Ocular Parameters Evaluation in Relation to the Refractive Error using Optical Coherence Topography
Farah Maqsood1, Menwah Al-Matrafi2, Nourah Al-Muaither3
1 Assistant Professor, Department of Optometry and Vision Science, King Saud University, Riyadh, Saudi Arabia.
2 Teaching Assistant, Department of Optometry and Vision Science, King Saud University, Riyadh, Saudi Arabia.
3 Optometry Doctor, Department of Optometry and Vision Science, King Saud University, Riyadh, Saudi Arabia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Farah Maqsood, King Saud University, Riyadh, Saudi Arabia.
E-mail: farahmaqsood@gmail.com; fmaqsood@ksu.edu.sa
Introduction
The increasing prevalence of myopia has become a major public health impact due to its potentially blinding ocular complications. This study was done to evaluate the choroidal and retinal thickness, depth of the anterior chamber and the curvature of the cornea using 3D Optical Coherence Topography (OCT) and Optical Coherence Biometry instrument (Zeiss IOLMaster 700) among Saudi female adults with emmetropia, low and moderate myopia.
Aim
To evaluate the choroidal thickness, foveal retinal thickness, depth of anterior chamber, Axial Length (AL) and curvature of the cornea between myopic and emmetropic individuals.
Materials and Methods
This cross-sectional study was done in the female section of Department of Optometry, College of Applied Medical Science, King Saud University (KSU), Riyadh, in Saudi Arabia. Hundred and four eyes of healthy females between the ages of 19-26 years who fulfilled the inclusion criteria were selected. There was no gender preference; only female subjects were included because this study was done in the female college. The subjects were categorised into emmetropic groups (Spherical Equivalent (SE) ≤ -0.25 D), mild myopic groups (SE between -0.50 to -3.00 D) and moderate myopic groups (SE between -3.00 to -6.00 D). The foveal retinal and subfoveal choroidal thickness was measured using 3D OCT, however AL, Anterior Chamber Depth (ACD) and corneal radius were measured using IOL master.
Results
The foveal retinal thickness of moderate myopia (205.55±15.35 μm) was found the same as in emmetropia (204.12±15.44 μm) and mild group (204.64±14.29 μm) with p>0.05. The significant difference was not found in the subfoveal choroidal thickness between these three groups. The mean AL of moderate myopia (25.03±0.75 mm) was significantly higher than mild myopia (23.99±0.74 mm) and emmetropia group (23.15±0.98 mm). There was highly significant difference in the ACD between the emmetropic and myopic groups. However, no significant difference was observed in the mean of corneal radius (K-reading) among the three groups (p>0.05). The corneal radius in total myopic eyes had a weak negative correlation with the AL.
Conclusion
This study demonstrated that the foveal retinal and subfoveal choroidal thickness did not differ significantly in emmetropic and myopic groups. Also, positive correlation was noted between the ACD and AL. Pearson’s correlation coefficient (r) in ACD and AL for emmetropic group was found 0.28 and 0.48 for the moderate myopic group.
Anterior chamber depth, Axial length, Choroidal thickness, Foveal thickness, Myopia
Introduction
Several pathological ophthalmic conditions like refractive error and glaucoma, cause ocular diseases and are dependent on ocular dimensions. A mismatch between the optical power and the AL of an eye causes the refractive error. Myopia may result from an eye being either too long or its optical components too powerful, leading to images of distant objects in front of the retina. On the contrary, hyperopia may result from an eye being either too short or its optical components not powerful enough, leading to images behind the retina. The abnormalities of ocular length, specifically of the vitreous chamber are the causes of most refractive errors. Myopia carries an increased risk of a number of sight-threatening ocular pathologies, including retinal detachment, choroidal neo vascularisation, cataracts, and glaucoma [1-5].
Extra elongation of the vitreous chamber in most myopia may be expected to have adverse effects for the structures making up the wall of the vitreous chamber, including the retina and choroid. These structural changes, as a product of excessive growth and stretching, would offer the increased risk of ocular pathology. Reports of a thinner nerve fiber layer and choroid in myopes are consistent with excessive stretch in these eyes [6-8]. In myopic eyes, the AL becomes longer than the normal length, and the sclera becomes thinner, especially at the posterior pole, and hence the retina may be stretched at the posterior pole in myopic eyes [9].
