Bone Mineral Status in Sub-clinical Hypothyroidism: A Case-control Study
M Vasanthan1, VM Vinodhini2
1 Assistant Professor, Department of Biochemistry, SRM Medical College Hospital and Research Centre, Faculty of Medicine and Health Sciences, SRM Institute of Science and Technology, Chennai, Tamil Nadu, India.
2 Professor and Head, Department of Biochemistry, SRM Medical College Hospital and Research Centre, SRM Institute of Science and Technology, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. M Vasanthan, Assistant Professor, Department of Biochemistry, SRM Medical College Hospital and Research Centre, Faculty of Medicine and Health Sciences, SRM Institute of Science and Technology, SRM Nagar, Kattankulathur, Kanchip, Chennai-603203, Tamil Nadu, India.
E-mail: vasanthm1@srmist.edu.in
Introduction
Hypothyroidism is the most common thyroid disorder which results in various metabolic disturbances. The disturbance in the bone minerals, calcium and phosphorus contribute to the most common imbalance. This is commonly overlooked in sub-clinical hypothyroidism, based on the absence of symptoms in patients related to thyroid hormone imbalance. The diagnosis of sub-clinical hypothyroidism is generally incidental and is based on the Thyroid Stimulating Hormone (TSH) level. The concentration of the circulating thyroid hormones, T3 (Triiodothyronine) and T4 (Thyroxine) are not altered in this condition.
Aim
To study the Ca/P ratio, an early indicator of osteoporotic marker among the patients with hypothyroidism.
Materials and Methods
The present study was designed as a case-control study and involved 35 controls with normal thyroid function and 35 subjects with sub-clinical hypothyroidism, of age group 20-45 years. The serum samples were analysed for calcium and phosphorus by their respective methods. The samples were analysed on the same day to maintain the stability of the parameters. Calcium/Phosphorus ratio (Ca/P) was calculated.
Results
Serum Calcium was found to be less (8.33±0.30) and serum phosphorus was more (6.61±0.88) in sub-clinical hypothyroidism when compared to control group. Therefore, a reversal of Ca/P ratio was (1.26±0.34) was noted.
Conclusion
This study underlines the necessity for patients with sub-clinical hypothyroidism to be monitored for bone mineral status to avoid complications in bone health.
Calcium, Calcium/Phosphorus ratio, Phosphorus
Introduction
Thyroid hormones T3 and T4 play a vital role in various metabolic activities, whose synthesis is regulated by TSH this in-turn is controlled by the Thyrotropin Releasing Hormone (TRH) of the hypothalamus. The condition when these thyroid hormones are circulated less in concentration in the blood than normal, the condition is termed as Hypothyroidism. The decrease in the concentration of thyroid hormones leads to an increase in the TSH. However, the symptoms of hypothyroidism appear only after the TSH exceeds 10 mIU/L [1]. Around 42 million of the Indian population is suffering from thyroid hormone imbalance, a study says, out of which hypothyroidism is more in number [2]. The frequency of hypothyroidism rises with the age and is found to be high among the women [3]. In 2015, among the South Indian population, hypothyroidism prevails itself with a prevalence of 11% according to a study conducted by Velayutham K et al., [4]. In sub-clinical hypothyroidism TSH level is elevated to some extent whereas T3 and T4 are within their normal ranges in serum [5].
Calcium and phosphorus imbalance are the most common metabolic disturbances seen in thyroid dysfunction [6]. As an important factor in causing secondary osteoporosis, thyrotoxicosis is more focused by the clinicians whereas hypothyroidism has comparatively a less focus [7]. A study conducted by Kavitha MM et al., also shows hypocalcaemia and hyperphosphatemia in hypothyroidism [8]. Decreased T3 and T4 leads to hypocalcaemia, which in-turn triggers overproduction of calcitonin. Calcitonin is responsible for the reabsorption of phosphate in tubules, leading to hyperphosphatemia. The disturbance in calcium and phosphorus levels in blood affects the bone metabolism. There is a decreased bone turnover in hypothyroidism leading to osteoporosis. This in-turn makes the individuals more prone to fracture especially in the older ages, when left untreated.
