Cystic lesions of the adrenal gland are usually rare, seen in 1/5750 to 1/250,000 of the population. They may be true cysts, infectious cysts, malignancies with cystic degeneration, or pseudocysts. Adrenal cysts are rare in the differential diagnosis of Retroperitoneal Cysts (RPC) and may be treated. They can be correctly identified through pathological testing. Here, the author presents a case of giant adrenal cyst in a young 38-year-old female.
Case Report
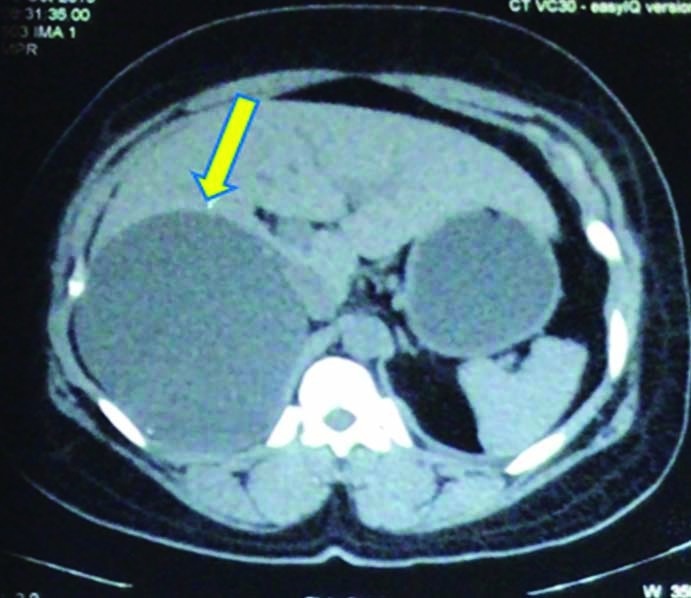
A 38-year-old female was admitted to the Department of General Surgery in October 2019 with a history of a mass in the right upper abdomen associated with pain, which is burning in nature and radiating to the back for three months. There was no similar complaint in past. On physical examination, a large non-tender lump of size 15×10 cm was palpable in the right upper abdominal region occupying the right hypochondrium and extending up to the lumbar area. After the clinical examination, the diagnosis of a retroperitoneal mass in right hypochondrium was made. The differential diagnosis was adrenal mass, cystic disease of lymphatics (chylolymphatic cyst), malignant connective tissue tumours, retroperitoneal lymphadenopathy, RPC, and retroperitoneal sarcoma. An abdominal ultrasound showed a large cystic lesion (maximum diameter, 10 cm) in the upper abdomen. Patient Contrast-Enhanced Computerised Tomography (CECT) [Table/Fig-1,2] revealed a complex retroperitoneal thin-walled cystic lesion measuring 12.5 (CC)×9.8 (TS)×12.1 (AP) cm near the liver abutting the right kidney. Punctate foci of wall calcifications were observed in the cyst. There was no evidence of wall enhancement or enhancing solid components in the lesion.
CECT image of retroperitoneal cyst sagittal section revealing complex retroperitoneal thin-walled cystic lesion measuring 12.5 (CC)×9.8 (TS)×12.1 (AP) cm near the liver abutting right kidney.

CECT image of reteroperitoneal cyst coronal section cyst marked with yellow arrow near the liver abutting right kidney.
The patient underwent exploration laparotomy as the origin of the lesion remained uncertain. Upon entering the abdomen, a large thin-walled cystic lesion was visible as arising from the retroperitoneum on the undersurface of the liver, displacing the right kidney downwards and medially and also the hepatic flexure of the colon completely downward [Table/Fig-3]. By combining sharp and blunt dissection, cystic lining was completely removed. Complete excision of the cyst was carried out [Table/Fig-4]. The postoperative period was uneventful and the patient was discharged on postoperative day 7.
Image showing intraoperative view of the cystic lesion under surface of liver, displacing the right kidney downwards and medially and also the hepatic flexure of colon completely downward taken during dissection.