The ACD measurement should be taken carefully before refractive procedures that employ phakic or pseudo phakic Intraocular Lenses (IOL). Several factors like IOL power, AL, Postoperative Effective Lens Position (ELP), and corneal curvature define postoperative refraction [10-12]. This study was done to take empirical information about ocular parameters in relation to the refractive errors especially between emmertropia and mild and moderate categories of myopia.
Materials and Methods
The research followed the tenets of the Declaration of Helsinki and the project protocol was approved by Research Ethics Committee of King Saud University by this code-CAMS 024-37/38. Subjects using e-mail announcements were recruited from the student population of the King Saud University and the data collection was done in five months from January 2017 to May 2017 in Optometry clinics of College of Applied Medical Science, KSU.
Inclusion criteria: This study was done in the female section, so only female subjects were recruited. A total of hundred and four eyes of the healthy subjects were recruited age between 19-26 years (mean±SD: 20.05±1.24 years) and refractive errors.
Exclusion criteria: Participants with any history of the eye disease that could affect retinal or choroidal thickness, ocular pathology disease, glaucoma, corneal or lens opacities and prior ocular surgery or ocular trauma.
These 104 eyes were categorised into three groups based on the refractive errors, with 26 classified as emmetropic group (SE ≤ -0.25 D), 56 classified as low myopic group (SE between -0.50 to -3.00 D), and 22 classified as moderate myopic group (SE between -3.00 to -6.00 D) [13].
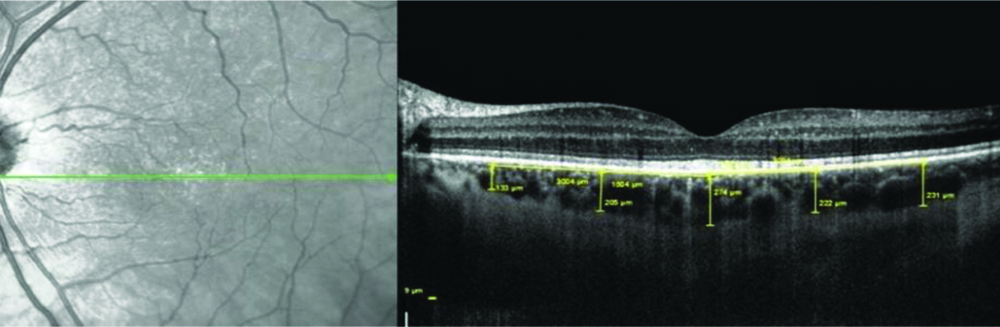
Visante™ Optical coherence tomography (ZEISS Visante OCT Model 1000, Carl Zeiss Meditec, Dublin, California, USA) was used to measure foveal retinal and subfoveal choroidal thickness because it includes infrared measurement light with major advantages of speed of image acquisition, noncontact, high resolution, and ease of operation. The AL, ACD and corneal radius were measured by IOL master Optical Coherence Biometry instrument (Zeiss IOLMaster 700). Combining performance with simplicity, the IOL Master quickly and accurately measures biometric parameters in a single location without ever touching the cornea. At the push of a button, AL, corneal curvature, White-to-White and ACD are quickly and precisely measured. Refraction for each eye was recorded with an automatic refractometer. All devices were calibrated according to manufacturer recommendations prior to undertaking the measurements. Measurements were performed by two independent and experienced optometrists, and the mean value was taken for the analysis. Pictures were excluded, if the discrepancy between the two optometrists was more than 10%. Visante™ OCT is designed for anterior segment imaging with the caliper measurement tool provided in the built-in analysis software which acquires multiple A-scans and creates a two dimensional image from them. The machine with 1050-nm-wavelength light source has a scanning speed of 100,000 A-scans per second. The 12-line radial scan pattern with a resolution of 1024×12 was used and an average of four overlapped consecutive scans gave each image, which covered an area of 12 mm×9 mm, centered on the fovea. The distance between the Bruch membrane and the choroid-sclera interface was measured as the choroidal thickness. Retinal thickness was measured as the distance between the internal limiting membrane and the interface between photoreceptor outer segments and retinal pigment epithelium. An example of choroidal thickness measurement using 3D-OCT is given in [Table/Fig-1].
Choroidal thickness measurement using 3D-OCT.
