Lymphangioma Circumscriptum of the Vulva- A Case Series
Rashmi S Mahajan1, Yogesh S Marfatia2, Atmakalyani R Shah3, Kishan R Ninama4
1 Professor and Head, Department of Skin and Venereal Disease, SBKS Medical Institute and Research Center, Vadodara, Gujarat, India.
2 Professor, Department of Skin and Venereal Disease, SBKS Medical Institute and Research Center, Vadodara, Gujarat, India.
3 Resident, Department of Skin and Venereal Disease, SBKS Medical Institute and Research Center, Vadodara, Gujarat, India.
4 Associate Professor, Department of Skin and Venereal Disease, SBKS Medical Institute and Research Center, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Atmakalyani R Shah, 68, Vama Hostel, Sumandeep Vidyapeeth, Piparia, Waghodia, Vadodara-391760, Gujarat, India.
E-mail: juishah13@gmail.com
Vulval dermatoses pose a diagnostic and therapeutic challenge for the dermatologists. Lymphangioma Circumscriptum (LC) is a form of lymphangioma affecting the skin and subcutaneous tissues that is characterised by benign dilation of lymphatic channels. This uncommon condition is known to occur over the chest, mouth, axilla, tongue, and rarely in the vulva. In this series, authors present three cases of LC of vulva in women between the age group of 45 to 60 years with late-onset fluid-filled lesions over the vulva. The first case had history of hysterectomy prior to onset of lesions, the second case had a spontaneous onset of lesions while the third was a suspected case of pelvic tuberculosis with secondary lymphangioma.
Lymphangiectasia, Vulvar, Vulval epithelium
Introduction
Disorders of vulval epithelium are a confusing spectrum of disorders. They are broadly classified as-1) Inflammatory, 2) Ulcerative and Bullous, 3) Infections, 4) Benign tumours and 5) Malignancies. It is essential to know the exact aetiology to plan successful therapy.
LC is a benign lymphatic malformation characterised by dilation of lymphatic vessels in the skin and subcutaneous tissue with lesions erupting locally as isolated or grouped translucid, thin-walled vesicles filled with a clear liquid [1]. These pathological lymphatic malformations have no communication with the normal lymphatics [2]. The precise cause of LC is not established. It could be congenital or acquired as a result of damage to the lymphatic vessels secondary to various aetiologies. The chest, mouth, axilla and tongue are the commonly affected sites while vulva is an infrequently encountered site for LC [1]. Herein, authors report three cases of LC of vulva in women between the age group of 45 to 60 years who presented with late-onset fluid-filled lesions over the vulva.
Case Series
Case 1
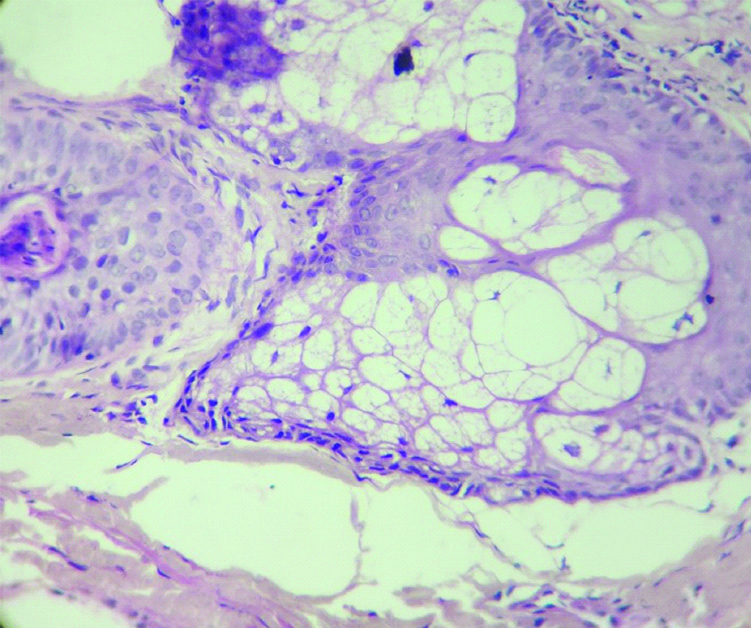
A 56-year-old female presented with asymptomatic swelling and skin lesions over genitalia since two years. She gave a history of spontaneous fluid discharge from lesions and incomplete healing of lesions inspite of various topical treatments. She had undergone total vaginal hysterectomy two and a half years back. There was no history of weight loss, pelvic tuberculosis, chemotherapy or radiotherapy in the past. Examination revealed multiple grouped vesicles and papules in a “Frog spawn” appearance with marked oedema over right labia [Table/Fig-1]; on puncturing a vesicle with a 26 gauze needle, clear fluid was visible. Punch biopsy taken from a vesicle over the right labia showed dilated lymph vessels with large cystic spaces in the deep dermis and hyperplastic squamous epithelium, suggestive of LC [Table/Fig-2]. The patient was treated in three sittings of cryotherapy at weekly intervals which led to partial regression of lesions.
