Introduction
Coronavirus Disease (COVID-19) outbreak is one of the biggest medical challenges to humankind in recent times, started from China in December 2019, and had spread to almost all the countries of the world. The social, psychological and economic fissures exposed by the pandemic resulted in mass disruption in human behaviour population. This is pushing them towards more stress.
Aim
To analyse the anxiety and depressive symptoms in COVID-19 positive patients.
Materials and Methods
A cross-sectional study was conducted on 325 COVID positive patients who were admitted in isolation ward in Tertiary Care Centre and were enrolled in this study, out of which 18 subjects refused to give the consent and 5 were already taking psychiatric medications and were excluded. Telephonic contact was not established with rest of the 5 patients. After ethical clearance, the anxiety and depressive symptoms were assessed by using Hamilton Anxiety Rating Scale (HAM-A) and Hamilton Depression Rating Scale (HAM-D).
Results
Maximum patients belonged to age group of 21-40 years (54.9%). Maximum patients were males (70%). Almost 3/4th of the population 64% had depressive symptoms of different severity and 61% had anxiety symptoms. Significant association of anxiety symptoms was seen with gender (p=0.001) and marital status (p=0.002). No association with depressive symptoms was seen with gender (p=0.087) and marital status (p=0.399).
Conclusion
COVID-19 had significant impact on the patients. More than half of the population had showed the psychological issues in the form of anxiety and depression. Males and married patients were affected more with both anxiety and depressive symptoms.
Anxiety, Coronavirus disease, Depression, Lockdown
Introduction
COVID-19 was declared as a Public Health Emergency of International Concern by World Health Organisation (WHO) in January, 2020. It was declared as a pandemic, with 7 lacs confirmed cases and more than 33,000 deaths in 204 countries, areas, or territories [1]. Globally, 9,843,073 confirmed cases of COVID-19, including 495,760 deaths, reported to WHO till June, 2020 end [1].
In India, COVID-19 cases showed its surge in the 2nd week of March 2020. Gradually, 1356 cases were reported with 46 deaths [2]. Almost all the cases had either a positive travel history or being in close contact with a confirmed COVID-19 patient. In view of this, lockdown was declared by the Prime Minister of India [3]. World-wide, countries have also taken similar or even strict measures to stop community spread of COVID-19. In India, from January 30 to 28 June 2020, there were 5,28,859 confirmed cases of COVID-19 with 16,095 deaths [4].
Historically, lockdown had been seen in 2003 (SARS), 2009 (SWINE FLU) and 2011(9/11) attack, and during riots in several countries and had many issues i.e., significant mental health problems ranging from anxiety, fear, depressive symptoms, sense of loneliness, sleep disturbances, anger issues, etc., and later symptoms of post-traumatic stress disorder and depression after 3-4 weeks of discharge [5]. Swine Flu was associated with stress, and general anxiety on a trend level, but not with depression. Although the Flu was significantly correlated with health anxiety, contamination cognitions and disgust sensitivity [3].
In addition to the physical impacts, mental health is also affected. Various numbers of psychiatric outcomes including social and occupational were found during this pandemic, at every level, from state to international. There was fear of acquiring the disease or death, people became helpless as no treatment was found.
The pandemic has had a harmful effect on the public mental health which can even lead to psychological crisis which might result in mass unemployment, starvation, increase in gender-based violence, homelessness, alcoholism, loan defaults and millions slipping into poverty. India in the current scenario with constantly decreasing growth rates presently projected at 1.9% by the International Monetary Fund (IMF). This is pushing them towards more stress. Farmer suicides occurring due to poverty, alcoholism, depression and family disputes, etc., was further intensified by COVID-19. The COVID-19 crisis brought a unique dilemma to the student fraternity too [4-6].
Getting infected and staying isolated (quarantined) as well as a fear of having serious complications due to COVID can have different psychological impact in different age groups as well. As the schools remained closed, children may feel restless as they may run out of the options to keep themselves engaged and unable to interact with the peer groups leading to irritability and boredom. Elderly may feel that their movement has been restricted due to which they were not able to carry out with their daily routine activities. Adults may feel burdened with household chores in the absence of housemaids/servants along with the difficulty in managing the monetary issues of the family. All this had some degree of psychological impact on the public. Therefore, this study was planned as a sense of panic has even set up among the general population because of the increasing number of positive cases.