Statistical Analysis
The demographic data for all the subjects was analysed using Microsoft Excel 2013. Analysis of variance (ANOVA) has been used to find the significance of study parameters between three groups of subjects. The relation of ACD and K-reading with AL of the three groups and total myopia was analysed by Pearson’s sample correlation test (R). The p-value of less than 0.05 was considered statistically significant using Instat Graph Pad software version 3.10.32. (Instat Graph Pad SOFTWARE inc.).
Results
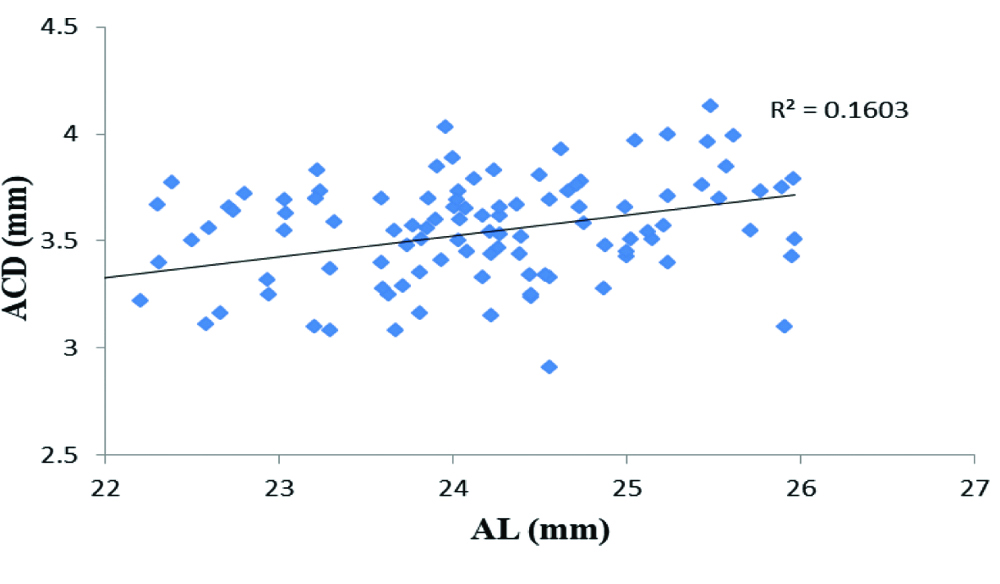
The mean foveal retinal thickness of moderate myopia was the same as in emmetropia and mild myopia group with p>0.05. There was no significant difference in the subfoveal choroidal thickness between the emmetropia (228.08±26.74 μm), mild myopia (223.70±18.25 μm) and moderate myopia group (228.09±17.59 μm). The mean of AL of moderate myopia (25.03±0.75 mm) was significantly higher than mild myopia (23.99±0.74 mm) and emmetropia group (23.16±0.98 mm). There was highly significant difference in the ACD between the emmetropia (3.21±3.21 mm) and moderate myopia (3.28±4.13 mm) groups. However, no significant difference was observed in the mean of corneal curvature (K-reading) among the three groups (p>0.05). The mean of foveal retinal thickness, subfoveal choroidal thickness, AL, ACD and K-reading are summarised in [Table/Fig-2]. In moderate myopic eyes, the ACD was significant and positively correlated with the AL and the values are given in [Table/Fig-3]. The Pearson’s correlation coefficient (r) was calculated by Pearson’s sample correlation test. The correlation between ACD versus AL is shown in [Table/Fig-4] and correlation coefficient for the graph was found 0.40.
Ocular Parameters (mean±standard deviation of foveal retinal thickness, subfoveal choroidal thickness, ACD, AL, K-reading).
| Parameters | Emmetropia group (n=26) | Mild myopia group (n=56) | Moderate myopia group (n=22) | p-value |
|---|
| Foveal retinal thickness (μm) | 204.12±15.44 | 204.64±14.29 | 205.55±15.35 | 0.946 |
| Subfoveal choroidal thickness (μm) | 228.08±26.74 | 223.70±18.25 | 228.09±17.59 | 0.584 |
| AL (mm) | 23.16±0.98 | 23.99±0.74 | 25.03±0.75 | 0.0001 |
| ACD (mm) | 3.21±3.21 | 3.10±4.03 | 3.28±4.13 | 0.0001 |
| K-reading (D) | 42.71±1.85 | 43.07±2.84 | 43.34±0.86 | 0.646 |
p-value of less than 0.05 was considered statistically significant using Instat Graph Pad software.