To estimate serum calcium and phosphorus in sub-clinical hypothyroidism as study group, and to compare the parameters and their ratio with control group with normal thyroid function, thereby to understand the influence of thyroid hormone in bone health, the need to screen the minerals and to treat the patients with sub-clinical hypothyroidism effectively.
Materials and Methods
The present study was a case-control study which included 35 subjects between 20-45 years of age attending Out-Patient Departments of various clinical specialties and incidentally diagnosed sub-clinical hypothyroidism as Group B, based on the thyroid hormone profile. Approval was obtained from the Institutional Ethical Committee with approval number (1243/IEC/2017). The study involved human participants in accordance to the ethical standards of the Institution where the study was conducted. The sample size was calculated based on the study by Roopa M and Gladys S [9]:
{2×(α+β)2[(S1)2+(S2)2]}÷[(M1-M2)2](α-95% Confidence level, β-90% Confidence level, S1,2-Standard Deviation1,2, M1,2-Mean1,2).
Group B (study group) included 23 women and 12 men whereas Group A (control group) included 18 men and 17 women with normal thyroid function. Patients with clinical conditions and those on medications that might affect serum calcium and phosphorus concentrations in serum were excluded from the study. Serum samples from the study group and the control group were drawn after getting informed and written consent, under strict aseptic conditions in the fasting state. The collected samples of both the groups (A and B) were analysed for FT4 (Free thyroxine), TSH, calcium and phosphorus. The hormones were analysed in fully automated hormone analyser Vitros ECi and the biochemical parameters were analysed in fully automated Biochemistry analyser-Beckman Coulter AU 480 by their respective methods [Table/Fig-1] [10]. Ca/P ratio was then calculated.
Methods of estimation [10].
| Parameter | Method |
|---|
| TSH (mIU/L) | CLIA |
| FT4 (ng/dL) | CLIA |
| Calcium (mg/dL) | Arsenazo |
| Phosphorus (mg/dL) | UV Molybdate |
Statistical Analysis
Statistical analysis by Independent t-test and Pearson’s correlation were performed to determine the relationship between risk variables. The p-value <0.05 was considered statistically significant and p-value <0.01 was considered as highly significant.
Results
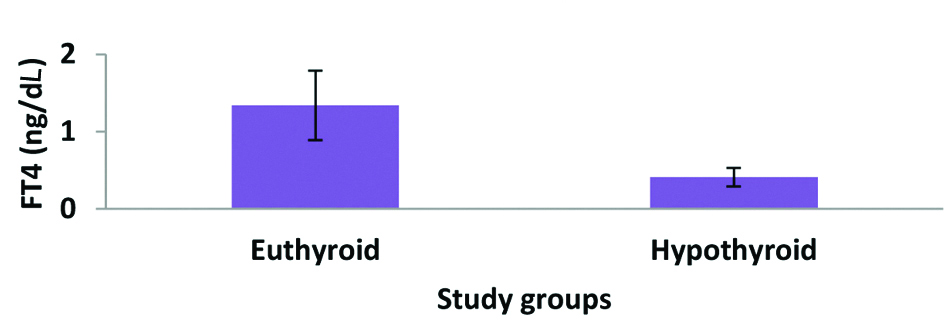
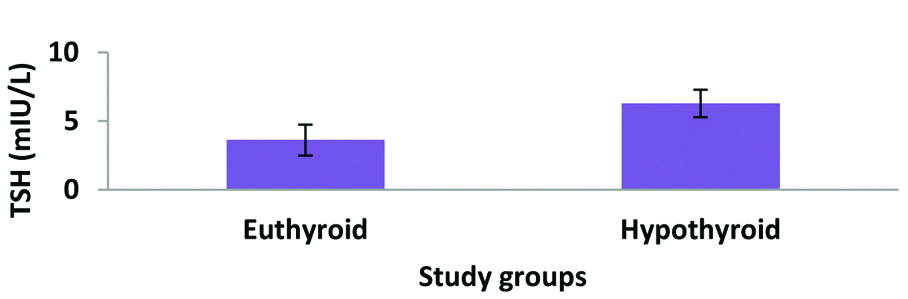
It was observed that the means of the parameters, FT4 and TSH were 1.34±0.45 ng/dL and 3.61±1.13 mIU/L respectively in Group A, whereas they were 0.41±0.12 ng/dL and 6.28±1.01 mIU/L among Group B [Table/Fig-2,3]. The TSH levels in Group B is indicative of sub-clinical hypothyroidism.