The study aimed to assess anxiety symptoms and depressive symptoms in patients suffering from COVID-19.
Materials and Methods
The present study was a cross-sectional study in which the data was collected as socio-demographic and clinical variables related to COVID-19. About 325 positive patients who were admitted in isolation ward in Tertiary Care Centre were enrolled in this study, out of which 18 subjects refused to give the consent and 5 were already taking psychiatric medications and were excluded. Telephonic contact was not established with rest of the 5 patients, having a total of 297 patients. It took 15-20 minutes to interview the patient. After getting the ethical approval from Institutional ethical committee, number as 1759 from the committee, the study was conducted. First the doctor on duty was approached to get the information of the patient. The information was collected telephonically after taking the verbal consent in the month of May to July, 2020.
Inclusion criteria: Subjects diagnosed with COVID positive, above 15 years of age and who gave the informed consent was enrolled.
Exclusion criteria: The patients having any other co-morbid psychiatric or a medical condition was excluded from the study.
HAM-A [7] and HAM-D [8] were the tools used to assess the anxiety and depressive symptoms in the patients respectively.
Tools
Socio-demographic profile: Self-made performa was used in which, age, sex, marital status, education, residential area and religion was included.
HAM-A [7]: The HAM-A was one of the first rating scales developed to measure the severity of anxiety symptoms. It consists of 14 items and each item is scored on a scale of 0 (not present) to 4 (severe), with a total score range of 0-56, where <17 indicated mild severity, 18-24 indicates mild to moderate and 25-30 indicated moderate severity. Maier W et al., tested the scale’s reliability and validity in two samples of 97 anxious and 101 depressed individuals and concluded that the reliability and concurrent validity of the HAM-A and its sub-scales were sufficient: there is reasonable inter-rater reliability and good one-week retest reliability (Y alpha=0.77 to 0.92.) [9].
HAM-D [8]: This is the most widely used clinician-administered depression assessment scale. Likert scoring is used and there are total of 17 items. Interpretation is; 0-7=Normal; 8-13=Mild Depression; 14-18=Moderate Depression; 19-22=Severe Depression and >23=Very Severe Depression. The internal consistency reliability of all forms of the HDI was high and ranged from coefficient alpha (ra)=0.91 to 0.94. Hamilton Depression Inventory (HDI) forms demonstrated high levels of reliability (ra=0.91 to 0.94, test-retest reliability (rtt)=0.95 to 0.96). Extensive validity evidence was presented, including content, criterion related, construct, and clinical efficacy of the HDI cut-off score [10].
Statistical Analysis
Descriptive analysis, using mean for variables such as clinical parameters and socio-demographic profile was assessed. Non-parametric tests Chi-square test was used for comparing variables distinct in nature. A p-value <0.05 considered statistically significant.
Results
[Table/Fig-1] shows the socio-demographic profile of the patients which were included in the study. Among the total 297 patients, maximum patients were in the age group of 21-40 years (54.9%). Maximum patients were males (70%), and 30% were females. Among all, about 34% were educated till 10th and 3.7% were illiterate. About 250 (84.2%) were Hindu and 47 (15.8%) were others. Maximum (65.7%) patients belonged to the urban area and 34.3% were resident of rural area. Distribution of anxiety severity is shown in [Table/Fig-2].
Socio-demographic profile of the patients.
| Socio-demographic profile | Variables | Frequency (%) |
|---|
| Age group (years) | 15 to 20 | 36 (12.1) |
| 21 to 40 | 163 (54.9) |
| 41 to 60 | 76 (25.5) |
| More than 60 | 22 (7.4) |
| Sex | Male | 208 (70) |
| Female | 89 (30) |
| Marital status | Unmarried | 73 (24.6) |
| Married | 224 (75.4) |
| Education | Illiterate | 11 (3.7) |
| Upto 5th | 62 (20.9) |
| Upto 10th | 101 (34.0) |
| High school | 85 (28.6) |
| Graduation | 33 (11.1) |
| Postgraduation | 5 (1.7) |
| Religion | Hindu | 250 (84.2) |
| Others | 47 (15.8) |
| Locality | Rural | 102 (34.3) |
| Urban | 195 (65.7) |
Distribution of anxiety severity in the patients.
