Introduction
This article highlights the impact on day to day life and health status after getting infected with SARS-CoV-2 and the emergence of Long COVID syndrome along with its after effects. The seriousness and degree of the long-term well-being outcomes stay dubious. Long-term outcomes seem to have dependable physical, mental, and social wellbeing impacts alongside worldwide monetary impacts. As we keep unpacking the details of COVID-19, as more research gets published, it is becoming evident that the disease is far more complicated than what we thought.
Epidemiology
The new novel Coronavirus Severe Acute Respiratory Syndrome (SARS-CoV-2) outbreak was declared a pandemic by the World Health Organisation (WHO) on March 11, 2020 [1]. As per the WHO interim guidance and the guidance provided by China, all participants are classified into:
Mild illness: Mild clinical symptoms without manifestations of pneumonia on imaging, pneumonia (having symptoms as well as having indicators of pneumonia in imaging, without having a requirement of supplemental oxygen)
Severe pneumonia: Defined as radiographic evidence of pneumonia and meeting any of the following: respiratory rate ≥30 breaths/min; oxygen saturation 93% during rest state. Severe respiratory distress is stated when there is >50% lesion progression within 24 to 48 hours, as seen in lung imaging.
The information about COVID-19, including clinical appearances, pathogenesis, and treatment, originated from exploration and perception during the intense contamination worldwide [2]. Defining the terms: Postacute COVID-19 can be defined as signs and symptoms of COVID-19 illness extending beyond three weeks from the initial onset, and chronic COVID-19 can be defined as symptoms extending beyond 12 weeks [3].
Literature Search
PubMed was searched with the terms COVID-19, Long COVID, Long term, Sequalae of articles from Jaunary 2020 till October 15, 2020. Authors scoured the abstracts for references related to long term complications, Long COVID, etc., and the article is majorly based on literature drawn from this source. A rapid google search was also conducted for the first 10 pages and a website dedicated to Long COVID was also utilised.
Long COVID Syndrome
The term “Long COVID” is used to describe the long-term effects of COVID-19 in people who have either suspected or confirmed COVID-19 [4]. Long COVID syndrome consists of dyspnoea, headache, fatigue, and anosmia and is more likely associated with increasing age, BMI, and female sex [5]. As of October 24, the total coronavirus disease cases worldwide figure was 42,725,678, and total deaths account for 1,152,253 [6]. Not much of research has been done reflecting the after-effects of COVID-19, i.e., Long COVID syndrome and impacts on respiratory, cardiovascular systems, neurological and other systems, and implications on mental health. The most common reported symptoms after acute COVID-19 found in these studies were fatigue and dyspnoea [7]. In a study performed in Germany amongst 100 patients who recently recovered from COVID-19 illness, cardiac magnetic resonance imaging showed cardiac involvement in 78% and ongoing myocardial inflammation in 60% [8]. Early reports from China proposed that 12-30% of patients admitted to the clinic with SARS-CoV-2 had a raised troponin over the 99th percentile [9]. It has been proposed that the basic pathophysiology behind these changes are increased metabolic demands, hypoxemia, right ventricular pressure overload, cytokines and T-cell mediated inflammatory reaction, or it may be as a result of direct myocardial cell infection.
Why are some people affected?
The specific reason behind why a few people experience a drawn out recuperation is obscure. It may be due to relapse or reinfection [10] inflammatory and other immune reactions [11] and also majority amounts to be a part of mental factors such as post-traumatic stress [12] which contribute to the disease process. There is long-term respiratory, musculoskeletal, and neuropsychiatric sequelae in diseases due to other coronaviruses (SARS and Middle East Respiratory Syndrome (MERS)) [13] and these have a comparable pathophysiological correlation with Long COVID.
Multisystem Involvement of SARS-COV-2
Respiratory System
According to a study published in a preprint, serial assessments spirometry (Forced Vital Capacity (FVC), Forced expiratory volume measured during the first second of the forced breath (FEV1)), lung volumes Total leucocyte count (TLC), respiratory muscle strength, lung diffusing capacity for carbon monoxide (DLCO), Six Minute Walk Test (6MWT) and High-Resolution CT (HRCT) were performed at 30 days after discharge which classified severity according to criteria: respiratory rate ≥30 times per minute, shortness of breath; SpO2 ≤93% in resting-state; partial arterial oxygen pressure (PaO2)/fraction of inspiration O2 (FiO2) ratio ≤300 mm Hg; a respiratory failure in COVID-19 requires mechanical ventilation; shock occurred or combined with other organ failure requires admitting the patient to Intensive Care Unit (ICU) and close monitoring and treatment accordingly [14].