K-reading: Mean of corneal radius; AL: Axial length; ACD: Anterior chamber depth
Correlation between AL and ACD. For all analyses, statistical significance was defined as p<0.05.
| Axial length correlation with anterior chamber depth | Emmetropia group | Mild myopia group | Moderate myopia group |
|---|
| r | p-value | r | p-value | r | p-value |
|---|
| ACD | 0.28 | 0.18 | 0.21 | 0.126 | 0.48 | 0.023 |
ACD: Anterior chamber depth
Correlation between Anterior Chamber Depth (ACD) and Axial Length (AL) measured (r=0.40) with Intraocular Lenses (IOL) master (Zeiss IOL Master 700).
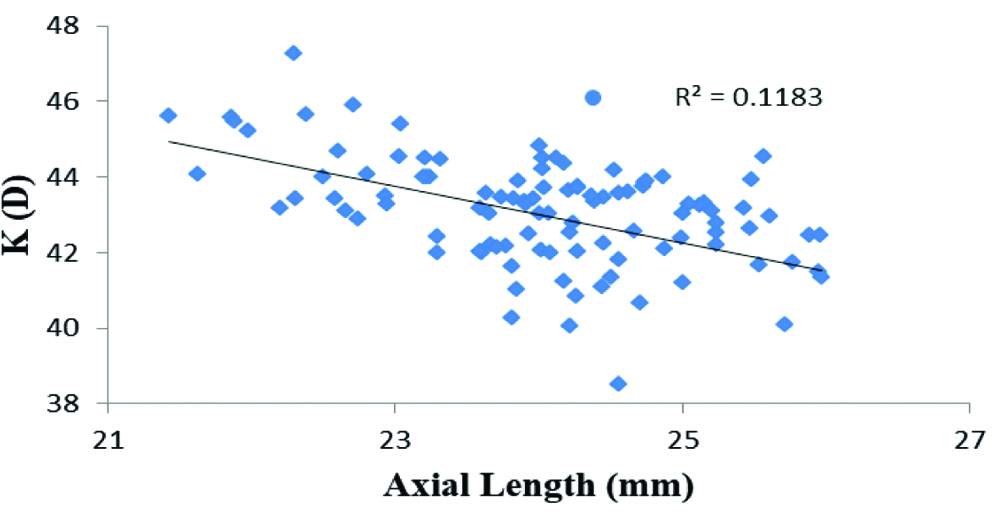
Furthermore, the corneal radius in total myopic eyes had a significantly negative correlation with AL as shown in [Table/Fig-5]. The corneal radius decreased with increasing AL.
Correlation between AL and K-reading. p-value <0.05 was considered statistically significant.
| Axial length correlation with corneal radius | Emmetropia group | Mild myopia group | Moderate myopia group |
|---|
| r | p-value | r | p-value | r | p-value |
|---|
| K-reading | -0.83 | 0.0001 | -0.375 | 0.0047 | -0.499 | 0.018 |
K-reading: Mean of corneal radius
The [Table/Fig-6] shows significant negative correlation (r=0.34) between the two parameters, AL and corneal radius in myopes i.e., axial elongation of eyeball tends to flatten the cornea.
Correlation between corneal radius (K reading) and Axial Length (AL) measured with 3D Optical Coherence Topography (OCT).
(r=0.34)
Discussion
The present study showed that the foveal retinal thickness in moderate myopia was not significantly thinner than the emmetropia and mild myopia groups. This was similar to the study done by Samuel NE and Krishnagopal S which showed that the average foveal thickness was similar in low and moderate myopia groups but increased in high myopia group [14]. A study done by Lim MCC et al., reported that various degrees of myopia did not show a significant effect on macular retinal thickness [15]. In contrast Song AP et al., found that the average foveal thickness was increased with an increase in degree of myopia [16]. In the foveal area, the absence of vasculature may lead to foveal pit. The intraocular pressure and ocular growth induced retinal stretch has less impact on the deformity of this foveal pit [17].