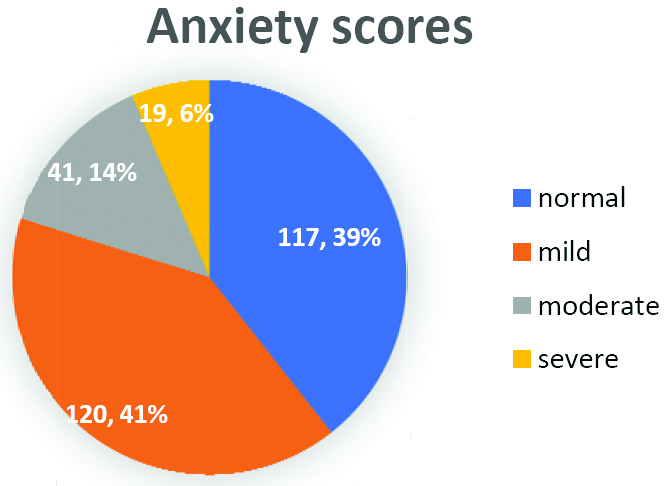
A significant association was seen with gender (p=0.001) and marital status (p=0.002). This depicts that males were more affected as compared to the females [Table/Fig-3].
Association of scores on HAM-A with the socio-demographic profile of the subjects.
| Socio-demograpic profile | Variables | Normal | Mild anxiety | Moderate anxiety | Severe anxiety | Total n (%) | p-value |
|---|
| Sex | Male | 76 (36.5%) | 77 (37%) | 37 (17.8%) | 18 (8.7%) | 208 (70) | 0.001* |
| Female | 41 (46.1%) | 43 (48.3%) | 4 (4.5%) | 1 (1.1%) | 89 (30) |
| Age (years) | ≤40 | 70 (35.0%) | 87 (43.5%) | 29 (14.5%) | 14 (7.0%) | 200 (67) | 0.171 |
| >40 | 47 (48.5%) | 33 (34.0%) | 12 (12.4%) | 5 (5.2%) | 97 (33) |
| Marital Status | Married | 91 (40.6%) | 80 (35.7%) | 34 (15.7%) | 19 (8.8%) | 224 (75.4) | 0.002* |
| Unmarried | 26 (35.5%) | 40 (54.8%) | 7 (9.6%) | 0 (0%) | 73 (24.6) |
| Education | Till 10th | 65 (37.4%) | 71 (40.8%) | 26 (14.9%) | 12 (6.9%) | 174 (58.6) | 0.797 |
| 10th or higher | 52 (42.3%) | 49 (39.8%) | 15 (12.2%) | 7 (5.7%) | 123 (39.7) |
| Religion | Hindu | 103 (41.0%) | 101 (40.2%) | 34 (13.5%) | 13 (5.2%) | 251 (84.2) | 0.196 |
| Others (Muslim, Sikh) | 14 (29.7%) | 19 (40.4%) | 7 (14.8%) | 6 (12.7%) | 46 (15.8) |
| Locality | Rural | 36 (35.6%) | 42 (41.6%) | 16 (15.8%) | 7 (6.9%) | 101 (34.3) | 0.771 |
| Urban | 81 (41.3%) | 78 (39.8%) | 25 (12.8%) | 12 (6.1%) | 196 (65.7) |
chi-square test was used; *significant
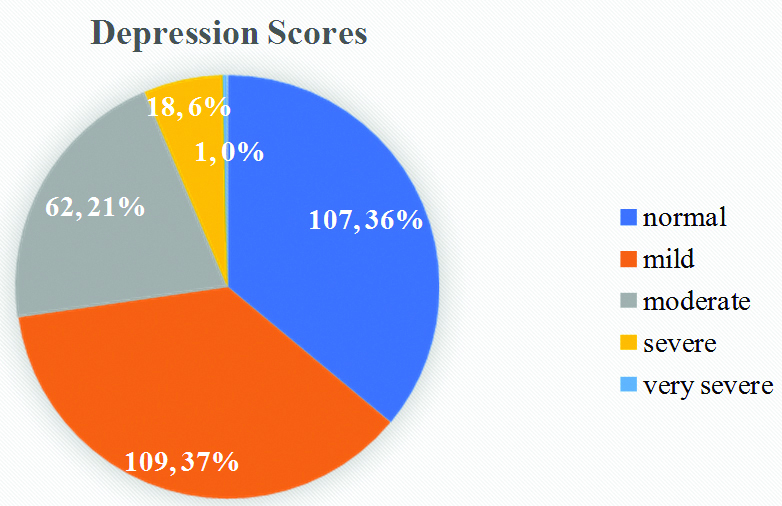
The depression scores of the patients is shown in [Table/Fig-4]. No significant association was seen with any of the socio-demographic profile variable [Table/Fig-5].
Showing the distribution of depression scores.
Association of scores on HAM-D with the socio-demographic profile of the subjects.
| Socio-demographic profile | Variables | Normal | Mild depression | Moderate depression | Severe depression | Very severe depression | Total n (%) | p-value |
|---|
