Ischemic heart disease is the single highest contributor to mortality and the burden of Acute Coronary Syndrome (ACS) in India is high in all parts of the country [1,2]. Coronary Angiograms (CAG) form the first line of management for most cases of ACS. The traditional access for percutaneous coronary interventions is the femoral route. A newer advance in the recent decades is the radial route [3]. In a recent study by Alkatiri AA et al., there was a reduction in mortality in the radial artery access group [3]. While the differences between the two methods have not been established conclusively, one meta-analysis [4] suggests that the radial route should be preferred.
Hence, the authors would like to report their experience with the DRA access for coronary angiography. This study was performed with the objectives to describe the success rate at achieving DRA puncture, the complications associated with DRA puncture technique in patients undergoing coronary angiography and the association of the factors (age, gender and other co-morbidities) with success in radial artery puncture.
Materials and Methods
This study was a hospital-based single centre retrospective observational study conducted at Vydehi Institute of Medical Sciences and Research Centre. Institutional Ethics Committee approval was obtained prior to the study. A total of 150 patients who were admitted for the performance of a CAG, and who underwent the angiogram by the DRA technique were included in the study. The case details of those fulfilling the inclusion criteria were accessed and details were noted. Data was collected in a pre-tested proforma from patients who underwent angiogram between August 2018 and March 2019.
Inclusion criteria: Patient included were above the age of 18 years, admitted for CAG, for ACS, chronic stable angina, recent STEMI and NSTEMI.
Exclusion criteria: Pre-procedure assessment was carried out and those with following conditions were excluded; Raynaud’s disease, upper limb vascular disorders, patients with neural disorders of radial nerve innervation area (for trans-snuff box), patients with chronic tenosynovitis, osteomyelitis, patients with marked deformities of hand, patients with recent fracture of scaphoid bone (for snuff box approach) and patients with ulnar tunnel (Guyon’s canal) syndrome.
Radial Artery Anatomy
Distally the radial artery [Table/Fig-1] gives rise to palmar carpel branch which anastamoses with similar branch arising from the ulnar artery and it gives rise to superficial palmar branch which passes through the thenar muscles, anastamosing with end of the ulnar artery to complete the superficial palmar artery. The radial artery, passes on the dorsum of wrist in between the tendon of extensor pollicis longus and tendons of abductor pollicis longus and extensor pollicis brevis, over the scaphoid and trapezium bone in the ASB. Further the radial artery runs medially between the heads of the first dorsal interosseous muscle into the palm where it anastamosis with the deep branch of ulnar artery completing the deep palmar arch. Sometimes the superficial palmar arch may be incomplete whereas, deep palmar arch is complete in most cases.
Anatomical Snuff Box (ASB).
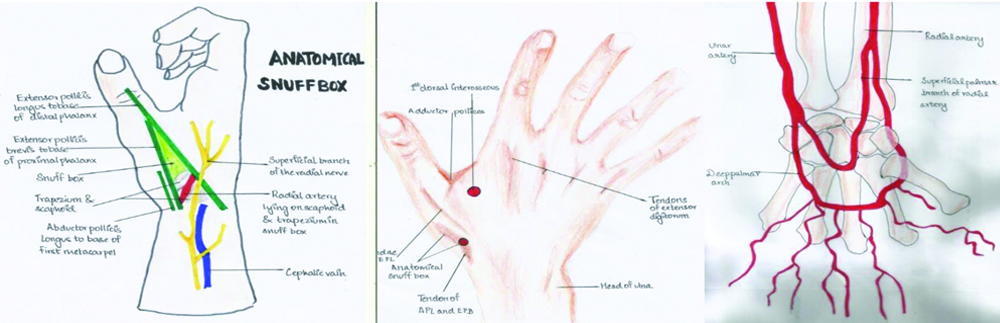
As the branches are already given in ASB, any occlusion at DRA puncture site could avoid flow interruption in radial and ulnar arteries in the forearm. Haemostasis was achieved in 2-3 hours in all patients. Early haemostasis is explained by smaller diameter of the artery, compression of the artery against scaphoid and trapezius bones.
Description of the technique: After positioning of the patient, 1 mg of diazepam was given before starting the procedure. Radial artery was punctured at anatomical snuffbox using 23G needle [Table/Fig-2a] and 0.032′ guide wire (Termoric) was inserted [Table/Fig-2b]. The procedure was done using 5-F sheath as shown in [Table/Fig-2c] (also shown in the [Videos-1,2]). After sheath insertion, cocktail containing 5 mg diltiazem, and 100 IU/kg unfractionated heparin was injected. Nitroglycerin was used as SOS. The average puncture time was noted. Further procedure was similar to radial angiogram. Radial sheath was removed just after procedure and compression was done for 6 hours. Successful puncture was defined as with a good jet of blood, insertion of sheath wire followed by sheath insertion with backflow. If any of these were absent, it was considered a “failed DRA puncture”.
a) Puncture of Distal Radial Artery (DRA); b) Wire insertion; c) Sheath placement.

