Secondary Hyperparathyroidism in Patients with Chronic Renal Failure Attending a Tertiary Health Care Hospital- A Cross-sectional Study in Saurashtra Region of Gujarat, India
Jaiminkumar Naginbhai Parmar1, Madhu Panjwani2, Bhaveshbhai Rameshbhai Bariya3
1 Physician, Department of General Medicine, Life Care Hospital, Vadodara, Gujarat, India.
2 Physician, Department of General Medicine, Sir T Hospital, Bhavnagar, Gujarat, India.
3 Tutor, Department of Community Medicine, GMERS Medical College, Valsad, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Bhaveshbhai Rameshbhai Bariya, B1-20, Vrajleela Duplex, Waghodiya Road, Vadodara, Gujarat, India.
E-mail: bariyabhavesh7@gmail.com
Introduction
Secondary hyperparathyroidism is a known and early complication of Chronic Renal Failure (CRF) patients. Renal hyperparathyroidism leads to a host of bone and cardiovascular problems that ultimately can cause fractures, decreased quality of life, and an increased risk of death.
Aim
To determine the hospital-prevalence of secondary hyperparathyroidism in CRF patient and establish the correlation between Serum Parathyroid Hormone (PTH) level, Serum calcium and Serum phosphorus level.
Materials and Methods
It was a cross-sectional study conducted on 50 patients with CRF at Government Hospital of Bhavnagar, Gujarat. Detailed medical history and blood investigations were done as a tool for data collection. The study variables were described by using statistical parameters like proportion, mean and standard deviation. Correlation coefficient was used for analysing relationship between Serum PTH, calcium and phosphorus.
Results
Mean age of the patients was 42.57 (SD 15.19) years with almost equal representation of both genders. Hypertension was the most common aetiological morbidity (62%) among the study participants followed by diabetes (20%). The hospital prevalence of secondary hyperparathyroidism was 86% in Chronic Kidney Disease (CKD). Serum PTH negatively correlated with serum calcium and positively correlated with serum phosphorus with correlation coefficient value of -0.32 and 0.15, respectively.
Conclusion
Parathyroid abnormalities and disorders of mineral metabolism are common among patients with CKD. Parathyroid abnormalities detected early may prevent future long term extra-renal complications.
Haemodialysis, Kidney failure, Serum calcium, Serum parathyroid hormone
Introduction
The Chronic Kidney Disease is a global health burden with a high economic cost to health systems. It is an independent risk factor for Cardiovascular Disease (CVD). There is increased risk of cardiovascular morbidity, premature mortality, and/or decreased quality of life in all stages of CKD [1]. CKD leads to a progressive decline in kidney function manifested as reduction in Glomerular Filtration Rate (GFR). The term CRF is defined as the process of continuing irreversible reduction in nephron number and GFR less than 60 mL/min per 1.73 m2 [2].
The global CKD prevalence is found between 11-13% with the majority of patients in third stage. As per the systematic review and meta-analysis published in 2016, the global CKD prevalence of all five stages was 13.4%, and stages 3-5 was 10.6% [1]. The overall prevalence of CKD in India was 17.2% with stages 1, 2, 3, 4 and 5 was 7%, 4.3%, 4.3%, 0.8% and 0.8%, respectively in 2013 [3].
CRF initially manifests only as a biochemical abnormality which progresses to loss of the excretory, metabolic and endocrine function of the kidney and later on the clinical signs and symptoms of renal failure are evident [4].
Secondary hyperparathyroidism is common in patients with CRF disease progression and it is a serious concern for the health of the patient. If CRF cannot be controlled successfully, secondary hyperparathyroidism develops which can lead to soft tissue calcification, bone disease, and vascular calcification, which can impact the morbidity and mortality adversely [5]. This serious consequence of CRF arises from disregulation of the intracellular and extracellular levels of PTH, calcium, phosphorus and vitamin D (calcitriol), and it becomes more severe as kidney function deteriorates. The interaction between PTH, calcium, phosphorus and vitamin D is complex posing significant challenge in effective control of secondary hyperparathyroidism [6].