| Age (years) | ≤40 | 71 (35.50%) | 72 (36.00%) | 44 (22.00%) | 13 (6.50%) | 0 (0.00%) | 200 (67) | 0.599 |
| >40 | 36 (37.10%) | 37 (38.10%) | 18 (18.60%) | 5 (5.20%) | 1 (1.00%) | 97 (33) |
| Sex | Female | 39 (43.80%) | 29 (32.60%) | 13 (14.60%) | 7 (7.90%) | 1 (1.10%) | 89 (30) | 0.087 |
| Male | 68 (32.70%) | 80 (38.50%) | 49 (23.60%) | 11 (5.30%) | 0 (0.00%) | 208 (70) |
| Marital status | Married | 75 (33.48%) | 88 (39.2%) | 48 (21.4%) | 12 (5.3%) | 1 (0.50%) | 224 (75.4) | 0.399 |
| Unmarried | 32 (43.80%) | 21 (28.80%) | 14 (19.20%) | 6 (8.20%) | 0 (0.00%) | 73 (24.6) |
| Educational status | Till 10th | 59 (33.90%) | 62 (35.60%) | 42 (24.10%) | 10 (5.70%) | 1 (0.60%) | 174 (58.6) | 0.467 |
| 10th or higher | 48 (39.00%) | 47 (38.20%) | 20 (16.30%) | 8 (6.50%) | 0 (0.00%) | 123 (39.7) |
| Religion | Hindu | 91 (36.30%) | 94 (37.50%) | 53 (21.10%) | 12 (4.80%) | 1 (0.40%) | 251 (84.2) | 0.360 |
| Others (Muslim, Sikh) | 16 (34.0%) | 15 (31.8%) | 9 (1.2%) | 6 (15.80%) | 0 (0.00%) | 46 (15.8) |
| Locality | Rural | 29 (28.70%) | 43 (42.60%) | 23 (22.80%) | 6 (5.90%) | 0 (0.00%) | 101 (34.3) | 0.343 |
| Urban | 78 (39.80%) | 66 (33.70%) | 39 (19.90%) | 12 6.10%) | 1 (0.50%) | 196 (65.7) |
chi-square test was used
Discussion
After the statistical analysis of present study, it was finally observed that maximum patients were having depressive symptoms as compared to the anxiety symptoms. About 64% of the population had depressive symptoms and 61% had anxiety symptoms. In present study, it was observed that males, elderly and married population were more prone to the psychological impact. Male were affected more, which can be because of the fact they have bear more responsibilities and also were afraid that if their family members also acquire the illness who will manage them. In the same married patients were more concerned about the family members and their health, which led to apprehension and further to the anxiety symptoms. People residing in the urban area showed more anxiety and depressive symptoms.
