Diffuse Idiopathic Skeletal Hyperostosis: An Anatomical Case Report
Anjali Singal1, Tulika Gupta2, Daisy Sahni3
1 Assistant Professor, Department of Anatomy, All India Institute of Medical Sciences, Bathinda, Punjab, India.
2 Associate Professor, Department of Anatomy, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
3 Professor and Head, Department of Anatomy, Post Graduate Institute of Medical Education and Reseacrh, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Tulika Gupta, Associate Professor, Department of Anatomy, Post Graduate Institute of Medical Education and Research, Chandigarh, India.
E-mail: sktulika@yahoo.com
Diffuse Idiopathic Skeletal Hyperostosis (DISH) is a noninflammatory disease of unknown cause characterised by osteophytic calcification or ossification of ligaments and enthesis; especially spinal. Authors hereby present a case report of a 65-year-old male cadaver, in whom the fusion of contiguous nine vertebrae from fifth thoracic to first lumbar vertebrae, because of ossification of the Anterior Longitudinal Ligament (ALL) was noticed. The tenth and eleventh thoracic vertebrae seemed to be affected worse, as maximum osseous anterior outgrowth (12 mm) of ossified ALL, ossification of Ligamentum Flavum (LF) and supraspinous ligament was also observed at this level. The Ossification of Anterior Longitudinal Ligament (OALL) along with the involvement of LF has not been classically reported. Ossification of spinal ligaments may cause local thoracic pain, stiffness and slowly progressive myelopathy. Ossified LF at the level of joint between tenth and eleventh thoracic vertebrae may result in compression of spinal cord at this level.
Anterior longitudinal ligament, Ligamentum flavum, Ossification
Case Report
During routine examination of dry and processed vertebrae in osteology section of Anatomy Department, a specimen with fusion of contiguous nine vertebrae from fifth thoracic (T5) to first lumbar (L1) vertebrae was observed [Table/Fig-1a-c]. The fusion was because of continuous type of OALL along with ossification of LF at the joint between tenth (T10) and eleventh thoracic (T11) vertebrae. The fusion between spine of T11 and T12 was also noticed. The specimen belonged to a 65-year-old male. Following observations were made, tabulated and analysed.
Ossified anterior longitudinal ligament. (a) Anterior view of fused vertebrae from fifth thoracic to first lumbar (T5- L1), (b) Left lateral view, (c) Right lateral view.
OAAL: Ossified anterior longitudinal ligament; *: Maximum anterior extent of bony outgrowth at the level of disc between tenth and eleventh thoracic vertebrae

Bodies of vertebrae: No direct fusion between bodies of vertebrae was observed, however they seemed to be fused because of continuous type of OALL, which extended more towards right lateral side (31-42 mm) as compared to left lateral side (7-32 mm) from midline [Table/Fig-1b,1c,2]. The OALL was more thick and nodular type at the level of intervertebral discs as compared to that in front of bodies of vertebrae. The bony outgrowth extension ranged anteriorly from 1 to 12 mm at different intervertebral levels, being highest at the level of disc between T10 and T11 [Table/Fig-1a,2]. No ossification was noted for posterior longitudinal ligament at any level.
The anterior and lateral extent of ossification of the anterior longitudinal ligament at different intervertebral levels.
| Intervertebral disc level | Anterior extent of bony outgrowth (mm) | Right extent of bony outgrowth from midline (mm) | Left extent of bony outgrowth from midline (mm) |
|---|
| T5-T6 | 1 | 31 | 10 |
| T6-T7 | 1 | 35 | 7 |
| T7-T8 | 1.5 | 35 | 13 |
| T8-T9 | 3 | 34 | 25 |
| T9-T10 | 5 | 32 | 28 |
| T10-T11 | 12 | 34 | 18 |
| T11-T12 | 4 | 35 | 32 |
| T12-L1 | 5 | 42 | 14 |
Laminae of vertebrae: Ossified LF was observed between lamina of T10 and T11 [Table/Fig-3a,b].
(a): Ossified ligamentum flavum between tenth and eleventh thoracic vertebrae and fusion of spines of eleventh and twelfth thoracic vertebrae (as marked in black circle) (b): Zoomed In view of ligamentum flavum.
OLF: Ossified Ligamentum flavum; T10: Tenth thoracic vertebra; T11: eleventh thoracic vertebra; T12: Twelfth thoracic vertebra; Sp11: Spine of eleventh thoracic vertebra; Sp12: Spine of twelfth thoracic vertebra
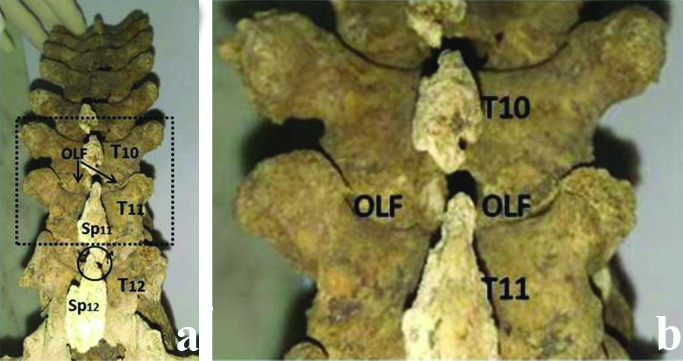
Spines of vertebrae: Fusion between spines of T11 and T12 observed [Table/Fig-3a].