Major uremic toxin, parathormone is responsible for long-term consequences such as renal osteodystrophy, alterations in cardiovascular structure and function, severe vascular calcifications, anaemia and immune disorders. There is an increased cardiovascular morbidity and mortality among CRF patients owing to this [7].
Skeletal and cardiac difficulties may reduce by early detection of secondary hyperparathyroidism in CRF patients. The aim of this study was to estimate the hospital prevalence of secondary hyperparathyroidism among patients with CRF who were on haemodialysis or conservative management and to establish the correlation between level of Serum Parathyroid Hormone (PTH) level, Serum Phosphorus level and Serum Calcium level in CRF patients.
Materials and Methods
It was a descriptive cross-sectional study conducted at Sir Takhtasinhji Hospital, Bhavnagar during August 2012 to August 2013. The study was started after taking permission from Institutional Review Board, Human Ethics Committee (HEC), Government Medical College, Bhavnagar. (Reference letter no. IRB (HEC) no. 302/2012, Medicine Department no. 23/2012).
Inclusion and Exclusion criteria: The study included 50 patients with CRF, aged 12 years and above, admitted in the study hospital during the study period. The CRF was defined as patient having creatinine clearance of <30 mL/min/1.73 m2 for greater than six week (stage four and more) [2]. Patients with known case of parathyroid gland disease or malignancy, bone disease or bone malignancy, subjects below 12 years were excluded from the study.
Before data collection, the patients were explained about the study procedure and their informed written consent was taken. A detailed medical history including symptoms like bone pain, fatigue, breathlessness, pedal oedema, decreased urine output was obtained. History of Diabetes Mellitus, Hypertension, Connective tissue disease, Tuberculosis, Nephrotic Syndrome was obtained.
Careful general examination and systemic examination was carried out by the attending physician. All study participants were subjected to investigations like Renal Function Test, serum PTH, serum phosphorus, serum calcium level.
Secondary hyperparathyroidism was diagnosed when serum PTH level was more than 72 pg/mL and serum calcium level below 1.12 Mmol/L. Chemiluminescent (CLIA) techniques was used with instrument Beckman Coulter DxI600.
Statistical Analysis
The data was entered and analysed using Microsoft Office Excel 2010, using data analysis tools and real statistics. Percentage was used to describe the profile of study participants. Pearson correlation coefficient was calculated to show the relationship between serum PTH, serum calcium and serum phosphorus. Statistical significance was defined as p<0.05. All the data collection records were stored confidentially and data entry sheet and analysis file were password protected.
Results
In this study, 50 patients of CKD were enrolled. Among these 43 patients were found with higher level of serum parathyroid level. Thus, the prevalence of secondary hyperparathyroidism was 86%.
Majority of the patients were between 41 to 50 years age group. Mean age was 42.57 years (SD 15.19). Males constituted 48% of the population. Majority of them had breathlessness (40%) as the presenting complaint. Pedal oedema and reduced urine output were noted in 30% and 26% respectively. Hypertension was the most common aetiological morbidity (62%) [Table/Fig-1].
Profile of study participants (n=50).
| Study variable | Frequency (Percentage) |
|---|
| Age group (years) |
| Less than 21 | 3 (6%) |
| 21-30 | 11 (22%) |
| 31-40 | 9 (18%) |
| 41-50 | 14 (28%) |
| 51-60 | 10 (20%) |
| 61-70 | 3 (6%) |
| Gender |
| Male | 24 (48%) |
| Female | 26 (52%) |
| Clinical features |
| Breathlessness | 20 (40%) |
| Pedal oedema | 15 (30%) |
| Decreased urine output | 13 (26%) |
| Convulsion | 02 (4%) |
| Aetiology of CRF |
| Hypertension | 31 (62%) |
| Diabetes | 10 (20%) |
| Tuberculous condition | 5 (10%) |
| Connective tissue disease | 4 (8%) |
| Nephrotic syndrome | 10 (20%) |
| On haemodialysis | 38 (76%) |
Among the study participants (N=50), 43 had developed secondary hyperparathyroidism. S. calcium level was low in 70% of the patients suggesting hypocalcaemia, while S. phosphorus level was raised in 50% of them [Table/Fig-2].