Concentration of FT4 in Group A and Group B.
Concentration of TSH in Group A and Group B.
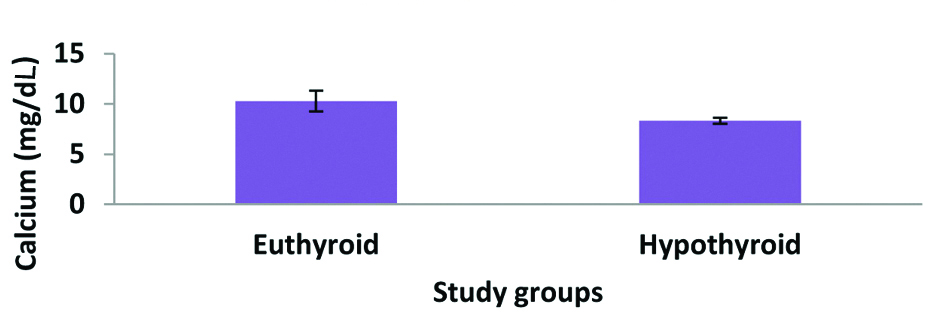
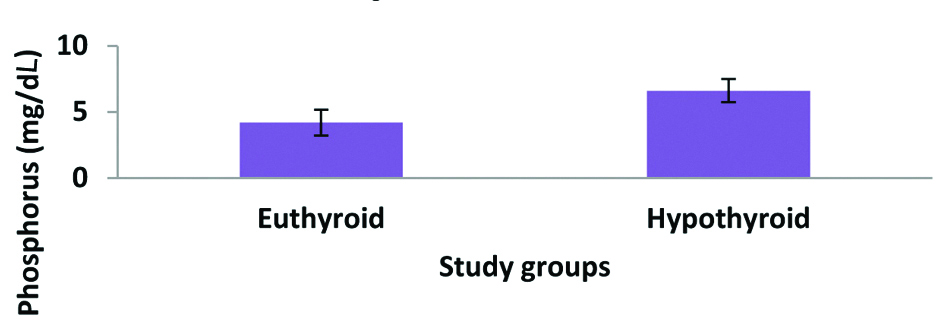
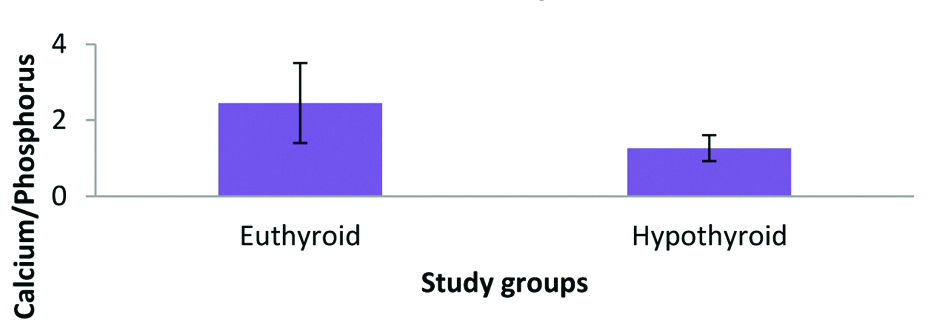
The bone mineral status was assessed with the help of calcium and phosphorus among the participants of both the groups. Mean Calcium was 10.28±1.03 mg/dL and 8.33±0.30 mg/dL among the controls and the subjects respectively. This indicates a decreased calcium level in patients with sub-clinical hypothyroidism [Table/Fig-4]. The mean phosphorus was 4.19±0.98 mg/dL in controls with normal thyroid function and 6.61±0.88 mg/dL in sub-clinical hypothyroidism [Table/Fig-5]. From the above mineral parameters, Ca/P was calculated and was derived as 2.45±1.05 in controls and 1.26±0.34 in subjects [Table/Fig-6]. This clearly indicates a reversal of the Ca/P among the patients with sub-clinical hypothyroidism [Table/Fig-7]. The normal Ca/P was obtained from a study as 2.09. Individuals with Ca/P <2.09 were more prone for osteoporosis and individuals with Ca/P >2.09 were normal [11].
Concentration of Calcium in Group A and Group B.
