In the current medical scenario, hypothyroidism is becoming one of the prevalent co-morbid conditions with a prevalence rate of 11% in Indian population [1]. Hypothyroidism has been attributed to affect various organ systems especially cardiovascular system. Heart disease accounts for a large proportion of mortality in developed and developing countries. The effects of thyroid disturbances on cardiovascular system have been well established for more than two centuries. The effects of hypothyroidism on cardiovascular system have been studied and there are various speculations. One conjecture is the disturbances in lipid profile which is thought to be due to effects of modified adipokines on low-density lipoprotein receptor affinity and inadequate thyroid hormone-mediated signaling leading to lower levels of cholesterol ester transfer protein which leads to low density lipoprotein accumulation [2]. The second speculation is the reduction of nitric oxide and endothelial dysfunction which leads to increase in systemic vascular resistance and altered myocyte function ultimately terminating in a cardiac dysfunction or death. With the increase in the prevalence of CVD, novel tools to predict cardiovascular risk in different population is gaining importance. LAP is one of the novel tools that were formulated to prognosticate the cardiovascular risk in hypothyroidism.
LAP is principally an abdominal adiposity biomarker that correlates with central lipid accumulation. It is a significant index of central adiposity to predict the occurrence of metabolic syndrome. LAP is based on a combination of two safe, easy and cost-effective measurements: waist circumference and serum triglycerides. The index was first presented by Kahn HS in his study which concluded that it was a better index than body mass index in predicting cardiovascular risk [3]. Kahn’s findings support the opinion that over accumulation of lipid brings worse cardiovascular consequences of weight gain as indicated by body mass index. This index was developed in an effort to reproduce the anatomical and physiological changes occurring with lipid accumulation in terms of numerical data [4].
Many studies depicted LAP score as a predictor of cardiovascular complications in various existing diseases such as type 2 diabetes mellitus, metabolic syndrome and polycystic ovarian syndrome [5,6]. However, there are no studies in Indian population to reveal the role of LAP score in hypothyroid patients. Therefore, it was aimed to study LAP score in hypothyroid patients and correlate it with TSH levels in hypothyroid patients. This study may form a basis to use LAP score to predict cardiovascular risk in hypothyroidism.
Materials and Methods
The study was a cross-sectional descriptive study conducted in a Tertiary care hospital in Southern India. Ethics committee approval was obtained from Institutional Human Ethics Committee with number 16/328 and the study was conducted for a period of one year from January to December 2017. The study was carried out according to the Helsinki Declaration of 1975 as revised in 1996. Considering the study by Jung CH et al., as reference, the sample size was calculated [7]. The Odds ratio for person with hypothyroidism having elevated LAP in comparison to general population was found to be 3.6. This was taken into consideration keeping the alpha error at 5% and power of study at 80% a sample size of 53 in each group was obtained using OpenEpi software. Assuming a no-response rate of 10% the sample size was decided to be 59 in each group.
The study included two groups- Cases and Controls. The cases were 59 hypothyroid patients who attended the endocrinology outpatient department during the study period and the controls were 59 individuals with no current or previous diagnosis of thyroid dysfunction attending the master health check-up services in the hospital. Patients with existing cardiovascular disease, diabetes mellitus, metabolic syndrome and who are on lipid-lowering drugs were excluded from the study.
After obtaining a written informed consent from the study participants, details such as age, gender, serum TSH, serum triglyceride levels were collected from medical records. Serum triglyceride measurements were converted from mg/dL to mmol/L. Waist circumference of the study population was measured at the midpoint between the lower border of the rib cage and the iliac crest in a plane perpendicular to the long axis of the body, with the subject standing balanced on both feet, approximately 20 cm apart, with both arms hanging freely by using a flexible inch tape.
LAP was calculated as follows:
LAP for men={Waist circumference (cm)-65}×{Triglyceride concentration (mmol/L)}.
LAP for women={Waist circumference (cm)-58}×{Triglyceride concentration (mmol/L)}.
The data collected was anonymised by removing identifiers such as barcode numbers and identification details as per the ethical norms.
Statistical Analysis
The data was organised in Microsoft Excel and then exported to the SPSS software version 24.0 for Windows, for analysis. Numerical data was expressed as Mean±SD. The categorical variables were correlated using the Chi-square test, and quantitative variables were compared using the t-test for independent variables. Correlation was tested using the Pearson correlation analysis. The p-value ≤0.05 was considered statistically significant.
