 (“not at all”), 1 (“slightly”), 2 (“moderately”) and 3 (“greatly”). Calculation is done by the item’s average score. The values range from 0 to 3 which are calculated by multiplying with 33, 1/3 to put scores on a scale of 0 to 100.
Statistical Analysis
The data will be collected and analyse utilising inferential and descriptive statistics by using Chi-Square test and Student’s t-test (unpaired and paired) and software for analysis will be SPSS 22.0 version and Graph pad prism 6.0 version and level of significance will be considered as p<0.05.
Discussion
Castronovo AD and Evelyn L, in their study showed that a physiotherapy program can improve or fully restore incontinence. ES modality and pelvic floor exercises in combination are effective in reduction of the UI symptoms [23].
Many studies utilise electrotherapy including ES for the strengthening of pelvic floor muscle in combination with pelvic floor muscle strength training exercises [11]. Also, studies used Russian current for the strengthening of muscles in athletes specially for larger muscles. Stimulation of Tibial-nerve has demonstrated success in the urge UI treatment [14]. Stimulation of sacral-nerve has also benefited in refractory cases [13-16].
PFMT is often center of PFR for affected elderly people [24]. A perineometer with BFB is also found to be effective in strengthening of pelvic floor muscles [25].
Electrotherapy Modalities and exercises also play an important role in postoperative complications in elderly populations [26,27]. Combination of electrotherapy with pelvic floor muscle exercises is generally used but there are no studies based on the individual effects of electrotherapy and exercises to strengthen pelvic floor muscles. There are no studies on the Russian current, which has strengthening effects for weakened pelvic floor. In the current study, all the modalities will be utilised individually and compare the effect [9-18].
This study aims to find out the effect of electrotherapy and muscle training in geriatric male UI population. This study intends to create awareness among patient, researcher and students and contribute to Evidence Based Physiotherapy.
Limitation(s)
The authors may face difficulty in following-up the patients as most of them will belong to rural areas. Social restrictions also may interfere in the outcome of the study.
Conclusion(s)
The study concluded probably that the electrical stimulation and muscle strength training will reduce the urinary incontinence symptoms of male geriatric population.
Author Declaration:
Financial or Other Competing Interests: As declared above
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 25, 2020
Manual Googling: Dec 02, 2020
iThenticate Software: Jan 25, 2021 (10%)
[1]. Hunskaar S, Ostbye T, Borrie MJ, The prevalence of urinary incontinence in elderly Canadians and its association with dementia, ambulatory function, and institutionalizationNorwegian Journal of Epidemiology 1998 8(2):177-82.10.5324/nje.v8i2.465 [Google Scholar] [CrossRef]
[2]. Tong YC, Diagnosis and treatment of geriatric urinary incontinenceIncont Pelvic Floor Dysfunct 2009 3(3):69-72. [Google Scholar]
[3]. Nitti VW, The Prevalence of Urinary IncontinenceRev Urol 2001 3(suppl 1):S2-06. [Google Scholar]
[4]. Keilman LJ, Urinary incontinence: Basic evaluation and management in the primary care officePrim Care Clin Office Pract 2005 32:699-722.10.1016/j.pop.2005.06.00316140124 [Google Scholar] [CrossRef] [PubMed]
[5]. Shamliyan TA, Wyman JF, Ping R, Wilt TJ, Kane RL, Male urinary incontinence: Prevalence, risk factors, and preventive interventionsRev Urol 2009 11(3):145-65. [Google Scholar]
[6]. Kuchel GA, Du Beau CE, Urinary incontinence in the elderly. American society of nephrologyGeriatric Nephrology Curriculum 2009 30:01-05. [Google Scholar]
[7]. Bhagwath G, Urinary incontinence in the elderlyIndian Academy of Clinical Medicine 2001 2(4):270-75. [Google Scholar]
[8]. Yo K, Lin SJ, Salmon JW, Bron MS, The impact of urinary incontinence on quality of life of the elderlyAm J Manag Care 2005 11:S103-11. [Google Scholar]
[9]. Rajkowska-Labon E, Bakula S, Kucharzewski M, Sliwiński Z, Efficacy of physiotherapy for urinary incontinence following prostate cancer surgeryBioMed Res Int 2014 2014:78526310.1155/2014/78526324868546 [Google Scholar] [CrossRef] [PubMed]