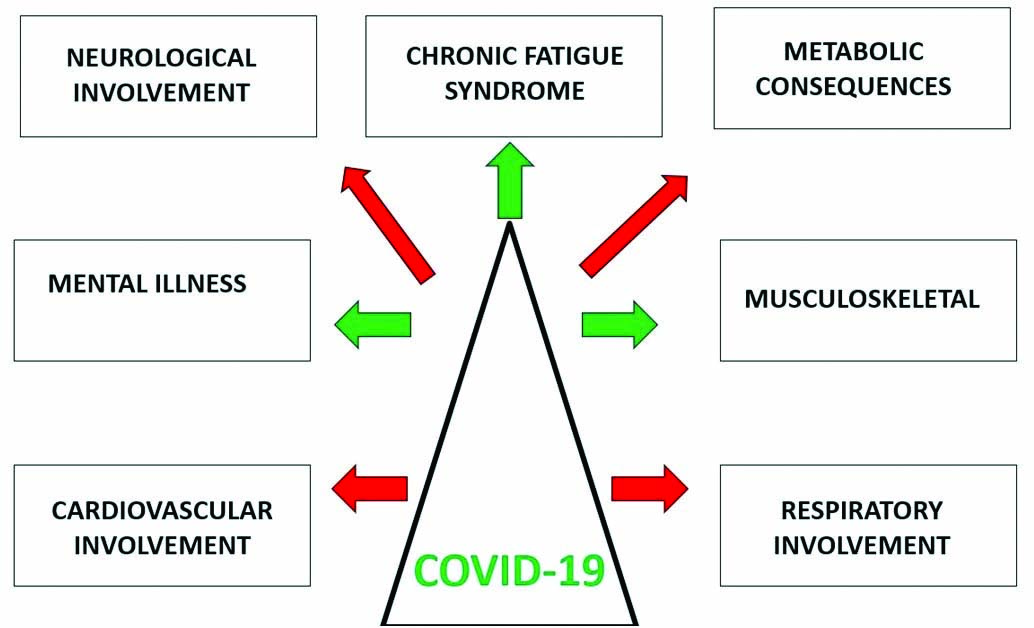
COVID-19 involves wide number of organs and organ systems as shown in [Table/Fig-1]. A 6MWT is an exercise test that evaluates the functional status closely related to patients’ daily activities with cardiopulmonary involvement.
Multisystem involvement of SARS CoV-2.
Recent research showed that nearly half of the discharged patients had a residual abnormality in the High-Resolution Chest CT scan. The most common abnormality seen amongst those patients was the decline in FEV1/FVC ratio and impaired diffusing-capacity [15]. The autopsy on patients who died from COVID-19 showed different degrees of alveolar structural destruction and pulmonary interstitial fibrosis [16]. In vast majority of patients, it was found to have diminished respiratory muscle strength in later course of illness. In early improving period of sickness, the 6MWT of the serious patients was discovered to be fundamentally more limited than that of the non severe patients, demonstrating that the extreme patients have helpless exercise resilience [17]. Follow-up serial computed tomography in this Beijing study revealed features of parenchymal abnormalities (e.g., “Ground-glass opacity”) [18]. The British Thoracic Society has published guidelines that recommend chest radiography three months postdischarge for all patients admitted to hospital with COVID-19 [19].