Results
The total number of participants were 118 out of which 59 (50%) were hypothyroid cases and 59 (50%) were controls. The age, gender, waist circumference and serum triglyceride of both the groups are depicted in [Table/Fig-1]. The two groups showed no statistically significant difference with regard to age (p-value 0.28) and gender (Chi-square test significance value 0.19) and therefore matched. There was no statistically significant difference between the waist circumference (p-value 0.29) and triglyceride concentration (p-value 0.39) between the two groups. The mean LAP score among cases were 38.6±15.6 cm.mmol/L and among controls were 30.9±13.2 cm.mmol/L. There was a statistically significant difference in the LAP scores with a p-value of 0.004 (p<0.05 considered significant).
Demographic profile of study population.
| Characteristics | Cases | Controls |
|---|
| Age (years) | 59.9±15.2 | 46.8±12.0 |
| Number of males | 21 | 29 |
| Number of females | 38 | 30 |
| Waist circumference (cm) | 83.37±4.45 | 84.37±3.91 |
| Serum triglyceride (mmol/L) | 1.5±0.09 | 1.6±0.08 |
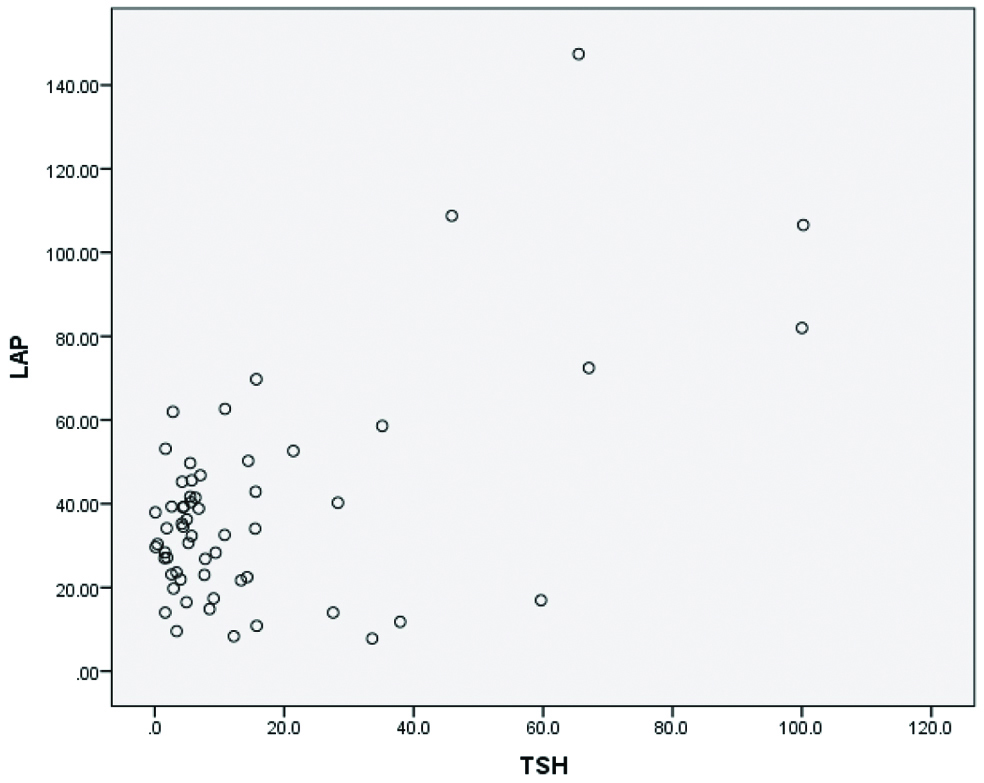
The LAP scores had no association with age (p-value 0.48) of hypothyroid patients. Chi-square test showed that LAP scores did not differ among male and female hypothyroid patients (p-value 0.38). Among the cases, LAP scores positively correlated with TSH levels to establish an association by means of Pearson’s correlation analysis (r-value 0.784 and p-value <0.001). Scatter plot showing the distribution of LAP and TSH values is depicted in [Table/Fig-2].
Scatter plot showing correlation between LAP and TSH.
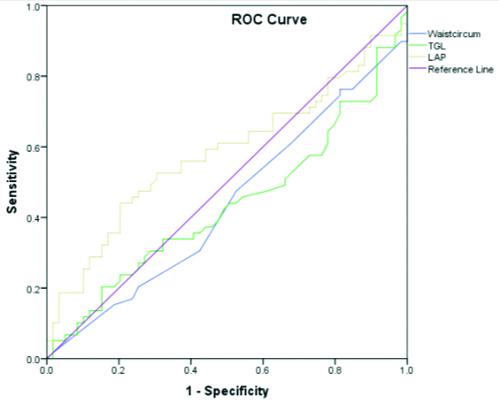
Receiver Operating Characteristic (ROC) curve analysis was done to assess the effectiveness of LAP in comparison to waist circumference and triglyceride levels [Table/Fig-3]. The areas under the curves were 0.43, 0.47 and 0.58 for waist circumference, triglycerides and LAP, respectively.