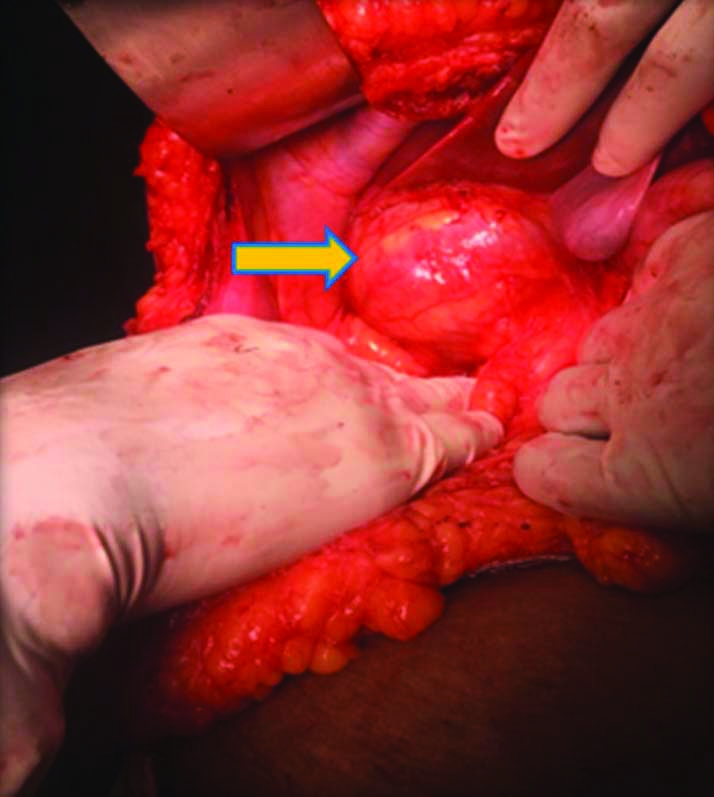
Postoperative view of the excised cyst sent for histopathological examination.

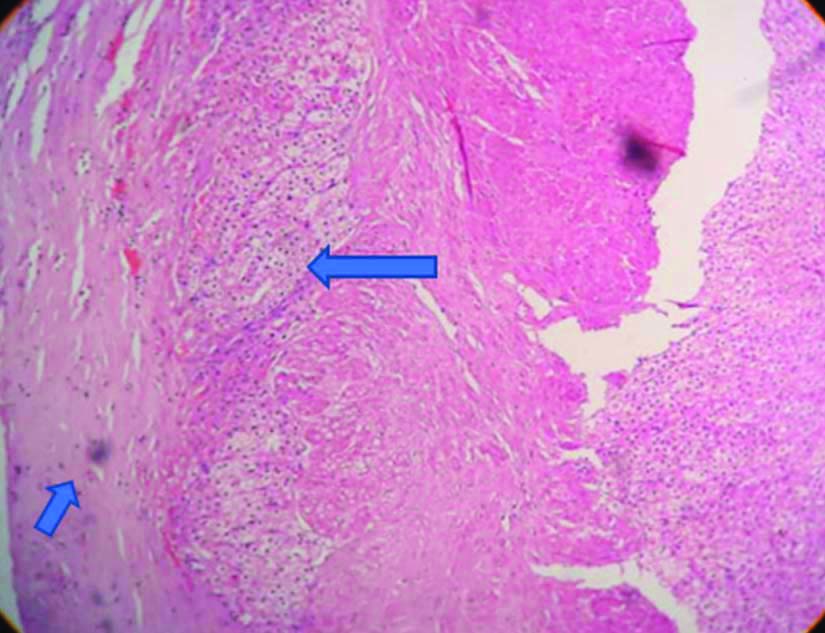
The gross features of a histopathological section of cyst measuring 15×10×1 cm showed a thin cyst wall with focal thickened areas showing multiple yellow nodules and the inner surface had disclosed multiple tiny papillary projections. Microscopically, papillary projections lined by cuboidal to flattened epithelium with hyalinised core was found with underlying hyalinised fibro collagenous and muscular tissue. Lymphoplasmacytic infiltrate, foamy macrophages were evident and focal calcification was found. Periphery was attached to the adrenal gland suggestive of the benign adrenal cyst [Table/Fig-5]. The patient was followed-up for the past six months and no other signs or symptoms were noticed.
Microscopy showing papillary projections lined by cuboidal to flattened epithelium with hyalinised core with underlying hyalinised fibro collagenous and muscular tissue. Periphery was attached to adrenal gland suggestive of benign adrenal cyst (Haematoxylin and Eosin stain, 40x magnification).
Discussion
This clinical case report prompts the diagnostic methods and clinical treatment of RPC lesions. These masses emerge inside the retroperitoneal space, which is a complex region behind the peritoneum [1-3]. There are several organs in this area (such as the adrenal and kidney glands, parts of the duodenum, the pancreas, the colon, and the oesophagus), major arteries (the aorta and the inferior cava vein), deep lymphatic vessels and structures, ligaments and fatty tissues [4]. Neoplasms rarely occur in the retroperitoneal space.