Cardiovascular System
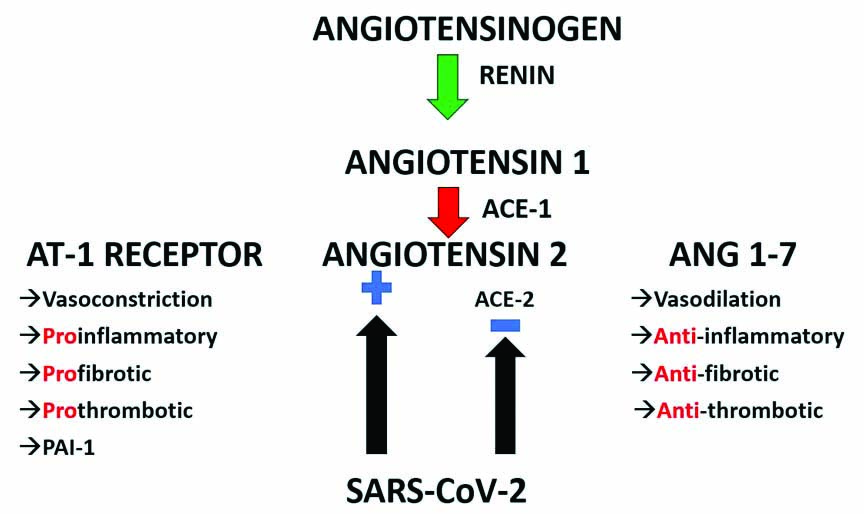
Cardiac involvement should be suspected in patients presenting with a history of new-onset palpitations, chest pain/pressure, breathlessness, or exercise-induced dizziness or syncopal attacks-even in the absence of fever and other respiratory symptoms. Angiotensin-converting enzyme 2 plays a pivotal role in pathogenesis. Myocardial injury plays a significant role. A study from the University hospital Frankfurt highlighted the Cardiac magnetic resonance study’s finding showing the involvement post COVID-19 [20]. The proposed mechanism is probably the rupture of the inflammatory plaque, cardiac stress due to high cardiac output, stent thrombosis, and infection via the angiotensin-converting enzyme 2 receptors causing systemic endothelitis [21]. The binding of SARS-CoV-2 to ACE-2 receptors could lead to acute systemic inflammatory responses and cytokine storm, consequently leading to lung-resident dendritic cell activation and T lymphocytes production and release of antiviral cytokines into the alveolar septa and interstitial compartments. A study reported that cardiac MR imaging revealed involvement in 58% of patients consisting of myocardial oedema and scar by Late Gadolinium Enhancement (LGE) [22]. Cardiac involvement was seen in majority of cases with ongoing myocardial inflammation with patients suffering from recent COVID-19 illness independent of pre-existing conditions, severity and overall course of the disease. The Peri epicardial LGE is seen in areas with increased contrast agent uptake, representing regional damage due to myocardial inflammation [23]. These findings can be attributed to fibrosis or oedema due to ongoing active pericarditis when seen with pericardial effusion. Nonischemic patterns of myocardial LGE occur in patients with acute or healed myocarditis [24]. The exact pathophysiological mechanism regarding cardiac involvement of COVID-19 is shown in [Table/Fig-2].
Pathophysiology of SARS and its action on ACE-2.
Neurological System
SARS-CoV-2 can easily enter brain tissue via direct invasion or viremia of the olfactory nerve, leading to anosmia. Some of the most common long-term neurological sequelae seen are vertigo, headache, and chemosensory dysfunction (i.e., anosmia and ageusia). Seizures, stroke, encephalitis, and other conditions such as “brain fog” and significant mood swings have been reported up to two to three months after initial illness onset [25].
Renal System
Urea nitrogen is the main element reflecting the crucial interrelation between nutritional status, protein metabolism, and renal situation [26]. Higher levels of Blood Urea Nitrogen (BUN) in COVID-19 patients suggests that there is the existence of persistent inflammation-immunosuppression and catabolism syndrome. Blood urea nitrogen is considered to be a risk factor for severe COVID-19 patients. Furthermore, urea nitrogen is an independent risk factor associated with radiographic changes seen in COVID-19. Therefore, the urea nitrogen level can be used as a parameter to predict whether patients with COVID-19 infection are at a higher risk of developing residual radiographic changes after discharge. This indicator then enables clinicians to centralise the management and recovery treatment of severe patients in a much better way [27].
Gastrointestinal Tract
The most common gastrointestinal symptoms are anorexia and diarrhea, followed by nausea and vomiting. SARS-CoV-2 virus directly invades the Gastrointestinal Tract (GIT) via binding with ACE-2 receptors in glandular cells of gastric, duodenal, and rectal epithelial cells and enterocytes of the small intestine. After getting infected with SARS-CoV-2, the “gut-lung axis”, the interaction between gut microbiota and pro-inflammatory cytokines may lead to GIT injury [28].
Metabolic System
According to a study published, it is proposed that the SARS-CoV-2 virus may lead to alterations in glucose metabolism that may lead to complicating the pathophysiology of pre-existing diabetes or may lead to new mechanisms of disease [29].