The findings were supported by the study on migrant workers by Kumar K et al., in Chandigarh, in which about 73.5% of the participants were found to be positive for depression and 50% of the participant were found to be positive for anxiety on the Generalised Anxiety Disorder-2 (GAD) [11]. Also, in another study more than half (71.8%) of the patients showed the depressive symptoms [12]. In a study by Varshney M et al., 15.0% had mild psychological impact and 5.5% had moderate psychological impact [13]. However, 12.7% reported severe psychological impact [13]. It implies that maximum patients had mild psychological impact which was similar to present study findings which showed that maximum population was having mild amount of anxiety and depression.
In total, 25% and 28% of the participants were moderate to extremely severely depressed, and anxious, respectively in a study by Verma S and Mishra A [14]. Similarly, in present study also, about 27% patient was moderate to severely depressed and about 20% were moderate to severely anxious.
In another study, about 66% of the population were in the normal range of the psychological and emotional distress and 3.4% were in the range of severe distress [15]. Also, according to Wang C et al., about three fourth of the population showed the psychological impact in form of depressive symptoms [16]. As per present study results, the three-fourth of patients had psychological impact in form of depressive and anxiety symptoms of different degrees.
Among the 500 respondents in the study, 19% had depressive symptoms with the score ≥10 on the scale physical health questionnaire-9 and 14% had anxiety symptoms [17]. While in present study, 64% had depressive and 61% had anxiety symptoms. The reason behind such difference may be because of their large sample size, covering various cities, and also the study was done in the initial days of the COVID in March, during which it was a havoc for the general population. In the score of “Perceived Helplessness”, the subscale of perceived stress scale-10, with female patients showing higher scores compared to male patients (p=0.010) in a study done by Guo Q et al., [18]. But in present study, male patients were more affected with the psychological impact in comparison with the females which can be better explained by the fact that in present study population had majority of the male members.
So, seeing the psychological impact of COVID-19, there is a need for early detection and the importance of picking up and effectively treating the milder clinical mood symptoms or sub-threshold syndromes before they evolve to more complex and enduring psychological responses like depression, anxiety and post-traumatic stress disorder. Therefore, all the higher authorities including the government and the medical should take charge and execute suitable course of action, such as providing psychological guidance, to prevent, reduce or manage increased anxiety among the general population, during the COVID-19 pandemic.
Limitation(s)
The sample size was small, due to which results cannot be generalised. Also, due to lack one to one communication, the important aspects of mental status examination were missed.
Conclusion(s)
COVID-19 had a significant psychological impact on the patients in form of anxiety and depressive symptoms. People became more concerned about the complications. Severe cases of the disease can lead to heart, and respiratory failure, acute respiratory syndrome, or even death. In addition to the physical impacts, COVID-19 can have serious effects on people’s mental health. Fear of complications was most commonly seen in the patients. Thus, it is essential to preserve the mental health of individuals. Therefore, government should employ teams of physicians and psychiatrist to help to formulate the psychological intervention in order to prevent the patients landing into short term or a long-term psychiatric illness. The physical complaints may wean off, but psychological complications may hamper the quality of life of the patients. Therefore, monitoring and oversight of the population mental health during crisis such as a pandemic is an immediate priority.