[10]. Ishigooka M, Hashimoto T, Izumiya K, Katoh T, Yaguchi H, Nakada T, Electrical pelvic floor stimulation in the management of urinary incontinence due to neuropathic overactive bladderFront Med Biol Eng 1993 5(1):01-10. [Google Scholar]
[11]. Yokoyama T, Nishiguchi J, Watanabe T, Nose H, Nozaki K, Fujita O, Comparative study of effects of extracorporeal magnetic innervation versus electrical stimulation for urinary incontinence after radical prostatectomyUrology 2004 63(2):264-67.10.1016/j.urology.2003.09.02414972468 [Google Scholar] [CrossRef] [PubMed]
[12]. Soni N, Sagdeo V, Rahule A, Role of interferential therapy along with pelvic floor exercises in the management of stress incontinenceJ Cont Med A Dent 2015 3(1):25-28.10.18049/jcmad/314 [Google Scholar] [CrossRef]
[13]. Caldwell KP, The electrical control of sphincter incompetenceLancet 1963 2(7300):174-75.10.1016/S0140-6736(63)92807-1 [Google Scholar] [CrossRef]
[14]. Heggannavar AB, Dharmayat SR, Nerurkar SS, Kamble SA, Effect of Russian current on quadriceps muscle strength in subjects with primary osteoarthritis of knee: a randomised control trialInt J Physiother Res 2014 2(3):555-60. [Google Scholar]
[15]. Lima EP, Rodrigues GB, Russian stimulation in strengthening abdominal muscleArq Bras Cir Dig 2012 25(2):125-28.10.1590/S0102-6720201200020001323381757 [Google Scholar] [CrossRef] [PubMed]
[16]. Ward AR, Shkuratova N, Russian electrical stimulation: The early experimentsPhysical Therapy 2002 82(10):1019-30.10.1093/ptj/82.10.101912350217 [Google Scholar] [CrossRef] [PubMed]
[17]. Choarelli PE, Kafe DRO, Physiotherapy for the pelyic floorAust J Physiother 1981 27(4):103-08.10.1016/S0004-9514(14)60750-9 [Google Scholar] [CrossRef]
[18]. Yamanishi T, Mizuno T, Watanabe M, Honda M, Yoshida KI, Randomized, placebo controlled study of electrical stimulation with pelvic floor muscle training for severe urinary incontinence after radical prostatectomyJ Urol 2010 184(5):2007-12.10.1016/j.juro.2010.06.10320850831 [Google Scholar] [CrossRef] [PubMed]
[19]. Brown JS, Bradley CS, Subak LL, The sensitivity and specificity of a simple test to distinguish between urge and stress incontinenceAnn Intern Med 2006 144(10):715-23.10.7326/0003-4819-144-10-200605160-0000516702587 [Google Scholar] [CrossRef] [PubMed]
[20]. Avery K, Donovan J, Peters T, Shaw C, Gotoh M, Abrams P, ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinenceNeurourol Urodyn 2004 23(4):322-30.10.1002/nau.2004115227649 [Google Scholar] [CrossRef] [PubMed]
[21]. Robinson JP, Shea JA, Development and testing of a measure of health-related quality of life for men with urinary incontinenceJ Am Geriat Soc 2002 50(5):935-45.10.1046/j.1532-5415.2002.50223.x12028184 [Google Scholar] [CrossRef] [PubMed]
[22]. Uebersax JS, Wyman JF, Shumaker SA, McClish DK, Fantl JA, the Continence Program for Women Research GroupShort forms to assess life quality and symptom distress for urinary incontinence in women: The incontinence impact questionnaire and the urogenital distress inventoryNeurourology and Urodynamics 1995 14:131-39.10.1002/nau.19301402067780440 [Google Scholar] [CrossRef] [PubMed]
[23]. Dowling-Castronovo A, Evelyn L, Urinary incontinence assessment in older adults: Part II - Established urinary incontinence. Best practices in nursing care to older adultsThe Hartford Institute for Geriatric Nursing. Revised 2018 (11.2) [Google Scholar]
[24]. Robinson JP, Avi-Itzhak T, McCorkle R, Psychometric properties of the Male Urogenital Distress Inventory (MUDI) and Male Urinary Symptom Impact Questionnaire (MUSIQ) in patients following radical prostatectomyUrologic Nursing 2007 27(6):512-18. [Google Scholar]
[25]. Kasatwar P, Bele A, Dhankar S, Naqvi W, Comparative study of effect of vaginal cones as a biofeedback device and pelvic floor exercises in rural females with urinary incontinenceJ Datta Meghe Inst Med Sci Univ 2020 15:36-39. [Google Scholar]
[26]. Darware M, Naqvi WM, A case report on Physiotherapy rehabilitation accelerating the recovery of older patient with anterior cruciate ligament reconstructionMedical Science 2020 24(103):1803-08. [Google Scholar]
[27]. Vaidya L, Kumar K, Naqvi W, Narang S, Pisulkar G, Dadlani M, Revision of total hip replacement surgery in elderly patient and its recovery based on periprosthetic fracture rehabilitationMedical Science 2020 24(104):2628-38. [Google Scholar]