Subarachnoid Block in a Patient with Ebstein’s Anomaly Posted for Total Abdominal Hysterectomy
Jayshri Desai1, Jayati Bhabutmal Jain2, Venkata Suryanarayana Gopavajhula3
1 Professor, Department of Anaesthesia, Smt. BK Shah Medical Institute and Research Centre, Vadodara, Gujarat, India.
2 3rd Year Resident, Department of Anaesthesia, Smt. BK Shah Medical Institute and Research Centre, Vadodara, Gujarat, India.
3 2nd Year Resident, Department of Anaesthesia, Smt. BK Shah Medical Institute and Research Centre, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Jayshri Desai, A/503, Sugamavenues, New Vikas Gruh Road, Mahalakshmi, Paldi, Ahmedabad, Gujarat, India.
E-mail: desai.jayshri@yahoo.com
Ebstein’s anomaly is considered to be one of the rare congenital heart conditions which occur due to abnormal development of tricuspid valve and atrialisation of right ventricle and could be associated with either Atrial Septal Defect (ASD) or Patent foramen ovale through which shunting occurs. It might be associated with other cardiac malformations and rhythm disturbances. In such a patient, clinical presentation varies from congestive cardiac failure in childhood to incidental diagnosis in adulthood. If such a patient comes for surgery, it will be a challenging job for anaesthesiologist. Various cases have been reported of successful management either under general anaesthesia or epidural anaesthesia. In order to avoid complications of general anaesthesia, in a case report of 40-year-old female to provide some knowledge and information on the use of subarachnoid block in the case of Ebstein’s Anomaly posted for total abdominal hysterectomy.
Anesthetic management, Congenital anomaly, Congenital heart disease, Spinal anaesthesia
Case Report
A 40-year-old female, admitted to presented to the pre-anaesthetic clinic with chief complaints of irregular heavy bleeding per vagina, soakage of more than three pads per day, lasting for 10 to 12 days, associated with pain in abdomen from past eight months and was diagnosed with Abnormal Uterine Bleeding (AUB) and posted for total abdominal hysterectomy.
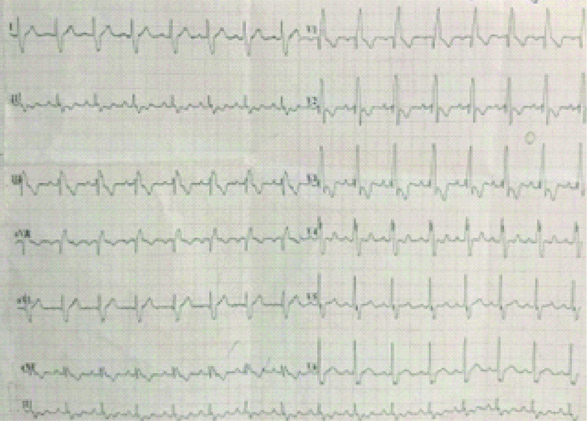
The patient also complaint of bilateral pitting oedema and breathlessness (New York Heart Association grade II). Not associated with chest pain, palpitations or recurrent chest infections. Electro cardiography shows right bundle branch block pattern, fragmented QRS complex and T wave inversions as shown in [Table/Fig-1]. After 2D Echocardiography and cardiac evaluation, she was diagnosed with Ebstein’s anomaly. She was started on tablet Spironolactone 40 mg OD since 3 days.
Right bundle branch block pattern, fragmented QRS complex and T wave inversions.
On examination, pulse rate was 100 beats per minute, regular, with normal volume, and character, with no radio-radial, or radio-femoral delay. Blood Pressure was 120/80 mmHg measured in right arm supine position. Respiratory Rate was 24 cycles per minute.
The Cardiovascular examination revealed systolic murmur at the tricuspid area. Chest X-ray showed Cardiomegaly with enlargement of right atrium, with prominent pulmonary artery, and Cardiothoracic ratio of 63% as shown in [Table/Fig-2]. A 2D ECHO revealed septal tricuspid leaflet apically displaced (>3.5 cm) with a severely dilated right atrium. The septal tricuspid leaflet showed limited mobility. Anterior tricuspid leaflet was elongated and redundant predominantly a sign of Ebstein’s anomaly. ASD Ostium Secundum (2 cm) with left to right shunt, mild valvular pulmonary stenosis, mild Tricuspid Regurgitation (TR), mild Pulmonary Artery Hypertension (PAH) were seen with Left ventricular ejection fraction of 40%. All other routine investigations were within normal limits.
Cardiomegaly with enlargement of right atrium, with prominent pulmonary artery, cardiothoracic ratio 63% (normal range 42%-50%).

Patient was kept nil per oral for 8 hours before surgery. After taking informed, written consent under American Society of Anaesthesiologists (ASA) grade III, Patient was shifted to operating room. An 18-gauge intravenous line was secured, preloaded with colloid solution slowly, multipara monitors attached and baseline vitals were recorded. The patient was premedicated with Injection Ondansetron 0.1 mg/kg intravenously. All measures to resuscitate the patient were kept ready and successful Subarachnoid block given in sitting position under all aseptic and antiseptic precautions between L3-L4 intervertebral space with 25-gauge Quincke’s spinal needle, 0.5% 3 mL hyperbaric bupivacaine with 0.5 mL fentanyl (total 3.5 mL) was given. There was good sensory and motor blockade till T8 level. The patient was haemodynamically stable, without hypotension, rhythm disturbances or any other complication throughout the procedure and in postoperative period.