Investigation profile of Chronic Renal Failure (CRF) patients (N=50).
| Parameter | Mean (SD) | Normal range | Frequency (%) |
|---|
| S.PTH (raised) | 278 (151)* | 14-75 mg/dL | 43 (86) |
| S.Calcium (low) | 1.08 (0.28) | 1.12-1.32 Mmol/L | 35 (70) |
| S.Phosphorus (raised) | 5.8 (1.9) | 3.5-5.5 mg/dL | 25 (50) |
| S.Urea (raised) | 120 (33.5)* | 15-40 mg/dL | 49 (98) |
| S.Creatinine (raised) | 7.8 (3.1) | 4-70 mg/dL | 50 (100) |
*Median (Quartile Deviation)
Majority of the patients with secondary hyperparathyroidism were in the age group of 41 to 50 years (27.91%). Mean age of hyperparathyroidism patients were 44.23 years [Table/Fig-3].
Profile of study participants with secondary hyper-parathyroidism (N=43).
| Study variables | N (%) |
|---|
| Age group (years) |
| Less than 21 | 1 (2.33) |
| 21-30 | 11 (25.58) |
| 31-40 | 7 (16.28) |
| 41-50 | 12 (27.91) |
| 51-60 | 9 (20.93) |
| 61-70 | 3 (6.98) |
| Gender |
| Male | 22 (51.2) |
| Female | 21 (48.8) |
| On haemodialysis | 34 (79.1) |
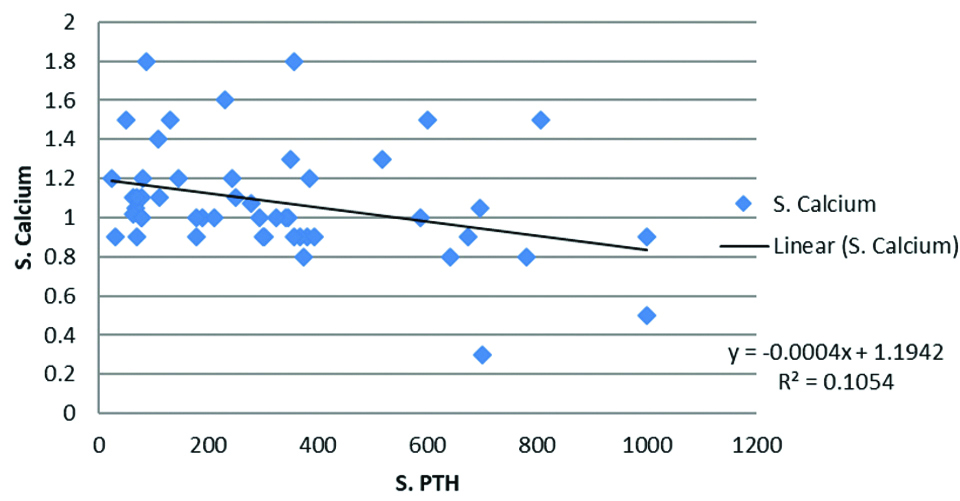
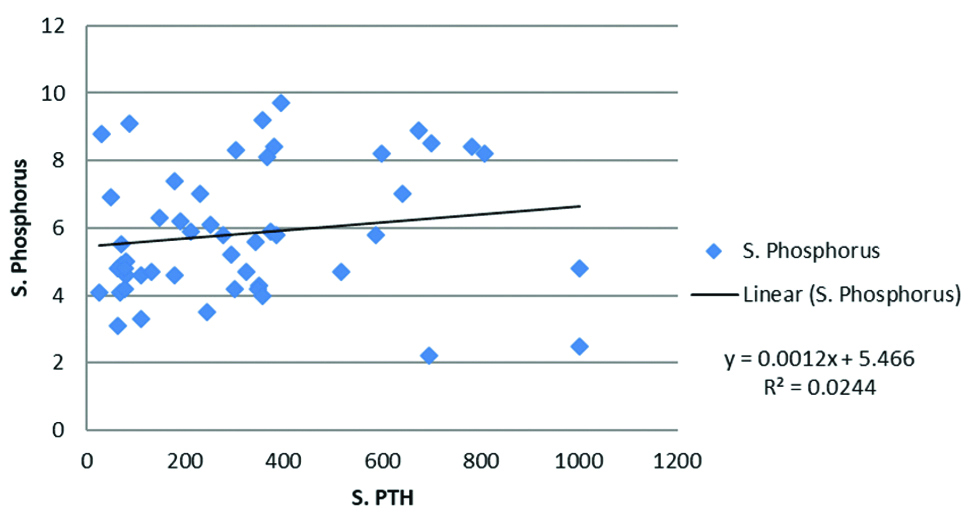
The relationship between S.PTH and S.Calcium was graphically in [Table/Fig-4]. There was linear relationship between these two variables with Pearson correlation coefficient (r) value of -0.3246 (-0.5531 to -0.05083) and p-value 0.02. This suggests moderate level negative correlation: increased level of S.PTH is associated with decrease in S. calcium level. Similarly, [Table/Fig-5] shows graphical presentation of S.PTH and S.Phosphorus relationship. S.Phosphorus positively correlated to S.PTH in the study participants with Pearson correlation coefficient value r=0.15 (0.1279 to 0.4164) and p-value of 0.279.
Relationship between S.PTH and S. Calcium level (N=50).
Relationship between S.PTH and S.Phosphorus level (N=50).
Discussion
A hospital based cross-sectional descriptive study was carried out to find out the prevalence of secondary hyperparathyroidism in CRF patients. Among the 50 patients of CKD, 43 were found with higher level of serum parathyroid level, thus the prevalence of secondary hyperparathyroidism was 86% in this study.