The following parameters were noted:
Intra-procedure
Ability to puncture: Yes or No
Complications: No complications/Severe spasm/Poor Jet/Failed to cannulate
Fluoroscopic time
Postprocedure: Pulse examination was done and any abnormality was noted.
All the patients were examined daily for any access site complication such as hematoma, occlusion of radial artery or radial nerve injury [Videos-1,2].
Statistical Analysis
Data entry was done in Microsoft excel and analysis was carried out using SPSS version 22.0 (IBM). Demographic variables were expressed as means, Standard Deviation (SD), frequency and percentages. A 2×2 tables were created and Fisher’s-exact test was performed to look for significance.
Results
All the requisite data was available in all the patients that were studied.
Characteristics of the patients: The average age (±SD) of the population was 55.07±9.256 years. There were 19 females and 131 males in this study, and the age distribution of both the genders is presented in [Table/Fig-3]. The average age (±SD) of the males was 55.4±9.49 years, which was more than that of the females (52±7.88 years). There were 11 patients less than 40 years of age, and all were males. There was a preponderance of males more than 50 years in this study.
| Age group (in years) | Females Number (% of total females) | Males Number (% of total males) |
|---|
| 21-40 | 0 | 11 (8.4) |
| 41-50 | 7 (36.8) | 28 (21.4) |
| 51-60 | 10 (52.6) | 53 (40.5) |
| >61 | 2 (10.5) | 39 (29.8) |
| Total | 19 | 131 |
Description of clinical parameters: [Table/Fig-4] shows the clinical parameters of the patient, blood pressure, Dose Area Product (DAP), fluorotime, puncture time and Cumulative Air Kerma.
Clinical parameters of the patients.
| Variables | Mean | Standard deviation | Median | 95% CI (Lower bound-Upper bound) |
|---|
| Age (years) | 55.07 | 9.256 | 55.0 | 53.58-56.57 |
| Systolic BP (mmHg) | 132.25 | 18.94 | 130 | 129.19-135.3 |
| Diastolic BP (mmHg) | 77.99 | 8.597 | 80 | 76.6-79.37 |
| Mean arterial pressure | 96.07 | 10.06 | 96.5 | 94.44-97.69 |
| Fluorotime | 3.88 | 5.17 | 2.29 | 3.04-4.171 |
| Puncture time | 4.215 | 1.19 | 4.19 | 4.022-4.408 |
| DAP | 24289.72 | 7858.87 | 25927.5 | 23561-26097 |
| Air Kerma | 368.18 | 114.76 | 375 | 349.66-386.7 |
Co-morbidities: A total of 52 patients (34.7%) suffered from diabetes mellitus while 62 patients (41.3%) suffered from hypertension. Among these, 20 had both the co-morbidities.
Number of attempts: It was possible to do successful puncture and proceed in the first attempt in 92 (61.33%) patients. Further, 48 patients (32%) required a second attempt; giving an overall 93.33% successful puncture rate. As a standard, a third attempt was not given, and the traditional radial artery technique was resorted to (as mentioned above). Among the rest of the 10 patients, 8 had poor jet and 2 had severe spasm (failed to cannulate DRA) and CAG was completed by radial or femoral route.
Puncture outcome: As shown in [Table/Fig-5], out of 150 patients, there was successful DRA puncture in 140 patients (93.4%). This is the most significant finding of this study.
| Complications | N=150 (%) |
|---|
| None | 140 (93.4) |
| Poor jet (Failed) | 8 (5.4) |
| Severe spasm | 2 (1.33) |
The angiography was completed with a single catheter in majority of cases. Failure of DRA puncture causing a lack of good jet were because of tortuosity of DRA, spasm of DRA due to periosteal or radial nerve irritation during puncture, pre-procedural feeble pulse, bony prominence causing defective cannulation. The average fluorotime was 3.88 minutes with a SD of 5.17.
Analytical statistics: There was no influence of age on the success of puncture. Fisher exact test was used to test the association and there was no relation between gender and success of puncture [Table/Fig-6,7]. Also, no association was found between hypertension and success of puncture; and diabetes and the success of puncture [Table/Fig-8,9].