ROC curve depicting waist circumference, LAP score and triglyceride in hypothyroid patients.
Waistcircum: Waist circumference; TGL: Triglyceride
Discussion
A predictor of cardiovascular risk in hypothyroid patients is pivotal. Cardiovascular complications can be as trivial as a mild tricuspid regurgitation or as severe as a massive myocardial infarction or sudden cardiac death. Cardiovascular diseases occurring unnoticed in a hypothyroid patient can be devastating for the patient and their families, questioning the ability of the physician for neglecting the cardiovascular risk concealed behind the low thyroid hormone levels. Owing to the growing incidence of risk of CVD, early detection of risk factors has become the basis of the morbidity and mortality reduction strategies. While many guidelines suggest a combination of screening metrics to target individuals at greater risk of cardiovascular events, the pre-established methods are not specifically helpful in prevention of the same [8]. Several cardiovascular risk evaluation instruments or tools are available for utilisation amongst healthy people such as CUORE [9], SCORE [10], Framingham [11], etc. Even then, such tools are not always effective in cases where expensive biochemical and anthropometric values need to be identified and the time designed to assess the individual is restricted. LAP score will be appreciated for its use in primary healthcare facilities that face financial limitations to calculate more sophisticated cardiovascular risk markers. Studies that applied LAP to assess cardiovascular risk in disease populations such as polycystic ovarian syndrome, metabolic syndrome and type 2 diabetes mellitus have been successful [5,12]. Xie X et al., assessed the risk of CVD among the growth hormone deficiency patients in China by LAP index and Framingham score [13]. In addition, it was noticed that the LAP is strongly associated with insulin resistance [14,15], dysregulation of blood glucose [16], and type 2 diabetes mellitus [17,18] and is also related with incidence of stroke [19]. A study from China states that TSH levels were positively associated with visceral adiposity index and LAP score [20]. However, there are no available studies on LAP scores of hypothyroid patients among Indian population.
In this study, LAP scores were significantly different between the study groups suggesting the metabolic implications of hypothyroidism.
There was no statistically significant difference between case and control groups with regards to age and gender. Contradictorily, Wakabayashi I et al., tested 10,170 Japanese workers aged 35-40 years and placed the cut-off values for LAP score among men and women as 37.2 cm.mmol/L and 21.1 cm.mmol/L, respectively [5]. It is well-established that the incidence of CVD increases with increasing age.
Population studies such as National Health and Nutrition Examination Survey (NHANES) III and NHANES 1999-2002 revealed higher TSH values with increasing age [21]. Hence, TSH rise may be linked with increased cardiovascular risk. The results of this study show good correlation of LAP score with TSH levels. Most of the commercially available TSH assays are based on immunometric assays which have more interference due to heterophile antibodies and it is an expensive test. A simple score such as LAP is preferable in developing countries to assess cardiovascular risk because standardised waist measurements are highly reproducible [1] and they are arguably simpler and less expensive to obtain than well-standardised weights and heights. Also, the laboratory cost of a single serum triglyceride assay would be low as compared with the costs of multiple tests for lipoproteins and an extensive biochemical profile. One of the advantages of LAP is that it does not arbitrarily dichotomise. Disadvantages such as venipuncture and the fasting state for testing serum triglycerides is a major inconvenience.
Limitation(s)
This research poses some significant limitations due to the study design. The present study was a cross-sectional study in which lifestyle associated data such as smoking, alcohol consumption, exercise, and eating patterns has not been recognised that could presumably have an effect on the correlation of the LAP index. Further, the size of the sample was limited. Because some patients in present study underwent a single consultation, cardiovascular events was not reported that occurred in due course. Finally, the majority of the patients were from a tertiary care centre in Southern India, so present study results cannot be readily extrapolated to other populations.
Conclusion(s)
This study reveals evidence for significant positive correlation of LAP score with TSH levels. Further LAP score is better than waist circumference or serum triglycerides, though not statistically insignificant, in hypothyroid patients. However, larger prospective studies need to be carried out to establish its association.
Further research is required on a larger scale in order to assess and determine an appropriate cut-off value for LAP scores. A follow-up study is also needed to observe the occurrence of any cardiovascular event in the study population. This will enhance the predictive potential of LAP score in prognosticating cardiovascular risk in hypothyroid population.