Case Report
A 59-year female, home maker resident of Chennai, came with complaints of multiple joint pain since one-year duration involving large and small joints (bilateral knee, shoulder, elbow, wrist, carpometacarpal, and proximal inter phalangeal joints). It was insidious in onset and progressive in nature and associated with early morning stiffness. She had complaints of dyspnoea since 6 months which was gradual in onset and progressive in nature, aggravated by mild to moderate exertion and relieved by rest, which was not associated with chest pain, palpitations, syncope, orthopnoea and Paroxysmal Nocturnal Dyspnoea (PND).
Patient does not have any other co-morbid illnesses, no previous hospitalisation. There is no significant family history (No history of any autoimmune disorders in the family). She lives in a pucca house with closed drainage facilities and uses filtered water for drinking and cooking purposes.
On examination, patient was conscious, afebrile, oriented to time, place and person. Patient had pallor and there was no icterus, cyanosis, clubbing, lymphadenopathy and pedal oedema. On local examination of the joints, patient had swelling and tenderness over bilateral knee, wrist, proximal interphalangeal joints. Swan neck deformity of right index finger was observed.
Respiratory system examination revealed the trachea to be in midline, chest movements was normal, there was no scars, sinuses, no spinal deformities, impaired percussion note and velcro crepitations over bilateral infra-scapular regions. Cardiovascular system examination revealed normal first and second heart sounds without any murmurs. On gastrointestinal examination, abdomen was soft, there was no organomegaly and bowel sounds were heard. On neurological examination, higher functions, cranial nerves, motor and sensory functions were intact.
The patient was having multiple small and large joint pains with early morning stiffness which improves as the day progresses and swan neck deformity of right index finger noted-our first differential diagnosis was RA. Authors ruled out osteoarthritis since the joint pain improved as the day progressed. Patient was not having any psychiatric symptoms, sleep disturbances, paresthesia, cognitive disturbances which helped us in ruling out fibromyalgia (a disease which is common among females between 40-60 years of age and it usually presents as polyarthralgia).
Since, the patient had a symptom for more than six weeks and there was relative sparing of the metatarsophalangeal joints, there was absence of tophi possibilities of gouty arthritis is limited. Patient did not have fever and symptoms suggestive of an infective aetiology preceding joint involvement which helps us to rule out reactive arthritis. There were no skin manifestations in the form of rash, urticaria and oral ulcers, ophthalmic examination did not reveal uveitis, dry eyes reducing the possibilities of Sjogren’s syndrome and SLE.
Investigations showed normocytic normochromic anaemia with haemoglobin of 10.4 gm/dL, total white blood cell count of 13,700/mm3 with neutrophil predominance 88.2%, lymphocyte 7.2%, platelet count of 459,000/mm3. Urine routine and Renal Function Tests (Blood urea nitrogen and serum creatinine) were normal. Erythrocyte Sedimentation Rate (ESR) was 78 mm in one hour (elevated), C-Reactive Protein (CRP) was reactive 23.09, rheumatoid factor was positive (384 IU/mL) and Anti-Cyclic Citrullinated Peptide (Anti-CCP) was positive (159 U/mL).