Association of age and success of puncture.
| Age | Successful puncture (n=140) | Unsuccessful (n=10) |
|---|
| Mean age (years) | 54.82143 | 56.4 |
| Variance | 84.79522 | 147.1556 |
| P (T<=t) one-tail: 0.304573Pooled variance: 88.5874(Note: Pooled variance t-test) | t Critical one-tail 1.655215 | Not statistically significant |
Association between gender and success of puncture.
| Gender | Successful puncture | Unsuccessful puncture |
|---|
| Male | 122 | 9 |
| Female | 18 | 1 |
| Total | 140 | 10 |
| p-value=1.0, not statistically significant |
*Fisher’s-exact test
Association between hypertension and success of puncture.
| Successful puncture | Unsuccessful puncture |
|---|
| Hypertensive | 59 | 3 |
| Non-hypertensive | 81 | 7 |
| p-value=0.7405, Not statistically significant |
*Fisher’s-exact test
Association between diabetes and the success of puncture.
| Successful puncture | Unsuccessful puncture |
|---|
| Diabetic | 49 | 3 |
| Non-diabetic | 91 | 7 |
| p-value=1.0, Not statistically significant |
*Fisher’s-exact test
Discussion
The choice of vessel for performing interventional cardiology procedures has definitely moved from femoral to the radial. A further improvement is the distal radial approach, with an advantage profile as described below.
The advantages are that it aids in an early discharge of the patient. There is little restriction in wrist mobility and better patient comfort [8] and it preserves radial artery for Per-Cutaneous Coronary Intervention (PCI), Coronary Artery By-Pass Grafting (CABG) and dialysis procedures. It has the ability to prevent distal gangrene, since a branch to superficial palmar arch is given before entering snuffbox.
The potential disadvantages include the fact that severe spasm may occur, if the needle irritates the periosteum of trapezius and scaphoid bone. Potential for injury to adjacent radial nerve and resultant severe pain and spasm remain. Technical expertise is needed and DRA, owing to its smaller diameter than conventional radial artery and the access may be difficult. The potential for hematoma formation and bleeding complications is reduced, since the artery is compressed against bone [9,10].
Owing to the advantage profile, a distal radial approach has been adopted in this study and the results have been presented above. A brief comparison with the other similar studies is provided below. In the present study, the successful puncture was seen in 93.3% of the patients. This result demonstrates the feasibility of performance of distal radial approach and is the highlight of the present study. While Kieminij F, noted 62 out of 70 (88.5%) success rate, and Maitra S et al., noted an 87.5% success rate, Soydan E and Akın M, noted a 100% success rate in 54 patients [8-10].
In the present study, the average age was 55.07 years as shown in [Table/Fig-4]. This is comparable with the age in other studies conducted by Soydan E and Akın M, (59.3 years), Brunet MC et al., (53.8 years) and Roghani-Dehkordi F et al., (57 years) [10-12]. However, Oliviera MDP et al., (62 years), Kim Y et al., (63 years) and Wretowski D et al., (69 years) have described their findings in a much older population [13-15].
In the present study, males formed a much higher proportion as shown in [Table/Fig-7]. This is comparable to studies by Soydan E and Akın M, Kim Y et al., and Wretowski D et al., [10,14,15].
In the present study, no specific difference was found in the adverse outcomes with respect to gender. However, Kim Y et al., have shown that females have a smaller radial artery diameter and such a difference in the DRA size between males and females has been demonstrated in an Indian population also, by Beniwal S et al., [14,16]. Only few studies have specifically studied the gender differences and the DRA interventions appear to be generally more successful in the males.
In the present study, 41.3% had hypertension as shown in [Table/Fig-8], which is slightly lesser than other studies, Soydan E and Akın M, (61.1%) and Lee S et al., (60.5%) [10,17]. Three out of the 10 puncture failures were in hypertensives, but no statistically significant differences were noted. Other studies have noted a higher proportion of puncture failures among hypertensives. In the study by Wretowski D et al., (which describes the very Distal Radial Approach), 86% of the puncture failures occurred in hypertensive patients [15]. Beniwal S et al., have reported a statistically significant difference of the radial artery diameters between hypertensives and those without [16]. In the study by Lee S et al., seven out of the nine puncture failures (77.8%) occurred in hypertensive patients [17].
In the present study, 34.7% had diabetes as shown in [Table/Fig-9], which is comparable to the studies by Soydan E and Akın M, (33.35%) and Lee S et al., (35.5%) [10,17]. There was no statistically significant association between the main outcome (puncture success) and diabetics. In consonance with the clinical findings, Beniwal S et al., have reported (using doppler ultrasonography measurements) that no statistically significant difference was noted between the radial artery diameter between diabetics and those without [16].
Limitation(s)
One drawback of the present study was that it was not balanced for gender. Also, there was no influence of gender on success of the outcome and hence, there is a need for further verification and more studies.
Further clarification regarding other co-morbidities and their impact on clinical results, and the contribution of the differences in the radial artery diameters needs further clarification in future studies.
Conclusion(s)
Through this study, we present that distal radial approach is feasible and relatively safe. Further randomised controlled trials may be required to establish this relatively new approach.
*Fisher’s-exact test
*Fisher’s-exact test
*Fisher’s-exact test