This was similar to study by Dayma CL et al., in Rajasthan which found 72% prevalence [8]. Patients who were on haemodialysis mostly had stage 5 CKD [9]. According to 2010 registry data from the Korean Society of Nephrology, haemodialysis was the most frequently used renal replacement therapy among the total patients with ESRD [10]. So, declining kidney function may be associated with higher level of PTH.
Disordered mineral metabolism is implicated in pathogenesis of musculoskeletal and vascular complications that afflict patients with advanced CKD. Several studies showed a compelling association between abnormalities in serum phosphate, calcium, calcium x phosphate (Ca x P) product, and PTH levels and all-cause mortality and cardiovascular events [11-13]. There was linear negative relationship between S.PTH and S.Calcium, while S.Phosphorus was found positively correlated to S.PTH in the study participants in this study. This positive correlation may be linked to increased mortality[14] emphasising the importance of SHPT control [15].
Serum calcium level was low in 70% of the patients, while S.Phosphorus level was raised in 50% of them in present study. In study by Mousavi Movahed SM et al., it was found that 28.9% of patients had low serum calcium and serum phosphorus was elevated in 31.1% of haemodialysis patients [16].
Hypertension was the most common aetiological morbidity (62%) among the study participants followed by diabetes (20%) and nephritic syndrome (20%) in present study. Hypertension was most common cause of nephropathy in the study by Dayma CL et al., (62%) followed by nephrotic syndrome (22%), diabetic nephropathy (16%), hepatitis C (12%), connective tissue disease (8%) and tuberculosis (2%) [8], while Owda A et al., found that hypertension was the cause of End Stage Renal Failure (ESRF) in 50% of the patients and diabetes in 37% of the patients [17]. Jorde R et al., had provided the evidence for an association between serum PTH levels and hypertension. In that study, involving 1784 patients over a 7-year period, the authors observed that the serum PTH level was a positive predictor of a change in systolic blood pressure over the study period in men; however it was not significant in women [18]. Serum PTH has also been shown to increase renin secretion and it may have direct effects on arteries and myocytes to promote arterial stiffness and left ventricular hypertrophy, respectively thereby responsible for development of hypertension [19,20].