A 56-year-old female with multiple grouped vesicles and papules in a “frogspawn appearance” with marked oedema over right labia.

Hyperplastic squamous epithelium. The upper dermis showing band like lymphocytic infiltrate while deep dermis shows few dilated lymph vessels. (H&E, 40X)
Case 2
A 60-year-old female presented with multiple tiny fluid-filled lesions over genitalia since 8-10 years. The onset of the lesions was spontaneous with gradual progression in number and size of lesions. She had taken multiple topical treatments and cryotherapy in the past with no response. Past history of hypothyroidism and bilateral Knee replacement was done few years ago. There was no past history of any abdominal surgery and ultrasonography was normal. On examination grouped vesicles and papules resembling “Frog spawn” over bilateral labia were seen [Table/Fig-3]. On puncturing a vesicle with a 26 gauze needle, serosanguinous fluid was observed. The patient refused a skin biopsy and a provisional diagnosis of LC was made.
Grouped vesicles and papules resembling “Frog spawn” seen over bilateral labia in a 60-year-old female.

Case 3
A 47-year-old female was referred from Gynaecology Out Patient Department for skin lesions over the vulva since 8-12 months. There was history of discharge of clear fluid from the lesions. She gave history of lower abdominal pain with weight loss since past 6-8 months. On examination, multiple grouped vesicles and papules were seen over bilateral labia [Table/Fig-4]. Routine investigations revealed anaemia (haemoglobin 10.2 g/dL) and raised Erythrocyte Sedimentation Rate (ESR) (31 mm/hr) while other biochemical parameters were within normal limits. Her mantoux test was positive (1.5 cm). Ultrasonography of the abdomen and pelvis showed multiple, enlarged, abnormal morphology lymph nodes in the pre and para aortic region, few of them being necrotic, suggestive of infective aetiology. The patient was counselled for skin biopsy, Acid Fast Bacilli (AFB) culture, Cartridge Based Nucleic Acid Amplification Test (CB-NAAT) and AFB staining but did not consent for the same. A provisional diagnosis of acquired LC due to pelvic tuberculosis was considered. However, the patient was lost to follow-up.
A 47-year-old female with multiple grouped vesicles and papules in a “frog spawn appearance” seen over bilateral labia.

Discussion
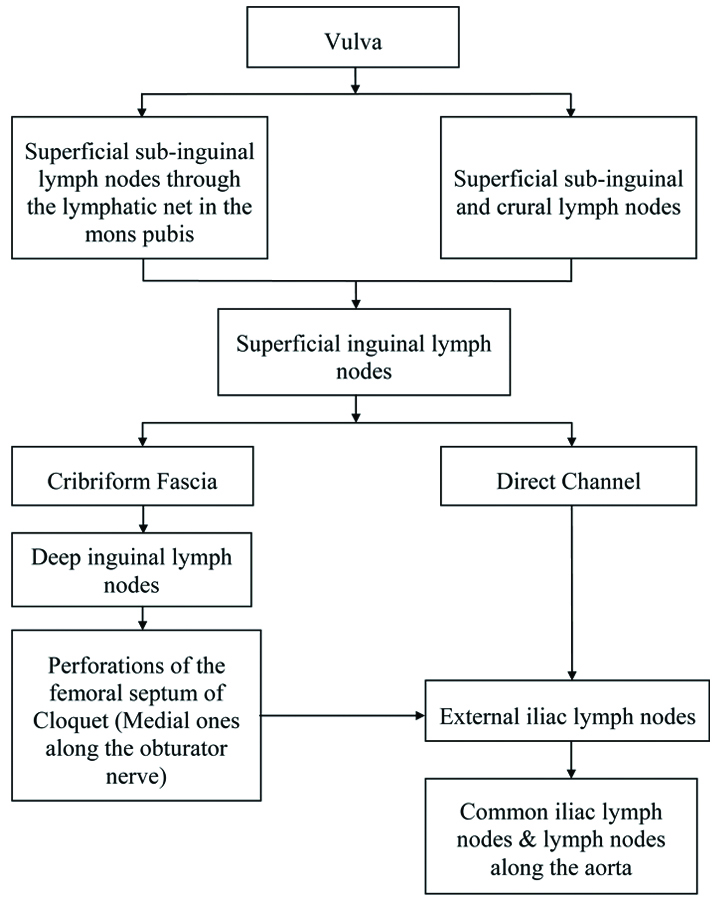
The vulva has an exceptionally abundant lymphatic system, the channels forming a fine network [Table/Fig-5]. Lymphatic Malformations (LM) are congenital disorders which consist of vesicles or large cysts filled with lymphatic fluid. They can be divided into microcystic lesions (LC) and macrocystic LM (diameter greater than 1 cm, previously known as cystic hygroma) which may be diagnosed in-utero as early as the first trimester of pregnancy. While most LMs are diagnosed during infancy, before the age of two years, some can manifest only at puberty or during adulthood. LMs occur sporadically in contrast to primary lymphedema that can be inherited as an autosomal dominant trait in up to 20% of cases [3]. Aetiology may be related to lymph vessel obstruction or lymphedema. Lymphangiogenic growth factors, Vascular Endothelial Growth Factor - C (VEGF- C) and VEGF-D along with their receptors on the lymphatic endothelial cells, VEGFR-3 have been found to play a role [4].