Intervertebral disc space, intervertebral foramina, vertebral canal and zygophyseal joints: were normal.
Discussion
Diffuse Idiopathic Skeletal Hyperostosis or Forestier disease, is an idiopathic rheumatological disease involving ossification of ligaments and enthesis throughout the body, especially the ALL of spine [1]. ALL is a strong band extending along anterior surfaces of vertebral bodies, attached to the basiocciput, it extends from first cervical to upper sacrum [2]. The present observation of OALL on anterior aspect of lowers eight thoracic and first lumbar vertebral bodies, with maintained intervertebral disc space, favoured diagnosis of DISH.
The cases of OALL have been reported at different thoracic and lumbar levels previously [1,3,4]. Its incidence has been reported as 28.4%, however only 2% vertebral columns showed continuous type of ossification [4]. In the present case, fusion of contiguous nine vertebrae from T5 to L1 vertebrae because of ossification of ALL along with ossification of LF at the joint between T10 and T11 vertebrae and fusion between the spine of T11 and T12 was observed. The involvement of LF in DISH, has not been reported earlier as per the best of our knowledge [1,3,4].
Though it commonly affects males with age of 60 years or above, it has also been reported in individuals of 25 to 30 year of age or even in paediatric population [1,5]. The present case belonged to a male of 65 years of age. The most common symptoms of OALL are compression of oesophagus and trachea [6,7]. In a previous report of DISH with cervical involvement and dysphagia, the patient experienced substantial improvement in symptoms after excision of cervical osteophytes [8]. Though neurological complications from OALL are rare however spinal cord compression and peripheral nerve involvement have been reported [1]. The ossification of spinal ligaments results in loss of flexibility causing mild to moderate restricted spinal movements and lower back ache if a spinal nerve becomes irritated [1].
OALL produces a tortuous paravertebral mass anterior to and distinct from vertebral bodies. In thoracic spine involved by DISH, bridging ossifications are often appreciated along right lateral aspect of the thoracic spine and not on the left lateral aspect, probably related to an impeding effect on ossification by pulsation of descending thoracic aorta [9,10] whereas the patients with situs-inversus develop flowing ossifications on the left side [10]. In the present case the extent of ossification on the right side varied from 31 to 42 mm from midline in contrast to 7 to 32 mm on the left side [Table/Fig-2], indicating more movement restriction on the right lateral side of vertebral column as compared to left. This may also make the structures on the right side of midline more prone to be affected. According to literature ALL is more thick and narrow opposite vertebral bodies than at the levels of intervertebral symphyses, however in the present case more thick and nodular bone formation was observed at level of intervertebral disc [2]. It might be due to the fact that spinal movements occur at intervertebral disc space, which might induce more ossification at this level. The osseous extensions commonly range from 1 to 2 mm, however, may reach even up to 30 mm [6]. In the present case, the osseous outgrowth extended anteriorly from 1 to 12 mm at different intervertebral levels, being highest at the level of disc between tenth and eleventh thoracic vertebrae (12 mm). Over time, these osseous growths steadily lengthen and extend, crossing intervertebral space. They are most frequently detected at the lower margin of the vertebral bodies and grow inferiorly [6].
No significant thoracic disk space narrowing was observed; however as mentioned in previous literature about the rare ossification between the spinous processes, fusion only between tips of spines of T11 and T12 was noticed in present case [10]. This fusion indicates the ossification of only the deepest fibres of supraspinous ligament, which connect the adjacent spines [2]. The spinal nerve and spinal cord compression has rarely been reported in cases of DISH [1]. In the present case, intervertebral foramina and vertebral canal were found to be normal showing no osteogenesis.
The LF connects two adjoining laminae at the posterior side of the dura mater and both side flaps are separated at the midline [11]. The predilection sites for ossification of this ligament are the lower thoracic, followed by high thoracic and mid thoracic areas. The most common site is between T10 and T11, as was also found in the present case [12]. It is assumed that when the tensile strength increases, expression of Bone Morphogenetic Protein (BMP-2), Transforming Growth Factor (TGF-β) and Vascular Endothelial Growth Factor (VEGF) are elevated in LF, which is key marker of chondrogenesis [13].
In present case, T10 and T11 seemed to have been affected worse, as maximum osseous anterior outgrowth (12 mm) and ossification of LF was noticed at this level. The fusion of spines was also observed between T11 and T12. It might be due to the fact that these segments receive the maximum tensile stress.