Also, this study showed that there was no significant relationship in subfoveal choroidal thickness between emmetropia and myopia groups (p=0.58). Likewise, in a previous study done by Lee K et al., found that both refractive error and AL did not correlate with choroidal thickness at all locations [18]. During the process of scleral stretching, choroidal layer may be stretched along with the sclera towards a temporal direction, while the retinal layer is less stretched, may be because retinal tissues are basically nervous tissues and do not regenerate in general, but sclera and choroid are vascular and connective tissues that are more prone to proliferation. In a study done by Mary HO et al., found that the choroidal thickness decreases with severity of myopia [7]. This difference may be due to older age of the subjects than the subjects included in this present study and the difference in the race, also present study did not have subjects with high degree of myopia. On comparing the AL between the three different groups, the moderate myopia showed greater AL compared with the emmetropia and mild myopia. The statistical significance between the AL of the three groups display a significant p-value (p=0.0001). This indicates that the AL increases with increasing degree of myopia. This is similar to a study done by Lisa AO et al., which stated that there was a significant linear relationship between AL and the degree of myopia [19]. Also, the same study showed the more myopic eye has deeper anterior chamber, which matches with present result that revealed a significant relation between the degree of myopia and the depth of anterior chamber. In contrast, there is no direct relationship between ACD and different degrees of myopia, which is more correlated to AL elongation. This was confirmed with a study done by Wagdy FM which showed that no correlation between ACD and degree of myopia in adult population [20]. In this study a significant correlation was found between anterior chamber and AL in moderate and total myopic eyes. This was similar to the study done by O’Donnell C et al., which demonstrated anterior chamber correlation with AL [21].
Limitation(s)
This study was limited by poor resolution of some images taken with OCT for subjects with poor fixation ability and also it did not include high myopia group. The current study population was only females, at the younger age group (19 to 26 years) and biased towards the low and moderate myopia. The number of subjects was small and hyperopic subjects were also not included. For more generalisable results, future studies on the similar design need to be planned with large number of subjects including hyperopia.
Conclusion(s)
In this study, the foveal retinal thickness of myopic and emmetropic eyes did not differ significantly. There was no significant relation found between myopic and emmetropic group. Also, there was a weak positive correlation between ACD and AL in total myopic eye. Moreover, there was a weak negative correlation between corneal radius and AL in total myopic eye.
p-value of less than 0.05 was considered statistically significant using Instat Graph Pad software.
K-reading: Mean of corneal radius; AL: Axial length; ACD: Anterior chamber depth
ACD: Anterior chamber depth
K-reading: Mean of corneal radius
Author Declaration:
Financial or Other Competing Interests: As declared above
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 01, 2020
Manual Googling: Dec 04, 2020
iThenticate Software: Dec 29, 2020 (20%)
[1]. Tornquist R, Stenkula S, Tornquist P, Retinal detachment. A study of a population-based patient material in Sweden 1971-1981. I. EpidemiologyActa Ophthalmol (Copenh) 1987 65(2):213-22.10.1016/0002-9394(81)90170-7 [Google Scholar] [CrossRef]
[2]. Hotchkiss ML, Fine SL, Pathologic myopia and choroidal neovascularisationAm J Ophthalmol 1981 91(2):177-83. [Google Scholar]
[3]. Pan CW, Cheung CY, Aung T, Cheung CM, Zheng YF, Wu RY, Differential associations of myopia with major age-related eye diseases: The Singapore Indian Eye StudyOphthalmology 2013 120(2):284-91.10.1016/j.ophtha.2012.07.06523084122 [Google Scholar] [CrossRef] [PubMed]
[4]. Kanski Jack J, Brad B, Ken KN, Pearson A, Clinical ophthalmology: A systematic approach 2011 7th edEdinburgh; New YorkElsevier/Saunders [Google Scholar]