RPC masses are difficult to diagnose and pose a challenge to the surgeon in deciding the treatment modality. Preoperative diagnostic assessment should include careful recording of patients’ history, laboratory, and radiographic investigations. Even with the use of multiple diagnostic modalities, the organ of origin of many cystic lesions cannot be determined preoperatively.
To identify these lesions, the most detailed classification and analysis reported by Dr. Yang and colleagues are summarised here. A broad variety of neoplastic lesions (cystic lymphangioma, mucinous cystadenoma, cystic teratoma, cystic mesothelioma, Mullerian cyst, epidermoid cyst, bronchogenic cyst, cystic changes in solid neoplasms, pseudomyxoma retroperitoneal) and non-neoplastic lesions (pancreatic pseudocyst, nonpancreatic pseudocyst, lymphocele, urinoma, and haematoma) can be included in the differential diagnosis of RPC [5].
Cystic lymphangiomas are benign congenital malformations characterised by defective lymphatic tissues that do not interact with normal lymphatic channels. These lesions are more prevalent in males and can develop at any age, while children below two years of age have them in 90% of the cases [6-8]. The acquired types of cystic lesions can result from trauma, inflammation, or lymphatic obstruction.
A neoplasm constitutes of multiple tissues that are not native to the area where it is created is a cystic teratoma. This neoplasm consists of all the three germinal layers i.e., endoderm, mesoderm, and ectoderm [8]. Cystic teratomas typically occur in adults and children within the gonadal and sacrococcygeal areas, although they are much less common in the retroperitoneum [9].
The unilocular cysts present in women with normal ovaries are homogeneous and well-defined mucinous cystadenomas [10]. The pathogenesis remains uncertain, but it has been proposed that these lesions originate from peritoneal invagination, with mucinous metaplasia and cyst formation arising from them.
Pseudomyxoma retroperitoneal typically develops clinically with abdominal or lumbar discomfort and a palpable mass. In some conditions, abscess development is likely with a high fever or discharge, and weight loss can also be observed.
Benign cutaneous tumours often appear in epidermoid cysts, but they are often rarely found in RPCs [11]. The histological section reveals the presence of squamous epithelium, with a mixture of desquamated waste, cholesterol, keratin, and water, and is the characteristic of epidermoid cysts.
The bronchogenic cyst is a spherical cyst that originates as an embryonic pouch in the foregut or trachea during the fifth week of gestation. The cyst typically occurs in the mediastinum or the lung and is usually asymptomatic. Infection is the main concern of this form of the lesion. These cysts are exceptionally rare inside the retroperitoneal space with a particularly complicated differential diagnosis [12].
The adrenal cyst is an unusual condition that accounts for about 5% of adrenal lesions diagnosed erroneously. These cysts most commonly happen in the fourth and fifth decades of life. Adrenal cysts may be included in the differential diagnosis of cystic abdominal lesions and, if suspected, by checking for urinary catecholamines and/or metanephrines, the functional state of a person should be checked [13]. In the present case, functional tests were not done, as the patient was asymptomatic.
CT scan offers discrete sectional images of the organs and retroperitoneal compartments and, in a few cases, knowledge of the most important radiological features enables sufficient lesion characterisation in conjunction with clinical details. It can therefore be considered suitable for evaluating RPCs.
Diagnostic procedure consisted of sonography guided lesion drainage. This technique made it possible to minimise the compression of the underlying materials and to research the essence of the cystic liquid. No neoplastic cells, bacteria or pancreatic enzymes were actually detected. In the absence of these elements, the successful diagnosis of this lesion was only speculative. It was determined that it was only possible to monitor the progression of the residual lesion, taking into account the risks of surgical examination of the region between the aorta and the cava. No regression of the cystic lesion was observed after three and six months, in particular. A lack of regression has reinforced the cystic lesion as benign condition as time has progressed. The present study identified this clinical case and analysed the literature to emphasise how, on the basis of surgical removal complications, CT scan evidence, retroperitoneal cystic lesions must be treated on a case by case basis. Invasive surgical procedures should not be conducted on all lesions, and a complicated near follow-up technique can therefore be compulsory [14].