Musculoskeletal System
Recovery from COVID-19 is associated with tiredness, fatigue, and reports of myalgia, joint pains, and small joint arthritis. The most serious sequelae after restoration from the SARS epidemic in 2003 were femoral head necrosis and pulmonary fibrosis [30]. Avascular necrosis of the femoral head is probably secondary to the use of steroids. As methylprednisolone and dexamethasone are being increasingly used during the current pandemic, bone health monitoring needs to be done as one of the long-term side-effects of these medications [31].
Dermatological Manifestations
Skin rashes can take many forms, including vesicular type, macular or maculopapular, urticarial, or chilblain-like lesions on the extremities [32].
Impact on Mental Health
The current COVID-19 pandemic leads to various mental health problems, including anxiety, stress, depressive symptoms, insomnia, denial, anger, and fear globally [33]. In the current pandemic situation, financial insecurity and job loss may exacerbate these symptoms of depression, anxiety, distress, and also some of the psychosomatic symptoms, as noted by the United Kingdom- “UK-COVID-19 Social Study” [34]. Post-traumatic Stress Disease is reported and may need frequent clinical contact to avoid exacerbations and hospitalisations. In today’s environment, telemedicine, wherever possible, is recommended to monitor mental illness and provide support.
Social Health and Effect on Health Care Systems
The WHO quotes that mild illness from COVID-19 disease takes approximately two weeks to recover, while severe illness may take up to 3-6 weeks to improve ultimately [35]. PHOSP-COVID (Posthospitalisation COVID-19 study in the UK) has been brought up and funded as a long-term research study to recruit 10,000 patients who have been hospitalised with COVID-19 [36].
Effect on Emotional Health and Well-being
The impact of emotional and behavioural concerns for those affected individuals has yet to be uncovered. A diagnosis of COVID-19 and subsequent need for physical-social distancing has been found to have feelings of isolation and loneliness at some stage. Individuals recovering from COVID-19 may be at a greater risk of post-traumatic stress disorder, depression, anxiety, and substance abuse disorder. These consolidated impacts can bring about a worldwide wellbeing emergency, considering the sheer number of COVID-19 cases worldwide. “Long haulers” is the term used to describe patients coming to outpatient follow-up clinics [37]. The care of this vulnerable class of patients requires an ambidextrous approach, with an integrated research agenda to avoid fragmentation of the health care system and simultaneously to allow a comprehensive study of the long-term health consequences of COVID-19 on multiple organ systems involved and also on the overall health and wellbeing of an individual. A survey of the long-term effects of the SARS, showed that the impairment of exercise capacity and health status remains for over two years in the SARS-survivors [38].
Returning to Physical Exercise State
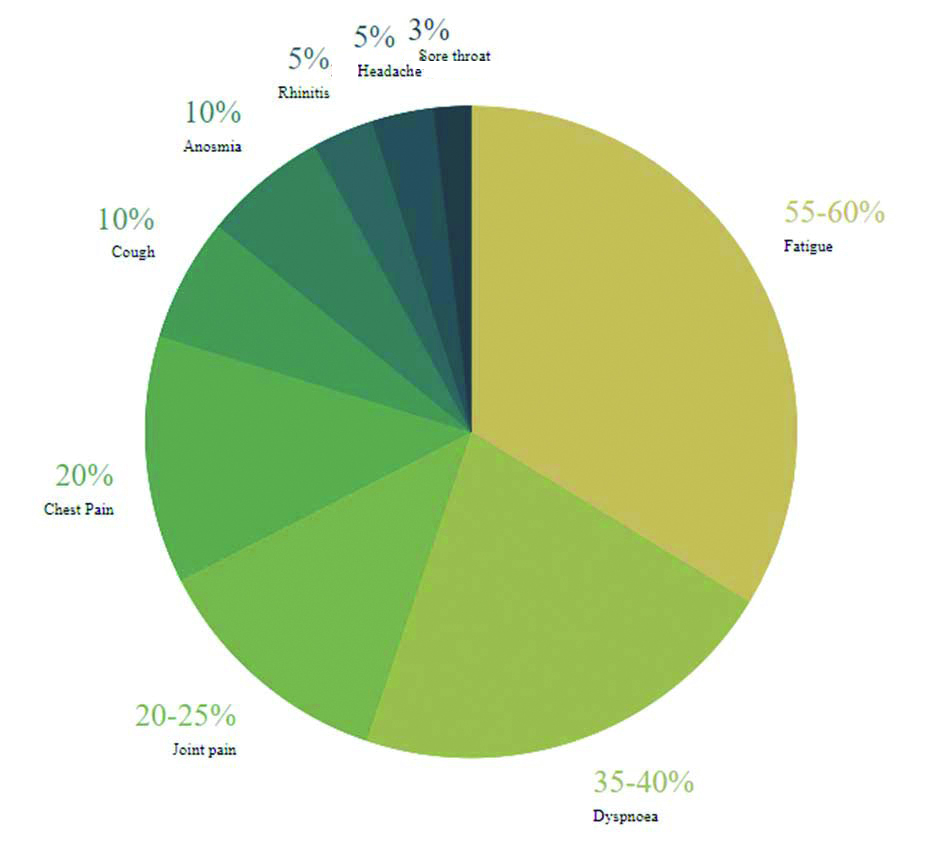