Secondary hyperparathyroidism was regarded as an important issue among End Stage Renal Disease (ESRD) patients in the study by Mousavi Movahed SM et al., [16]. A 35.55% patients had iPTH levels in the accepted range, while in 37.78% it was above accepted range among fourty five haemodialysis patients in that study and its early detection and treatment may lead to slow the progression of mineral and bone metabolism disorders among CKD patients [16]. One of the conclusions from a meta-analysis study by Segall L et al., was: hyperphosphatemia, secondary hyperparathyroidism, and vitamin D deficiency had been associated with LV hypertrophy and dysfunction. Thus, attaining adequate phosphate, calcium, vitamin D, and serum PTH levels is a rational treatment goal in CKD patients, with or without heart disease, although their benefits for preventing or improving heart failure in these patients have not been proven so far [21].
Limitation(s)
This study was a single center hospital based study conducted on a limited proportion of patients and is descriptive cross-sectional. A multicentric study with large sample size is recommended that will increase the power as well as external validity of the study.
Conclusion(s)
The results of all of the above studies show that parathyroid abnormalities and disorders of mineral metabolism are common among patients with CKD. The hospital prevalence of secondary hyperparathyroidism in present study was 86%. There was also negative correlation between S.PTH and S.Ca level suggesting lower S.Ca level with higher S.PTH level. There was positive correlation between S.PTH and S.PO4 level that suggest higher value of S.PO4 is associated with higher level of S.PTH. There should be high suspicion of secondary hyperparathyroidism in patients with CKD. Early diagnosis and prompt management of the mineral metabolism disturbances may prevent suffering of the patients from further extra-renal complications.
*Median (Quartile Deviation)
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jul 11, 2020
Manual Googling: Dec 12, 2020
iThenticate Software: Jan 12, 2021 (16%)
[1]. Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, Global prevalence of chronic kidney disease- A systematic review and meta-analysisPLoS ONE 2016 11(7):e015876510.1371/journal.pone.015876527383068 [Google Scholar] [CrossRef] [PubMed]
[2]. Harrison’s principles of internal medicine, 18th ed. [monograph on the Internet] 2012 New YorkThe McGraw-Hill Companies, Inc. [Google Scholar]
[3]. Singh AK, Farag YM, Mittal BV, Subramanian KK, Reddy SR, Acharya VN, Epidemiology and risk factors of chronic kidney disease in India- Results from the SEEK (Screening and Early Evaluation of Kidney Disease) studyBMC Nephrol 2013 14:11410.1186/1471-2369-14-11423714169 [Google Scholar] [CrossRef] [PubMed]
[4]. Davidson S, Davidson’s Principles and Practice of Medicine 2006 20th edPhiladelphiaChurchil Livingstone Elsevier Publication:485 [Google Scholar]
[5]. Amiri M, Nasri H, Secondary hyperparathyroidism in chronic kidney disease patients: Current knowledgeJ Parathyroid Dis 2014 2(1):01-02.Doi: 10.12884/jpd.2014.01 [Google Scholar]
[6]. Moe SM, Disorders involving calcium, phosphorus, and magnesiumPrim Care 2008 35(2):215-37.10.1016/j.pop.2008.01.00718486714 [Google Scholar] [CrossRef] [PubMed]
[7]. Nikodimopoulou M, Liakos S, Secondary hyperparathyroidism and target organs in chronic kidney diseaseHippokratia [Internet] 2011[cited 2020 Jun 5] 15(Suppl 1):33-38.Available from: http://www.ncbi.nlm.nih.gov/pubmed/21897756 [Google Scholar]