Conclusion(s)
RPCs are rare and it is difficult to arrive at the exact diagnosis preoperatively, in most cases. Adrenal cysts can be considered in the differential diagnosis of RPC and computerised tomography is preferred as the radiographic imaging modality of choice for the preliminary evaluation.
[1]. Davenport M, Pollard K, Smith SE, MacMahon MJ, Adrenal cysts-report, review, and classificationPostgrad Med J 1988 64:71-73.10.1136/pgmj.64.747.713420063 [Google Scholar] [CrossRef] [PubMed]
[2]. Osman S, Lehnert BE, Elojeimy S, Cruite I, Mannelli L, Bhargava P, A comprehensive review of the retroperitoneal anatomy, neoplasms and pattern of disease spreadCurr Probl Diagn Radiol 2013 42:191-208.10.1067/j.cpradiol.2013.02.00124070713 [Google Scholar] [CrossRef] [PubMed]
[3]. Tan JJ, Tan KK, Chew SP, Mesenteric cysts: An institution experience over 14 years and review of literatureWorld J Surg 2009 33:1961-65.10.1007/s00268-009-0133-019609826 [Google Scholar] [CrossRef] [PubMed]
[4]. Tirkes T, Sandrasegaran K, Patel AA, Hollar MA, Tejada JG, Tann M, Peritoneal and retroperitoneal anatomy and its relevance for cross sectional imagingRadiographics 2012 32:437-51.10.1148/rg.32211503222411941 [Google Scholar] [CrossRef] [PubMed]
[5]. Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, Retroperitoneal cystic masses: CT, clinical and pathological findings and literature reviewRadiographics 2004 24:1353-65.10.1148/rg.24504501715371613 [Google Scholar] [CrossRef] [PubMed]
[6]. Gümüstas OG, Sanal M, Güner O, Tümay V, Retroperitoneal cystic lymphangioma: A diagnostic and surgical challengeCase Rep Pediatr 2013 2013:29205310.1155/2013/29205323533897 [Google Scholar] [CrossRef] [PubMed]
[7]. Waldhausen JH, Holterman MJ, Tapper D, Identification and surgical management of cystic retroperitoneal lymphangioma in childrenPediatr Surg Int 1996 11:283-85.10.1007/BF0017844124057641 [Google Scholar] [CrossRef] [PubMed]
[8]. Ashley DJ, Origin of teratomasCancer 1973 32:390-94.10.1002/1097-0142(197308)32:2<390::AID-CNCR2820320216>3.0.CO;2-W [Google Scholar] [CrossRef]
[9]. Sasi W, Ricchetti GA, Parvanta L, Carpenter R, Giant mature primary retroperitoneal teratoma in a young adult: Report of a rare case and literature reviewCase Rep Surg 2014 2014:93053810.1155/2014/93053825506459 [Google Scholar] [CrossRef] [PubMed]
[10]. Yan SL, Lin H, Kuo CL, Wu HS, Huang MH, Lee YT, Primary retroperitoneal mucinous cystadenoma: Report of a case and review of the literatureWorld J Gastroenterol 2008 14:5769-72.10.3748/wjg.14.576918837099 [Google Scholar] [CrossRef] [PubMed]
[11]. Fdili Alaoui FZ, Oussaden A, Bouguern H, El Fatemi H, Melhouf MA, Amarti A, Giant pelvic retroperitoneal epidermoid cyst: A rare case reportCase Rep Med 2012 2012:98138710.1155/2012/98138723150734 [Google Scholar] [CrossRef] [PubMed]
[12]. Govaerts K, Van Eyken P, Verswijvel G, Van der Speeten K, A bronchogenic cyst, presenting as a retroperitoneal cystic massRare Tumours 2012 4:e1310.4081/rt.2012.e1322532911 [Google Scholar] [CrossRef] [PubMed]
[13]. Sioka E, Symeonidis D, Chatzinikolaou I, Koukoulis G, Pavlakis D, Zacharoulis D, A giant adrenal cyst difficult to diagnose except by surgeryInt J Surg Case Rep 2011 2:232-34.10.1016/j.ijscr.2011.05.00722096737 [Google Scholar] [CrossRef] [PubMed]
[14]. Morotti A, Busso M, Barozzino MC, Cinardo P, Angelino V, Familiari U, Detection and management of retroperitoneal cystic lesions: A case report and review of the literatureOncol Lett 2017 14(2):1602-08.10.3892/ol.2017.632328789385 [Google Scholar] [CrossRef] [PubMed]