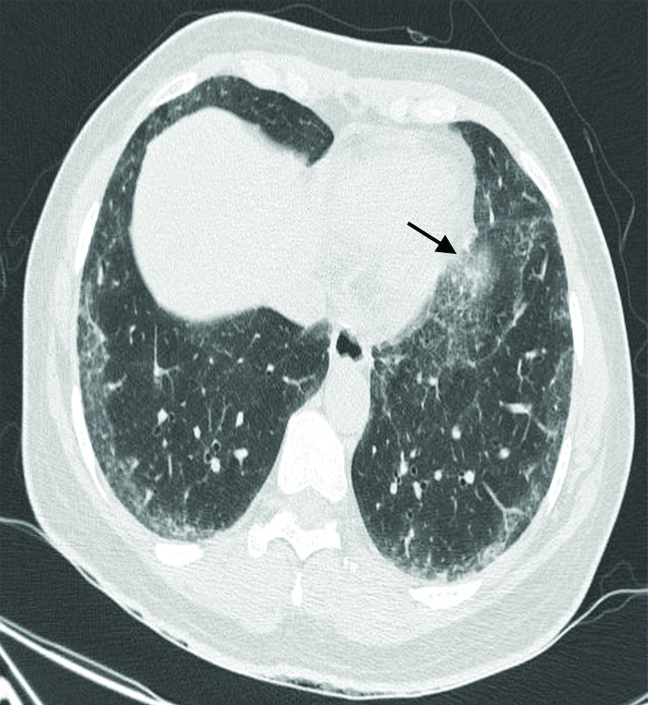
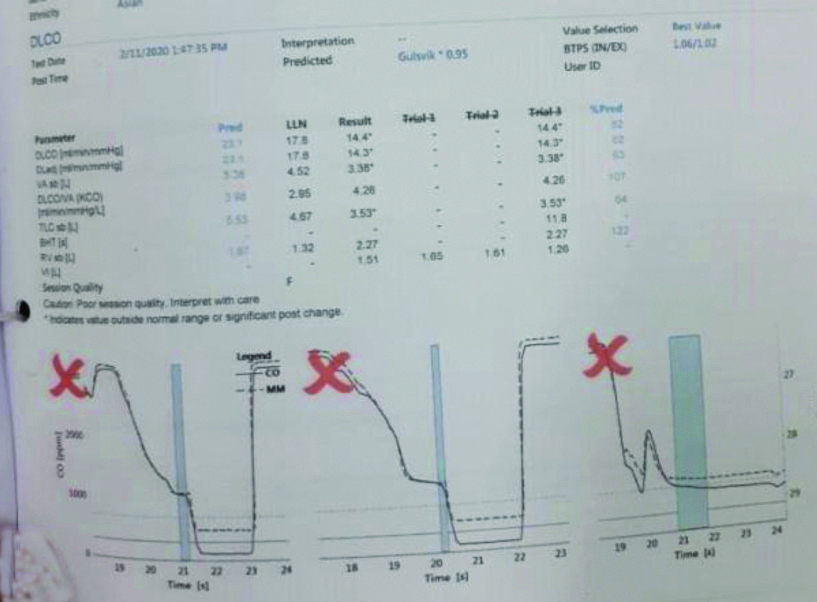
Patient satisfied European League Against Rheumatism (EULAR) [1] criteria for RA (patient had more than four small joints involvement [Table/Fig-1], with symptoms lasting for more than six weeks and her Anti-CCP, Rheumatoid factor, ESR and CRP was reactive). Chest X-ray and HRCT chest was done, it revealed evidence of subpleural reticulations noted involving posterior aspects of lung predominantly in lower lobes which was suggestive of Nonspecific interstitial pneumonia pattern of ILD [Table/Fig-2]. Pulmonary function test showed restrictive pattern with moderate severity [Table/Fig-3].
X-ray right wrist: Thumb metacarpophalangeal joint hyperextension (black arrow), Proximal interphalangeal joint erosion (white arrow).

Subpleural reticulations noted involving posterior aspects of lung predominantly in lower lobes (Black arrow).
Pulmonary function test: restrictive pattern.
Patient was diagnosed as RA with ILD. Patient was started on sulfasalazine 500 mg twice daily, Hydoxychloroquine 200 mg daily and high dose prednisolone 40 mg per day for ILD (Systemic steroids was tapered and was changed to maintenance doses). With hydroxychloroquine and sulfasalazine patients joint symptoms started to improve.
After six months on follow-up patient started to develop fever, malar rash and photosensitive rash on sun exposed areas (neck, shoulders and hands) over the past one month.
On examination patient had hyperpigmentation erythematous rims with central pallor, butterfly shaped rash present over cheeks and bridge of nose. Patient had oral ulcers over the hard palate which was not painful. Following which ANA was send which showed +++ cytoplasmic speckled positivity. Extractable nuclear antigen panel was sent which revealed a positive reaction for Anti-dsDNA and Anti-Histone was negative. Patient fulfilled the Systemic Lupus International Collaborating Clinics (SLICC) [2] criteria for SLE (fever, malar rash, oral ulcers, synovitis with ANA and Anti-dsDNA positivity).
Patient was diagnosed with Rhupus since the patient had features of erosive arthritis and manifestations of SLE. Sulfasalazine was stopped and the patient was started on high dose oral steroids tab prednisolone 40 mg and then was tapered on weekly basis and continued on 5 mg/day maintenance dose, hydroxychloroquine 200 mg twice daily and mycophenolate mofetil 500 mg twice a day following which patient’s dyspnea and joint pain started to improve, number of swollen and tender joints were reduced to less than 1, CRP and ESR was reduced from patient’s baseline value, rash and oral ulcers improved with treatment.