Discussion
Ebstein’s Anomaly is a rare congenital heart disease with an incidence of 1 in 100,000 in general population. It was first described by Wilhelm Ebstein in 1866 which occurs due to incomplete delamination of embryonic tricuspid valve. This results in an atypically displaced valve tissue leading to congenital tricuspid insufficiency [1]. In patients with Ebstein’s anomaly anaesthetic management chosen, should be based on the cardiac status, type of surgery, site of surgery and also the duration of surgery [1].
Ebstein’s anomaly includes dysplastic abnormalities of the Tricuspid valve leaflets resulting in TR and sometimes stenosis. The right ventricle contractility is compromised as there is atrialisation of ventricle (wherein part of the right ventricle effectively forms part of atrium) due to downward displacement and elongation of septal and anterior cusp [1,2,3].
Patients can have a variety of symptoms related to the anatomical abnormalities of Ebstein anomaly and their haemodynamic effects or associated structural and conduction system disease. Cyanosis is fairly common and frequently due to right-to-left shunt at the atrial level and/or severe heart failure. It is transient in neonatal life, with recurrence in adult life; it may appear for the first time in adult life. The transient appearance or worsening of cyanosis in adult life is due to paroxysmal arrhythmias; once apparent, the cyanosis progressively worsens. Fatigue and dyspnea are due to poor cardiac output secondary to right ventricular failure, PAH and decreased left ventricular ejection fraction. Palpitations and sudden cardiac death may occur due to paroxysmal Supraventricular Tachycardia (SVT) or Wolff-Parkinson-White (WPW) syndrome in as many as one third of patients [1,2-4]. Fatal ventricular arrhythmias may also occur due to the presence of accessory pathways. Symptoms of right heart failure include ankle oedema and ascites. Other less common presenting symptoms includes Brain abscess due to right-to-left shunt, Bacterial endocarditis, Paradoxical embolism, stroke, and transient ischaemic attacks [3,5].
Present patient was acyanotic, with left to right shunt via ASD. She had cardiomegaly, mild PAH, mild TR, mild PS, with EF 40%. She had no additional serious conditions like WPW syndrome or cardiac failure. Aim in the present case was to maintain sinus rhythm, heart rate, preload, contractility, prevent rise in pulmonary vascular resistance, and maintain systemic vascular resistance. General anaesthesia causes impairment of myocardial function due to inhalational anaesthetics. It may necessitate the use of additional induction agent due to prolonged accumulation within the enlarged right atrium. The stress response which may occur due to laryngoscopy and intubation may lead to worsening of the condition. General anaesthesia may also cause increased catecholamine levels and an increased intrathoracic pressure which further increases intracardiac blood shunting [1,3,4]. Thus, subarachnoid block was chosen over general anaesthesia. Feared drawback with use of spinal anaesthesia is occurrence of sympathetic blockade induced precipitous hypotension, which may lead to right to left shunt and arrhythmias [1,4]. Thus, adequate preloading with colloids is of utmost importance and also appropriate ionotropic support to be kept available for emergency purposes. Paradoxical emboli which can be life threatening must be prevented by avoiding air bubbles in the peripheral venous lines. Reports of subarachnoid block being used in patients with Ebstein’s anomaly are scarce which made me choose this as topic of discussion [3].
Conclusion(s)
In present patient of Ebstein’s disease posted for total abdominal hysterectomy under subarachnoid blockade with injection bupivacaine and injection fentanyl provides good haemodynamic stability without any other cardiac complications and also provides effective postoperative analgesia and faster recovery.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 30, 2020
Manual Googling: Nov 13, 2020
iThenticate Software: Dec 24, 2020 (6%)
[1]. Usha Devi R, Vasantha Kumar KR, Vasundhara VM, Prabhu A, Subarachnoid block in a patient with Ebstein’s AnomalyJ Evolution Med Dent Sci 2015 4(82):14377-83.10.14260/jemds/2015/2045 [Google Scholar] [CrossRef]
[2]. Churlinov K, Anaesthesia for cesarean section baby delivery in parturient with Ebstein’s AnomalyEC Anaesthesia 2015 2(4):187-94. [Google Scholar]
[3]. Chaterjee S, Sengupta I, Mandal R, Sarkar R, Chakraborty PS, Anaesthetic management of Caesarean section in a patient with Ebstein’s anomalyIndian J Anaesth 2008 52(3):321-23. [Google Scholar]
[4]. Singh VK, Ratan R, Anaesthetic management of a patient with restrictive cardiomyopathy and ebstein anomaly for femoral hernia repairKarnataka Anaesth J 2015 1:196-98.10.4103/2394-6954.180654 [Google Scholar] [CrossRef]
[5]. Ganesh M, Krishnamurthy D, Talikoti AT, Abhishek KM, A rare case of Ebstein’s anomaly scheduled for elective caesarean SectionJ Clin Biomed Sci 2018 8(2):64-67. [Google Scholar]