Lymphatic drainage of the vulva.
Classification of lymphangiomas is confusing and is given by some authors as shown in [Table/Fig-6] [5-7].
Classification of lymphangiomas [5-7].
| Authors Name/Reference No. | Classification |
|---|
| Peachy RDG and Lim CC [5] | • Classic• Localised |
| Lever WF and Schaumburg-Lever G [6] | • Localised- Presentation: at any age- No specific sites of predilection• Classic- Presentation: at birth or early in life- Predisposed sites: proximal portion of limbs, areas adjacent to limb girdles• Cavernous• Progressive |
| Fisher I and Orkin M [7] | Acquired lymphangioma or lymphangiectasis (obstruction to local lymph vessels) |
The vulva is an unusual site for lymphangioma. It is characterised by thin-walled grouped vesicles resembling a frog spawn [Table/Fig-7] [8] and is caused by accumulation of lymphatic fluid in the extracellular space due to lymphatic dysfunction (lymphedema) [3]. It may be primary or secondary [Table/Fig-8]. The differential diagnosis that can be considered at this location and the possible complications are mentioned in [Table/Fig-9]. Diagnosis is usually clinical but biopsy, nuclear magnetic resonance, lymphangiography and ultrasound are useful [1,8].
Frog spawn (Credits: https://eastdartmoorwoods.org/2020/02/29/frogspawn-february/).

Allen’s Classification of lymphedema based on aetiology [8].
| Primary lymphedema | Secondary lymphedema |
|---|
| • Types- Congenital lymphedema (Milroy’s disease)- Lymphedema Praecox(Meige’s syndrome - presenting before 35 years of age) - Lymphedema tarda (presenting after 35 years of age)• May be isolated or part of a syndrome (Turner’s syndrome, Noonan’s syndrome, Proteus syndrome, Incontinentia Pigmenti, Yellow nail syndrome, Lymphedema-distichiasis syndrome) | • More common• Pathogenesis- Result of acquired obstruction or obliteration of lymph-conducting pathways leading to build-up of lymph in superficial vessels and subsequent formation of lesions. - Architectural disruption causes dilatation and sequestration of lymphatic channels which were previously normal• Causes - Malignancies - Kaposi’s sarcoma, Lymphoma or Infiltrative tumour- Iatrogenic due to radical lymph node excision or radiotherapy- Bacterial Infections- Filariasis- Podoconiosis- Lymphogranuloma Venereum- Tuberculosis- Cat-Scratch Disease- Post-Phlebitic Syndrome- Venous Ulcers- Accidental or self-inflicted trauma (repeated application of tourniquet to wrist (Secrétan’s syndrome))- Inflammatory conditions (Rosacea, Sarcoidosis, Rheumatoid Arthritis, Crohn’s Disease) |
Lymphangioma circumscriptum: Various differential diagnosis, complications and treatment options [1,3,4,8,9].