Discussion
Rhupus syndrome was first coined by Peter Schur in the year 1971, as patients who satisfied the criteria for both SLE and RA. Case definition of Rhupus was symmetrical and erosive polyarthritis which is accompanied by signs and symptoms of SLE, and the patient being reactive for specific immunological markers of SLE including Anti-dsDNA or Anti-Smith antibodies [3]. It has been observed that Rhupus as an entity is more common in females and in around 80% of patient’s RA was the initial presentation and remainder had a simultaneous onset of RA and SLE. Mean of age onset of the disease was 45 years [3].
Devrimsel G and Beyazal MS, reported three cases with Rhupus syndrome, all three patients had a history of polyarthritis predominantly involving the small joints of the hand, which was followed by skin manifestations including malar rash. Laboratory studies revealed an elevated ESR, CRP, ANA, RA factor and anti-CCP was reactive [3].
Sarkar S and Saha K, observed a 23 year old female patient who was diagnosed with RA presented with high grade fever and acute onset dysponea with polyarthritis, on examination she was having alopecia, oral ulcers, swan neck deformities of both bands with ulnar deviation of wrist joints. She didn’t improve with antibiotics (cefipime), HRCT chest revealed bilateral multiple lower lobe consolidation with pleural effusion. Laboratory investigations revealed a positive ANA, Anti-ds DNA, and RA factor, following which she was diagnosed with Rhupus syndrome presenting as pneumonitis. She was started on high dose IV steroids (methylprednisolone 1 gm for seven days) followed by oral prednisolone tapering course [4].
Nizami MF et al., reported a patient, 40-year-old male, who presented with polyarthritis involving small and large joints, thyroiditis, he had an elevated ESR and CRP, RA factor and Anti-CCP was found to be negative. He fulfilled the EULAR criteria for RA and was started on sulfasalazine, hydroxychloroquine and prednisolone. He later developed painless oral ulcers and was found to be positive for ANA and anti-ds DNA, following which he was diagnosed with Rhupus syndrome [5].
The index patient presented initially with polyarthritis and dyspnoea she was diagnosed with RA and ILD. She was started on hydroxycholoroquine, sulfasalazine and prednisolone. During follow-up after six months she developed a hyperpigmented rash over cheeks and bridge of nose, nonpainful oral ulcers with ANA showing speckled positivity and ENA panel showing positive anti-ds DNA and negative anti histone antibodies, she was diagnosed with Rhupus based on the clinical manifestations of both RA and SLE and she had symmetrical erosive joint disease, positive RA factor, Anti-CCP, Anti-dsDNA and ANA.
Extensive Human Leukocyte Antigen- DR Isotype (HLA-DR) testing has been done and it has been concluded by few studies that the Rhupus patients have distinctive HLA-DR subgroup involvement (HLA-DR4, DR2, DR6, DR1 alleles) when compared with SLE and RA patients, where there is an increased frequency of association between RA and HLA-DR1 and SLE with HLA-DR3. This has led to a conclusion that Rhupus can be a separate entity rather than a mere coincidence [6,7].
The most common symptom of Rhupus is symmetrical arthritis, joint swelling, morning stiffness, joint deformities and rheumatoid nodules. The presence of rheumatoid nodules in SLE patients should be considered as a risk factor for Rhupus syndrome and should be closely monitored. Rhupus patients have mild SLE activity and less involvement of visceral organ compared with isolated SLE patients. This maybe because of the immunoglobulin M-type of RF could compete with complement for binding to circulating immuno compounds, which, in turn, helps to protect the body from complement activation [6,8].
Tani C et al., Compared cases of rhupus with RA and SLE and they observed higher CRP reactivity and lower complement levels and higher ESR level when compared with patients with SLE. Patients with rhupus have 100% positivity to ANA and around 50% patients had a positive Anti-dsDNA [9].
Generally, treatment regimens including low-to-moderate dosages of systemic corticosteroids combined with 1-3 Disease-Modifying Antirheumatic Drugs (DMARDs) (e.g., methotrexate, leflunomide, hydroxychloroquine, sulfasalazine) [10]. From observations made by Benavente EPI and Paira SO and Seo SR et al., Rhupus patients clinically improved with mycophenolate mofetil, or cyclosporin (DAS 28 score improved significantly following initiation of MMF and cyclosporin) [11,12]. Piga M et al., did a pilot study to assess effects of Rituximab in patients with Rhupus and concluded that addition of Rituximab to the above mentioned regimen was associated with sustained improvement proven by improvement in DAS 28, SLEDAI scores [13].