The European Association of Preventive Cardiology (EAPC) and section of sports cardiology recommends refraining from exercise until a Symptom free interval for 1 week and to resume training in a graduated way [39]. A cardiovascular investigation is recommended in an appropriate, COVID secure environment for at risk cases. As shown in [Table/Fig-3] [7], fatigue was the most commonly founded symptom in patients post COVID-19. The criteria for further studies of this population were: if the person was hospitalised during the COVID-19 illness; if symptoms of myocarditis had occurred during the acute infection; if the sickness was debilitating (confined to bed for several days) or prolonged (lasting >7 days), even if the person was apparently ‘recovered’; and a complaint of persisting exercise intolerance [39]. Sufficient evidence is not available regarding presentation of clinically mild COVID associated myocarditis nor its long-term outcome can be predicted. Regarding to some non specific symptoms in some athletes, the differential diagnosis of a past COVID-19 infection or a COVID-19 associated myocarditis should be taken into consideration [39].
The most common symptoms which are observed in patients presented post COVID-19 illness [7].
D-Dimer’s significance and its correlation with long-term symptoms: D-dimer elevation has been reported as an essential laboratory finding in COVID-19 patients. Several studies have reported that D-dimer levels on admission were an independent predictor of in-hospital death for patients with COVID-19 [40]. It is also established that the D-dimer level was a significant prognostic factor for having an abnormal DLCO. Hence, for the patients who have marked raised D-dimer, pulmonary rehabilitation should be pursued subsequently, even in the absence of severe respiratory symptoms.
Conclusion(s)
COVID-19 disease is now known to cause grievous long-term consequences. Raising awareness, recognition, research, and multidisciplinary involvement will be considered the cornerstones to manage long-term sequelae of COVID-19 effectively. Low-grade cardiac injury should be considered among COVID-19 survivors, which might limit their performance of strenuous physical exercises.
[1]. Coronavirus [Internet]. [cited 2020 Oct 25]. Available from: https://www.who.int/health-topics/coronavirus#tab=tab_1 [Google Scholar]
[2]. Why strange and debilitating coronavirus symptoms can last for months | New Scientist [Internet]. [cited 2020 Oct 21]. Available from: https://www.newscientist.com/article/mg24632881-400-why-strange-and-debilitating-coronavirus-symptoms-can-last-for-months/ [Google Scholar]
[3]. Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L, Management of post-acute covid-19 in primary careBMJ [Internet] 2020 Aug 11 [cited 2020 Oct 21] :370Available from: http://dx.doi.org/10.1136/bmj.m302610.1136/bmj.m302632784198 [Google Scholar] [CrossRef] [PubMed]
[4]. Lancet [Internet]. [cited 2020 Oct 21]. Available from: https://www.thelancet.com/infection Published online September 1, 2020 https://doi.org/10.1016/S1473-3099(20)30701-5 1 Long-term consequences of COVID-19: research needs10.1016/S1473-3099(20)30865-3 [Google Scholar] [CrossRef]
[5]. Sudre CH, Murray B, Varsavsky T, Graham MS, Penfold RS, Bowyer RC, Attributes and predictors of Long-COVID: Analysis of COVID cases and their symptoms collected by the Covid Symptoms Study AppmedRxiv [Internet] 2020 Oct 21 [cited 2020 Oct 27] 2020.10.19.20214494. Available from: https://www.medrxiv.org/content/10.1101/2020.10.19.20214494v1 [Google Scholar]
[6]. Coronavirus Update (Live): 42,725,678 Cases and 1,152,253 Deaths from COVID-19 Virus Pandemic-Worldometer [Internet]. [cited 2020 Oct 24]. Available from: https://www.worldometers.info/coronavirus/ [Google Scholar]