| Differential diagnosis | • Acquired Lymphangiectasia due to Radiotherapy or Crohn’s Disease• Molluscum Contagiosum• Tuberculosis Verrucosa Cutis• Venereal Lymphogranuloma• Leiomyoma• Malignant Tumour• Condyloma Acuminatum• Genital Herpes• Filariasis• Epidermal Cysts• Steatocystoma Multiplex• Fox-Fordyce Disease• Cherry Hemangioma• Angiokeratoma |
| Complications | • Cellulitis• Secondary Infections• Minor Haemorrhages• Psychosexual Dysfunction• Hidradenitis Suppurativa• Squamous Cell Carcinoma• Lymphangiosarcoma |
| Treatment options | • Electrocoagulation• Superficial Radiotherapy• Cryosurgery• Surgical Extirpation• Argon Laser Surgery• Carbon Dioxide Laser- Best results (superficial lymph vessel pulverised to seal the deep cisterns) • Ultra-Pulse High Energy CO2• Tunable Dye Lasers• Injection of a Sclerosant (Hypertonic Saline or Doxycycline) into the Cistern |
Treatment for LC is intended in the presence of recurrent infection, persistence of exudative lymphatic fluid or blood and for cosmetic purposes. The various forms of therapy are elucidated in [Table/Fig-9]. High degree of recurrence is seen unless the deep lymphatic cisterns are precisely managed. Curative treatment is radical surgical excision of lesions to eliminate both the superficial portion and the deep lymphatic cisterns [1,8].
Idiopathic LC in a 60-year-old female has been reported by Sinha A et al., who had complete clearance after vulvectomy [4]. Esquivias Gómez JI et al., have reported a case of a 44-year-old woman with LC of the vulva secondary to chronic idiopathic lymphedema of the right lower limb [1]. LC occurring as late as 13 years following hysterectomy has been reported by Sobti A et al., [9].
Conclusion(s)
A high index of suspicion is required to the untrained eye to diagnose LC on the vulva. All possible aetiologies should be considered. Pricking of the lesion with a sterile needle often causes oozing of clear fluid which is a clue to the diagnosis. Histopathology is a vital tool to establish the final diagnosis. These cases were reported because of their rare site of presentation.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 05, 2020
Manual Googling: Nov 24, 2020
iThenticate Software: Dec 21, 2020 (13%)
[1]. Esquivias Gómez JI, Miranda-Romero A, Cuadrado Vallés C, Bajo del Pozo C, Sánchez Sambucety P, Martínez Fernández M, Lymphangioma circumscriptum of the vulvaCutis 2001 67:229-32. [Google Scholar]
[2]. Whimster IW, The pathology of lymphangioma circumscriptumBr J Dermatol 1976 94(5):473-86.10.1111/j.1365-2133.1976.tb05134.x1268059 [Google Scholar] [CrossRef] [PubMed]
[3]. Boom LM, Vikkula M, Section 28: The Skin in Inflammatory and Other Vascular Disorders, Chapter 172: Vascular malformations, Fitzpatrick Dermatology in General medicine 2012 8th ed:2086-89. [Google Scholar]
[4]. Sinha A, Phukan JP, Jalan S, Pal S, Lymphangioma circumscriptum of the vulva: Report of a rare caseJ Midlife Health 2015 6(2):91-93.10.4103/0976-7800.15896826167062 [Google Scholar] [CrossRef] [PubMed]
[5]. Peachy RD, Lim CC, Whimster IW, Lymphangioma of skin. A review of 65 casesBr J Dermatol 1970 83(5):519-27.10.1111/j.1365-2133.1970.tb15735.x5484713 [Google Scholar] [CrossRef] [PubMed]
[6]. Lever WF, Schaumburg-Lever G, Histopathology of the Skin 1989 7th edPhiladelphia, PaLippincott-Raven [Google Scholar]
[7]. Fisher I, Orkin M, Acquired lymphangioma (lymphangiectasis)Arch Dermatol 1970 101(2):230-34.10.1001/archderm.101.2.2305413258 [Google Scholar] [CrossRef] [PubMed]
[8]. Rao R, Shenoi S, Diseases of Arteries, Veins And Lymphatics, Iadvl Textbook Of Dermatology3rd ed:726-730. [Google Scholar]
[9]. Sobti A, Wee DA, Tan KB, Acquired vulvar lymphangioma circumscriptumAstrocyte 2016 3(3):162-64.10.4103/astrocyte.astrocyte_5_17 [Google Scholar] [CrossRef]