Conclusion(s)
Two connective tissue disorders co-existing together is a rare entity and presence of RA and SLE in a same patient is a rare occurrence because of inverse or opposite immunopathological activity. Prevalence of organ damage in patients with rhupus is relatively rare but in our case the patient presented with a restrictive lung disease in addition. Such patients will be requiring high doses of corticosteroids to prevent the development of fibrosis. Thus, identifying this unique entity is important as treatment options varies between a patient who presents with RA or SLE when compared patients with rhupus.
[1]. Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiativeArthritis Rheum 2010 62(9):2569-81.10.1002/art.2758420872595 [Google Scholar] [CrossRef] [PubMed]
[2]. Hochberg MC, Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus [letter]Arthritis Rheum 1997 40:172510.1002/art.17804009289324032 [Google Scholar] [CrossRef] [PubMed]
[3]. Devrimsel G, Beyazal MS, Three case reports of rhupus syndrome: An overlap syndrome of rheumatoid arthritis and systemic lupus erythematosusCase Reports in Rheumatology 2018 2018:61947383 pages, 201810.1155/2018/619473829610698 [Google Scholar] [CrossRef] [PubMed]
[4]. Sarkar S, Saha K, Bilateral acute lupus pneumonitis in a case of rhupus syndromeLung India 2012 29:280-82.10.4103/0970-2113.9911922919171 [Google Scholar] [CrossRef] [PubMed]
[5]. Nizami MF, Sharma CB, Guria RT, Singh SK, A rare case of rhupus syndrome with Hashimoto’s thyroiditis, associated adverse effect of drugs and incidental findingsJ Family Med Prim Care 2019 8(9):3048-50.10.4103/jfmpc.jfmpc_568_1931681693 [Google Scholar] [CrossRef] [PubMed]
[6]. Simón JA, Granados J, Cabiedes J, Morales JR, Varela JA, Clinical and immunogenetic characterisation of Mexican patients with ‘rhupus’Lupus 2002 11(5):287-92.10.1191/0961203302lu189oa12090562 [Google Scholar] [CrossRef] [PubMed]
[7]. Brand CA, Rowley MJ, Tait BD, Muirden KD, Whittingham SF, Coexistent rheumatoid arthritis and systemic lupus erythematosus: Clinical, serological, and phenotypic featuresAnn Rheum Dis 1992 51(2):173-76.10.1136/ard.51.2.1731550399 [Google Scholar] [CrossRef] [PubMed]
[8]. Davis JS, Bollet AJ, Protection of a complement-sensitive enzyme system by [8]rheumatoid factorJ Immunol 1964 92:139-44. [Google Scholar]
[9]. Tani C, D’Aniello D, Delle Sedie A, Carli L, Cagnoni M, Possemato N, Rhupus syndrome: Assessment of its prevalence and its clinical and instrumental characteristics in a prospective cohort of 103 SLE patientsAutoimmun Rev 2013 12(4):537-41.10.1016/j.autrev.2012.09.00423063507 [Google Scholar] [CrossRef] [PubMed]
[10]. Li J, Wu H, Huang X, Xu D, Zheng W, Zhao Y, Clinical analysis of 56 patients with rhupus syndrome: Manifestations and comparisons with systemic lupus erythematosus: A retrospective case-control studyMedicine (Baltimore) 2014 93(10):e4910.1097/MD.000000000000004925170930 [Google Scholar] [CrossRef] [PubMed]
[11]. Benavente EPI, Paira SO, Rhupus: Report of 4 casesReumatol Clin 2011 7(5):333-35.10.1016/j.reumae.2010.12.003 [Google Scholar] [CrossRef]
[12]. Seo SR, Lee SJ, Park DJ, Kim TJ, Park YW, Lee SS, Successful treatment using cyclosporine in a patient with rhupus complicated by aplastic anaemia: A case report and review of the literatureClin Exp Rheumatol 2011 29(4):708-11.Epub 2011 Sep 1. PMID: 21813067 [Google Scholar]
[13]. Piga M, Gabba A, Cauli A, Garau P, Vacca A, Mathieu A, Rituximab treatment for ‘rhupus syndrome’: Clinical and power-Doppler ultrasonographic monitoring of response. A longitudinal pilot studyLupus 2013 22(6):624-28.Epub 2013 Apr 410.1177/096120331348274123559669 [Google Scholar] [CrossRef] [PubMed]