[8]. Dayma CL, Ajmera D, Jelia SC, Jain P, Study of prevalence of secondary hyperparathyroidism in chronic renal failure in hadoti region, IndiaInt J Res Med Sci 2019 7(8):2903-08.10.18203/2320-6012.ijrms20193144 [Google Scholar] [CrossRef]
[9]. Late Stage | Kidney Disease Stages | DaVita Kidney Care [Internet]. [cited 2020 Nov 27]. Available from: https://www.davita.com/education/kidney-disease/stages/stage-5-of-chronic-kidney-disease [Google Scholar]
[10]. Jin DC, Ha IS, Kim NH, Lee SW, Lee JS, Yoon SR, Brief report: Renal replacement therapy in Korea, 2010Kidney Res Clin Pract 2012 31(1):62-71.10.1016/j.krcp.2012.01.00526889410 [Google Scholar] [CrossRef] [PubMed]
[11]. Rubel JR, Milford EL, The relationship between serum calcium and phosphate levels and cardiac valvular procedures in the hemodialysis populationAm J Kidney Dis 2003 41(2):411-21.10.1053/ajkd.2003.5005012552504 [Google Scholar] [CrossRef] [PubMed]
[12]. Malawadi BN, Suma MN, Prashant V, Akila P, Anjalidevi BS, Manjunath S, Secondary hyperparathyroidism in all the stages of chronic kidney disease in southern Indian populationInt J Pharm Pharm Sci 2014 6(4):287-90. [Google Scholar]
[13]. Michael PD, Christopher PP, David JN, Edmund L, Kidney Disease. In: Carl AB, Edward RA, David EB, editorsTietz textbook of clinical chemistry and molecular diagnostics 2006 4th editionPhiladelphiaWB Saunders:1671-1745. [Google Scholar]
[14]. Mulluche HH, Monier-Faugere MC, Hyperphosphatemia: Pharmacologic intervention yesterday, today and tomorrowClin Nephrol 2000 54:309-17. [Google Scholar]
[15]. Kim GH, Choi BS, Cha DR, Chee DH, Hwang E, Kim HW, Serum calcium and phosphorus levels in patients undergoing maintenance hemodialysis: A multicentre study in KoreaKidney Research and Clinical Practice 2014 33(1):52-57.10.1016/j.krcp.2013.12.00326877950 [Google Scholar] [CrossRef] [PubMed]
[16]. Mousavi Movahed SM, Beladi Mousavi SS, Faramarzi M, Secondary hyperparathyroidism among end-stage renal disease patients in Beharlou hospital, Tehran province, IranJ Parathyr Dis 2018 6(2):64-67.10.15171/jpd.2018.20 [Google Scholar] [CrossRef]
[17]. Owda A, Elhwairis H, Narra S, Towery H, Osama S, Secondary hyperparathyroidism in chronic hemodialysis patients: Prevalence and raceRenal Failure 2003 25(4):595-602.10.1081/JDI-12002255112911164 [Google Scholar] [CrossRef] [PubMed]
[18]. Jorde R, Svartberg J, Sundsfjord J, Serum parathyroid hormone as a predictor of increase in systolic blood pressure in malesJ Hypertens 2005 23(9):1639-44.10.1097/01.hjh.0000179764.40701.3616093907 [Google Scholar] [CrossRef] [PubMed]
[19]. Nyirenda MJ, Padfield PL, Parathyroid hormone and hypertensionJournal of Hypertension 2005 23(9):1633-34.10.1097/01.hjh.0000179508.84479.9016093904 [Google Scholar] [CrossRef] [PubMed]
[20]. Sancho JJ, Rouco J, Riera-Vidal R, Sitges-Serra A, Long-term effects of parathyroidectomy for primary hyperparathyroidism on arterial hypertensionWorld J Surg 1992 16(4):732-35.10.1007/BF020673711413842 [Google Scholar] [CrossRef] [PubMed]
[21]. Segall L, Nistor I, Covic A, Heart failure in patients with chronic kidney disease: A systematic integrative review. Lainscak M, editorBiomed Res Int [Internet] 2014 2014:937398Available from: https://doi.org/10.1155/2014/93739810.1155/2014/93739824959595 [Google Scholar] [CrossRef] [PubMed]