[7]. Carfì A, Bernabei R, Landi F, Persistent symptoms in patients after acute COVID-19 [Internet]JAMA-Journal of the American Medical Association. American Medical Association 2020 324(6):603-05.10.1001/jama.2020.1260332644129 [Google Scholar] [CrossRef] [PubMed]
[8]. Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from Coronavirus Disease 2019 (COVID-19)JAMA Cardiol [Internet] 2020 [cited 2020 Oct 20] Available from: https://jamanetwork.com/journals/jamacardiology/fullarticle/276891610.1001/jamacardio.2020.355732730619 [Google Scholar] [CrossRef] [PubMed]
[9]. Lan L, Xu D, Ye G, Xia C, Wang S, Li Y, Positive RT-PCR test results in patients recovered from COVID-19 [Internet]. Vol. 323JAMA- Journal of the American Medical Association. American Medical Association 2020 [cited 2020 Oct 23] :1502-3.Available from: http://www.nhc.gov.cn/yzygj/s7653p/202002/10.1001/jama.2020.278332105304 [Google Scholar] [CrossRef] [PubMed]
[10]. Wu F, Wang A, Liu M, Wang Q, Chen J, Xia S, Neutralizing antibody responses to SARS-CoV-2 in a COVID-19 recovered patient cohort and their ImplicationsSSRN Electron J [Internet] 2020 Apr 20 [cited 2020 Oct 23] 2020.03.30.20047365. Available from: https://www.medrxiv.org/content/10.1101/2020.03.30.20047365v210.2139/ssrn.3566211 [Google Scholar] [CrossRef]
[11]. Colafrancesco S, Alessandri C, Conti F, Priori R, COVID-19 gone bad: A new character in the spectrum of the hyperferritinemic syndrome? [Internet]. Vol. 19Autoimmunity Reviews. Elsevier BV 2020 [cited 2020 Oct 23] Pp. 102573. Available from: /pmc/articles/PMC7199723/?report=abstract10.1016/j.autrev.2020.10257332387470 [Google Scholar] [CrossRef] [PubMed]
[12]. Jiang HJ, Nan J, Lv ZY, Yang J, Psychological impacts of the COVID-19 epidemic on Chinese people: Exposure, post-traumatic stress symptom, and emotion regulationAsian Pac J Trop Med [Internet] 2020 Jun 1 [cited 2020 Oct 23] 13(6):252-59.Available from: https://www.apjtm.org/article.asp?issn=1995-7645;year=2020;volume=13;issue=6;spage=252;epage=259;aulast=Jiang10.4103/1995-7645.281614 [Google Scholar] [CrossRef]
[13]. Grn S, Schumm J, Greulich S, Wagner A, Schneider S, Bruder O, Long-term follow-up of biopsy-proven viral myocarditis: Predictors of mortality and incomplete recoveryJ Am Coll Cardiol 2012 59(18):1604-15.10.1016/j.jacc.2012.01.00722365425 [Google Scholar] [CrossRef] [PubMed]
[14]. Impact of Coronavirus Disease 2019 on Pulmonary Function in Early Convalescence Phase | Research Square [Internet]. [cited 2020 Nov 23]. Available from: https://www.researchsquare.com/article/rs-26415/v1 [Google Scholar]
[15]. Huang Y, Tan C, Wu J, Chen M, Wang Z, Luo L, Impact of coronavirus disease 2019 on pulmonary function in early convalescence phase [Internet]. Vol. 21, Respiratory ResearchBioMed Central 2020 [cited 2020 Oct 24] :163Available from: https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-020-01429-610.1186/s12931-020-01429-632600344 [Google Scholar] [CrossRef] [PubMed]
[16]. Menter T, Haslbauer JD, Nienhold R, Savic S, Hopfer H, Deigendesch N, Postmortem examination of COVID-19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings in lungs and other organs suggesting vascular dysfunctionHistopathology [Internet] 2020 Aug 1 [cited 2020 Dec 3] 77(2):198-209.Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/his.1413410.1111/his.1413432364264 [Google Scholar] [CrossRef] [PubMed]
[17]. Ong KC, Ng AWK, Lee LSU, Kaw G, Kwek SK, Leow MKS, 1-Year pulmonary function and health status in survivors of severe acute respiratory syndromeChest [Internet] 2005 [cited 2020 Oct 24] 128(3):1393-400.Available from: https://pubmed.ncbi.nlm.nih.gov/16162734/10.1378/chest.128.3.139316162734 [Google Scholar] [CrossRef] [PubMed]