[5]. Flitcroft DI, The complex interactions of retinal, optical and environmental factors in myopia aetiologyProg Retin Eye Res 2012 31(6):622-60.10.1016/j.preteyeres.2012.06.00422772022 [Google Scholar] [CrossRef] [PubMed]
[6]. Zhao L, Wang Y, Chen CX, Xu L, Jonas JB, Retinal nerve fibre layer thickness measured by Spectralis spectral-domain optical coherence tomography: The Beijing Eye StudyActa Ophthalmologica 2014 92:e35-41.10.1111/aos.1224023981513 [Google Scholar] [CrossRef] [PubMed]
[7]. Mary HO, David TLL, Vesta CKC, Dennis SCL, Choroidal thickness measurement in myopic eyes by enhanced depth optical coherence tomographyOphthalmol 2013 120(9):1909-14.10.1016/j.ophtha.2013.02.00523683921 [Google Scholar] [CrossRef] [PubMed]
[8]. Vincent SJ, Collins MJ, Read SA, Carney LG, Retinal and choroidal thickness in myopic anisometropiaInvest Ophthalmol Vis Sci 2013 54:2445-56.10.1167/iovs.12-1143423482471 [Google Scholar] [CrossRef] [PubMed]
[9]. Wakitani Y, Sasoh M, Sugimoto M, Ito Y, Macular thickness measurements in healthy subjects with different axial lengths using optical coherence tomographyRetina 2003 23(2):177-82.10.1097/00006982-200304000-0000712707596 [Google Scholar] [CrossRef] [PubMed]
[10]. Holladay JT, Prager TC, Chandler TY, Musgrove KH, Lewis JW, Ruiz RS, A three-part system for refining intraocular lens power calculationsJournal of Cataract and Refractive Surgery 1988 14(1):17-24.10.1016/S0886-3350(88)80059-2 [Google Scholar] [CrossRef]
[11]. Hosny M, Alio JL, Claramonte P, Attia WH, Perez-Santonja JJ, Relationship between anterior chamber depth, refractive state, corneal diameter, and axial lengthJournal of Refractive Surgery 2000 16(3):336-40.10.3928/1081-597X-20000501-0710832983 [Google Scholar] [CrossRef] [PubMed]
[12]. Olsen T, Prediction of the effective postoperative (intraocular lens) anterior chamber depthJournal of Cataract and Refractive Surgery 2006 32(3):419-24.10.1016/j.jcrs.2005.12.13916631049 [Google Scholar] [CrossRef] [PubMed]
[13]. David AG, Theodore PG, Jeffrey TK, Wendy Marsh-Tootle, Thomas TN, Karla Z, Care of the patient with myopia, optometric clinical practice guidelineAmerican Optometric Association 2006 https://www.aoa.org/AOA/Documents/Practice%20Management/Clinical%20Guidelines/Consensus-based%20guidelines/Care%20of%20Patient%20with%20Myopia.pdf [Google Scholar]
[14]. Samuel NE, Krishnagopal S, Foveal and macular thickness evaluation by spectral OCT SLO and its relation with axial length in various degree of myopiaJournal of Clinical and Diagnostic Research 2015 9(3):01-04.10.7860/JCDR/2015/11780.567625954643 [Google Scholar] [CrossRef] [PubMed]
[15]. Lim MCC, Hoh ST, Foster PJ, Lim TH, Chew SJ, Seah SKL, Use of optical coherence tomography to assess variations in macular retinal thickness in myopiaInvestigative Ophthalmology & Visual Science 2005 46(3):974-78.10.1167/iovs.04-082815728555 [Google Scholar] [CrossRef] [PubMed]
[16]. Song AP, Wu XY, Wang JR, Liu W, Sun Y, Yu T, Measurement of retinal thickness in macular region of high myopic eyes using spectral domain OCTInternational Journal of Ophthalmology 2014 7(1):122-27. [Google Scholar]
[17]. Dubis AM, Mcallister JT, Carroll J, Reconstructing foveal pit morphology from optical coherence tomography imagingBr J Ophthalmol 2009 93(9):1223-27.10.1136/bjo.2008.15011019474001 [Google Scholar] [CrossRef] [PubMed]
[18]. Lee K, Junwon L, Christopher SL, Sun YP, Sung CL, TaekJune L, Topographical variation of macular choroidal thickness with myopiaActa Ophthalmologica 2015 93(6):e469-74.10.1111/aos.1270125752626 [Google Scholar] [CrossRef] [PubMed]
[19]. Lisa AO, Jill Y, Christine FW, Refractive error and ocular parameters: Comparison of two SD-OCT SystemsOptom Vis Sci 2015 92(4):437-46.10.1097/OPX.000000000000055925785537 [Google Scholar] [CrossRef] [PubMed]
[20]. Wagdy FM, Relationship between central corneal thickness, anterior chamber depth and degree of myopia in adultLife Science Journal 2013 10(3):184-86. [Google Scholar]
[21]. O’Donnell C, Hartwig A, Radhakrishnan H, Correlations between refractive error and biometric parameters in human eyes using the LenStar 900Cont Lens Anterior Eye 2011 34(1):26-31.10.1016/j.clae.2010.10.00621081280 [Google Scholar] [CrossRef] [PubMed]