Clinical implications: The ossification of spinal ligaments may cause friction between the joints of vertebrae, resulting in reduced vertebral column flexibility, making it prone to vertebral fracture. To strengthen bones and to bear the friction generated, bony spurs may be formed. As bone spurs increases in size, they can protrude into surrounding structures and can cause pain. The bone spurs in thoracic region can compress esophagus or rarely larynx, bronchus, trachea and inferior vena cava causing discomfort in the center of back, behind the rib cage. The spinal nerve roots may also get compressed resulting in myelopathy [1].
Conclusion(s)
As DISH may cause various skeletal and extra skeletal symptoms, the knowledge of this anatomical variation would be useful for the clinicians to interpret different clinical conditions.
Author Declaration:
Financial or Other Competing Interests: No
Was informed consent obtained from the subjects involved in the study? No
For any images presented appropriate consent has been obtained from the subjects. No
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 08, 2020
Manual Googling: Dec 17, 2020
iThenticate Software: Jan 23, 2021 (10%)
[1]. McCafferty RR, Harrison MJ, Tamas LB, Larkins MV, Ossification of the anterior longitudinal ligament and Forestier’s disease: An analysis of seven casesJ Neurosurg 1995 83(1):13-17.10.3171/jns.1995.83.1.00137782829 [Google Scholar] [CrossRef] [PubMed]
[2]. Standring S, Borley NR, Collins P, Crossman AR, Gatzoulis MA, Healy JC, Gray’s anatomyThe anatomical basis of clinical practice 2008 40th EdNew YorkChurchill Livingstone:728-29. [Google Scholar]
[3]. Mizuno J, Nakagawa H, Song J, Symptomatic ossification of the anterior longitudinal ligament with stenosis of the cervical spine: A report of seven casesJ Bone Joint Surg [Br] 2005 87-B:1375-79.10.1302/0301-620X.87B10.1674216189311 [Google Scholar] [CrossRef] [PubMed]
[4]. Kosuri KC, Venumadhav N, Ks S, Ossified ligamentum longitudinal anterius in adult human dry vertebraeJ Clin Diagn Res 2014 8(8):AC04-06.10.7860/JCDR/2014/8691.470225302180 [Google Scholar] [CrossRef] [PubMed]
[5]. Coakley FV, Vive J, Finlay DB, Shannon RS, Childhood ossification of the anterior longitudinal ligament of the cervical spineClin Radiol 1995 50(2):115-16.10.1016/S0009-9260(05)82993-9 [Google Scholar] [CrossRef]
[6]. Resnick D, Shaul SR, Robins JM, Diffuse idiopathic skeletal hyperostosis (DISH): Forestier’s disease with extraspinal manifestationsRadiol 1975 115(3):513-24.10.1148/15.3.5131129458 [Google Scholar] [CrossRef] [PubMed]
[7]. Bakker JT, Kuperus JS, Kuijf HJ, Õner FC, de Jong PA, Verlaan JJ, Morphological characteristic of diffuse idiopatic skeletal hyperosteosis in the cervical spinePLoS One 2017 12:e018841410.1371/journal.pone.018841429155874 [Google Scholar] [CrossRef] [PubMed]
[8]. Iplikcioglu AC, Karabag H, Diffuse idiopathic skeletal hyperostosis causing dysphagia: A case reportJ Clin Exp Orthop 2018 4(1):5510.4172/2471-8416.100055 [Google Scholar] [CrossRef]
[9]. Forestier J, Lagier R, Ankylosing hyperostosis of the spineClin Orthop Relat Res 1971 74:65-83.10.1097/00003086-197101000-000094993095 [Google Scholar] [CrossRef] [PubMed]
[10]. Belanger TA, Rowe DE, Diffuse idiopathic skeletal hyperostosis: Musculoskeletal manifestationsJ Am Acad Orthop Surg 2001 9(4):258-67.10.5435/00124635-200107000-0000611476536 [Google Scholar] [CrossRef] [PubMed]
[11]. Ahn DK, Lee S, Moon SH, Boo KH, Chang BK, Lee JI, Ossification of the Ligamentum FlavumAsian Spine J 2014 8(1):89-96.10.4184/asj.2014.8.1.8924596612 [Google Scholar] [CrossRef] [PubMed]
[12]. Park BC, Min WK, Oh CW, Jeon IH, Kim SY, Kyung HS, Surgical outcome of thoracic myelopathy secondary to ossification of ligamentum flavumJoint Bone Spine 2007 74(6):600-05.10.1016/j.jbspin.2007.01.03317888708 [Google Scholar] [CrossRef] [PubMed]
[13]. Yayama T, Uchida K, Kobayashi S, Kokubo Y, Sato R, Nakajima H, Thoracic ossification of the human ligamentum flavum: Histopathological and immunohistochemical findings around the ossified lesionJ Neurosurg Spine 2007 7(2):184-93.10.3171/SPI-07/08/18417688058 [Google Scholar] [CrossRef] [PubMed]