[18]. Li K, Fang Y, Li W, Pan C, Qin P, Zhong Y, CT image visual quantitative evaluation and clinical classification of coronavirus disease (COVID-19)Eur Radiol 2020 30(8):4407-16.10.1007/s00330-020-06817-632215691 [Google Scholar] [CrossRef] [PubMed]
[19]. COVID-19: information for the respiratory community. British Thoracic Society. Better lung health for all [Internet]. [cited 2020 Dec 3]. Available from: https://www.brit-thoracic.org.uk/covid-19/covid-19-information-for-the-respiratory-community/ [Google Scholar]
[20]. Frankfurt study finds high rate of cardiac complications in recovered COVID-19 patients [Internet]. [cited 2020 Nov 26]. Available from: https://cardiovascularnews.com/frankfurt-study-finds-high-rate-of-cardiac-complications-in-recovered-covid-19-patients/ [Google Scholar]
[21]. Chen L, Li X, Chen M, Feng Y, Xiong C, The ACE2 expression in human heart indicates new potential mechanism of heart injury among patients infected with SARS-CoV-2Cardiovasc Res [Internet] 2020 May 1 [cited 2020 Oct 21] 116(6):1097-100.Available from: https://academic.oup.com/cardiovascres/article/116/6/1097/581313110.1093/cvr/cvaa07832227090 [Google Scholar] [CrossRef] [PubMed]
[22]. Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C, Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance ImagingJACC Cardiovasc Imaging 2020 13(11):2330-39.10.1016/j.jcmg.2020.05.00432763118 [Google Scholar] [CrossRef] [PubMed]
[23]. Puntmann VO, Carr-White G, Jabbour A, Yu CY, Gebker R, Kelle S, Native T1 and ECV of noninfarcted myocardium and outcome in patients with coronary artery diseaseJ Am Coll Cardiol 2018 71(7):766-78.10.1016/j.jacc.2017.12.02029447739 [Google Scholar] [CrossRef] [PubMed]
[24]. Gulati A, Jabbour A, Ismail TF, Guha K, Khwaja J, Raza S, Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathyJAMA-J Am Med Assoc [Internet] 2013 Mar 6 [cited 2020 Oct 21] 309(9):896-908.Available from: https://jamanetwork.com/10.1001/jama.2013.136323462786 [Google Scholar] [CrossRef] [PubMed]
[25]. Zubair AS, McAlpine LS, Gardin T, Farhadian S, Kuruvilla DE, Spudich S, Neuropathogenesis and Neurologic manifestations of the coronaviruses in the age of coronavirus disease 2019: A review [Internet]JAMA Neurology. American Medical Association 2020 (77):1018-27.[cited 2020 Oct 24]. p. Available from: https://jamanetwork.com/10.1001/jamaneurol.2020.206532469387 [Google Scholar] [CrossRef] [PubMed]
[26]. Cheng A, Hu L, Wang Y, Huang L, Zhao L, Zhang C, Diagnostic performance of initial blood urea nitrogen combined with D-dimer levels for predicting in-hospital mortality in COVID-19 patientsInt J Antimicrob Agents [Internet] 2020 Sep 1 [cited 2020 Oct 25] 56(3):106-10.Available from: /pmc/articles/PMC7377803/?report=abstract10.1016/j.ijantimicag.2020.10611032712332 [Google Scholar] [CrossRef] [PubMed]
[27]. Cheng Y, Luo R, Wang K, Zhang M, Wang Z, Dong L, Kidney disease is associated with in-hospital death of patients with COVID-19 [Internet]. Vol. 97Kidney International. Elsevier B.V. 2020 [cited 2020 Nov 23] :829-38.Available from: /pmc/articles/PMC7110296/?report=abstract10.1016/j.kint.2020.03.00532247631 [Google Scholar] [CrossRef] [PubMed]
[28]. Zhang D, Li S, Wang N, Tan HY, Zhang Z, Feng Y, The cross-talk between gut microbiota and lungs in common lung diseases [Internet]. 11Frontiers in Microbiology 2020 [cited 2020 Oct 25] Frontiers Media S.A.Available from: /pmc/articles/PMC7052046/?report=abstract10.3389/fmicb.2020.0030132158441 [Google Scholar] [CrossRef] [PubMed]