chi-square test was used; *significant
chi-square test was used
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 02, 2020
Manual Googling: Dec 24, 2020
iThenticate Software: Jan 20, 2021 (13%)
[1]. WHO. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/?gclid=EAIaIQobChMIrKv17Zqm6gIV2AorCh36hQDREAAYASAAEgKC_vD_BwE [Google Scholar]
[2]. Coronavirus. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019. [Last accessed on 2020 Mar 30] [Google Scholar]
[3]. India COVID-19 Tracker. Available from: https://www.covid19india.org/. [Last accessed on 2020 Mar 30] [Google Scholar]
[4]. Ministry of Health and Family Welfare. GOI RSS. Available from: https://www.mohfw.gov.in/. [Last accessed on 2020 Mar 30] [Google Scholar]
[5]. Wheaton MG, Abramowitz JS, Berman NC, Fabricant LE, Olatunji BO, Psychological predictors of anxiety in response to the H1N1 (Swine Flu) pandemicCognitive Therapy and Research 2012 36:210-18.10.1007/s10608-011-9353-3 [Google Scholar] [CrossRef]
[6]. Salari N, Hosseinian-Far A, Jalali R, Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysisGlobal Health 2020 16(1):5710.1186/s12992-020-00589-w32631403 [Google Scholar] [CrossRef] [PubMed]
[7]. Hamilton M, The assessment of anxiety states by ratingBr J Med Psychol 1959 32(1):50-55.10.1111/j.2044-8341.1959.tb00467.x13638508 [Google Scholar] [CrossRef] [PubMed]
[8]. Hamilton M, A rating scale for depressionJ Neurol Neurosurg Psychiatry 1960 23(1):56-62.10.1136/jnnp.23.1.5614399272 [Google Scholar] [CrossRef] [PubMed]
[9]. Maier W, Buller R, Philipp M, Heuser I, The Hamilton Anxiety Scale: Reliability, validity and sensitivity to change in anxiety and depressive disordersJ Affect Disord 1988 14(1):61-68.10.1016/0165-0327(88)90072-9 [Google Scholar] [CrossRef]
[10]. Reynolds WM, Kobak KA, Reliability and validity of the Hamilton Depression Inventory: A paper-and-pencil version of the Hamilton Depression Rating Scale Clinical InterviewPsychological Assessment 1995 7(4):472-83.10.1037/1040-3590.7.4.472 [Google Scholar] [CrossRef]
[11]. Kumar K, Mehra A, Sahoo S, Nehra R, Grover S, The psychological impact of COVID-19 pandemic and lockdown on the migrant workers: A cross-sectional surveyAsian J Psychiatr 2020 :5310.1016/j.ajp.2020.10225232593970 [Google Scholar] [CrossRef] [PubMed]
[12]. Chakraborty K, Chatterjee M, Psychological impact of COVID-19 pandemic on general population in West Bengal: A cross-sectional studyIndian J Psychiatry 2020 62(3):266-72.10.4103/psychiatry.IndianJPsychiatry_276_2032773869 [Google Scholar] [CrossRef] [PubMed]
[13]. Varshney M, Parel JT, Raizada N, Sarin SK, Initial psychological impact of COVID-19 and its correlates in Indian Community: An online (FEEL-COVID) surveyPLoS ONE 2020 15(5):e023387410.1371/journal.pone.023387432470088 [Google Scholar] [CrossRef] [PubMed]
[14]. Verma S, Mishra A, Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19Int J Soc Psychiatry 2020 66(8):756-62.10.1177/002076402093450832567466 [Google Scholar] [CrossRef] [PubMed]
[15]. Feng MC, Wu HC, Lin HT, Lei L, Chao Lu CM, Yang WP, Exploring the stress, psychological distress, and stress-relief strategies of Taiwan nursing staffs facing the global outbreak of COVID-19Hu Li Za Zhi 2020 67(3):64-74. [Google Scholar]
[16]. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in ChinaInt J Environ Res Public Health 2020 17(5):01-25.10.3390/ijerph1705172932155789 [Google Scholar] [CrossRef] [PubMed]
[17]. Choi EPH, Hui BPH, Wan EYF, Depression and anxiety in Hong Kong during COVID-19Int J Environ Res Public Health 2020 17(10):374010.3390/ijerph1710374032466251 [Google Scholar] [CrossRef] [PubMed]
[18]. Guo Q, Zheng Y, Shi J, Wang J, Li G, Li C, Immediate psychological distress in quarantined patients with COVID-19 and its association with peripheral inflammation: A mixed-method studyBrain Behav Immun 2020 1591(20):30618-18.10.1016/j.bbi.2020.05.03832416290 [Google Scholar] [CrossRef] [PubMed]