[29]. Rubino F, Amiel SA, Zimmet P, Alberti G, Bornstein S, Eckel RH, New-Onset Diabetes in Covid-19 [Internet]. Vol. 383New England Journal of Medicine. Massachussetts Medical Society 2020 [cited 2020 Oct 25] :789-91.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7304415/10.1056/NEJMc201868832530585 [Google Scholar] [CrossRef] [PubMed]
[30]. Zhang P, Li J, Liu H, Han N, Ju J, Kou Y, Long-term bone and lung consequences associated with hospital-acquired severe acute respiratory syndrome: A 15-year follow-up from a prospective cohort studyBone Res [Internet] 2020 Dec 1 [cited 2020 Oct 25] 8(1):1-8.Available from: https://doi.org/10.1038/s41413-020-0084-510.1038/s41413-020-0084-532128276 [Google Scholar] [CrossRef] [PubMed]
[31]. Dexamethasone in hospitalised patients with COVID-19-Preliminary ReportN Engl J Med [Internet] 2020 Jul 17 [cited 2020 Oct 25] Available from: https://pubmed.ncbi.nlm.nih.gov/32678530/ [Google Scholar]
[32]. Galván Casas C, Català A, Carretero Hernández G, Rodríguez-Jiménez P, Fernández-Nieto D, Rodríguez-Villa Lario A, Classification of the cutaneous manifestations of COVID-19: A rapid prospective nationwide consensus study in Spain with 375 casesBr J Dermatol [Internet] 2020 Jul 1 [cited 2020 Oct 24] 183(1):71-77.Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/bjd.1916310.1111/bjd.1916332348545 [Google Scholar] [CrossRef] [PubMed]
[33]. Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A, The outbreak of COVID-19 coronavirus and its impact on global mental health [Internet]. Vol. 66International Journal of Social Psychiatry 2020 [cited 2020 Oct 25] SAGE Publications Ltd:317-20.Available from: http://journals.sagepub.com/doi/10.1177/002076402091521210.1177/002076402091521232233719 [Google Scholar] [CrossRef] [PubMed]
[34]. HOME | CovidSocialStudy [Internet]. [cited 2020 Oct 25]. Available from: https://www.covidsocialstudy.org/ [Google Scholar]
[35]. Situation Report-73 HIGHLIGHTS. [cited 2020 Dec 4]; Available from: https://www.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200402-sitrep-73-covid-19.pdf [Google Scholar]
[36]. Major study into long-term health effects of COVID-19 launched in the UK [Internet]. [cited 2020 Oct 25]. Available from: https://www.nihr.ac.uk/news/major-study-into-long-term-health-effects-of-covid-19-launched-in-the-uk/25200 [Google Scholar]
[37]. Patient Led Research for COVID-19 Long Haulers [Internet]. [cited 2020 Oct 21]. Available from: https://patientresearchcovid19.com/ [Google Scholar]
[38]. Ngai JC, Ko FW, Ng SS, To KW, Tong M, Hui DS, The long-term impact of severe acute respiratory syndrome on pulmonary function, exercise capacity and health statusRespirology [Internet] 2010 Apr [cited 2020 Oct 25] 15(3):543-50.Available from: /pmc/articles/PMC7192220/?report=abstract10.1111/j.1440-1843.2010.01720.x20337995 [Google Scholar] [CrossRef] [PubMed]
[39]. Schellhorn P, Klingel K, Burgstahler C, Return to sports after COVID-19 infectionEur Heart J [Internet] 2020 May 20 [cited 2020 Oct 25] Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7314071/ [Google Scholar]
[40]. Juvela S, Siironen J, D-Dimer as an independent predictor for poor outcome after aneurysmal subarachnoid hemorrhageStroke 2006 37:1451-1456.Available from: http://ahajournals.org10.1161/01.STR.0000221710.55467.3316690901 [Google Scholar] [CrossRef] [PubMed]