Concentration of Phosphorus in Group A and Group B.
Calcium/Phosphorus in Group A and Group B.
Parameters among Groups A and B.
| Parameters | Group A | Group B |
|---|
| Mean | SD | Mean | SD |
|---|
| FT4 (ng/dL) | 1.34 | 0.45 | 0.41 | 0.12 |
| TSH (mIU/L) | 3.61 | 1.13 | 6.28 | 1.01 |
| Calcium (mg/dL) | 10.28 | 1.03 | 8.33 | 0.30 |
| Phosphorus (mg/dL) | 4.19 | 0.98 | 6.61 | 0.88 |
| Ca/P | 2.45 | 1.05 | 1.26 | 0.34 |
SD: Standard deviation; FT4: Free thyroxine; TSH: Thyroid stimulating hormone; Ca/P: Calcium/Phosphorus ratio
The results obtained clearly showed decreased concentrations of the parameters serum calcium, phosphorus and Ca/P in Group B (Hypothyroid patients) when compared to the healthy controls, with high significance of p<0.001 for calcium and phosphorus, and a high significance for Ca/P as well [Table/Fig-8].
Comparison of the variables between the groups A and B.
| Dependent variable | Group | Group | Mean difference (A-B) | Std. Error | Significance p* | 95% Confidence interval |
|---|
| Lower bound | Upper bound |
|---|
| FT4 | A | B | -0.930 | 0.079 | <0.001 | -1.09 | -0.77 |
| TSH | A | B | 2.670 | 0.256 | <0.001 | 2.16 | 3.18 |
| Calcium | A | B | -1.950 | 0.181 | <0.001 | -2.31 | -1.59 |
| Phosphorus | A | B | 2.420 | 0.223 | <0.001 | 1.98 | 2.86 |
| Ca/P | A | B | -1.190 | 0.187 | <0.001 | -1.56 | -0.82 |
*Student’s t test *p<0.001; highly significant (significance of difference between sub-clinical hypothyroid cases and normal controls)
Discussion
Reduced levels of FT3 and FT4 are termed as hypothyroidism and it leads to a positive feedback with increased TSH levels through the hypothalamic-pituitary-thyroid axis. Studies show a decrease in calcium and a decrease in phosphorus among hypothyroid patients when compared to those with normal thyroid status.
According to a study, hypocalcaemia and decreased bone turnover were noted in hypothyroidism, in compliance with the current study [12]. Both the mean calcium and phosphorous levels were lower in hypothyroidism with a higher significance compared to controls a study says [13]. Whereas, the present study showed an increase in phosphorus. Another study showed normal calcium levels in hypothyroid patients [14]. Contrastingly, the present study there was decreased calcium levels.
An increase in the risk of fracture among patients with hypothyroidism was reported [15]. There were studies with evidences supporting the existence of bone disorders with thyroid disorders among different age groups [16,17]. According to a study conducted on 1290 subjects which included subjects from most states of India, bone mineral density is not affected by TSH when compared to the euthyroids [18]. In a large cohort study conducted among Korean population during 2011-2016 no association was found between BMD and sub-clinical hypothyroidism [19]. Another study showed an association between femoral neck bone loss and sub-clinical hyperthyroidism [20]. Bone health was not impaired among children with long-term sub-clinical hypothyroidism, reports a study [21].
The studies which contrasted with the presently conducted study implicate us the importance of conducting more elaborate studies in this regard.
Limitation(s)
The study population shall be enlarged as present study had relatively less sample size. Present study should have considered the dietary habit of the subjects. The study shall have included bone mineral density to screen for osteoporosis.
Conclusion(s)
From the study it is concluded that, disturbances in thyroid hormone, even in sub-clinical stages, are responsible for changes in bone mineral health by altering calcium and phosphorus levels in serum and thereby, leading to the bone complications like osteoporosis and fracture, affecting the normal life of the diseased. The condition can be reversed if the minerals were estimated and a proper correction for thyroid hormones and the minerals were attained in the early stages.
SD: Standard deviation; FT4: Free thyroxine; TSH: Thyroid stimulating hormone; Ca/P: Calcium/Phosphorus ratio
*Student’s t test *p<0.001; highly significant (significance of difference between sub-clinical hypothyroid cases and normal controls)
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 01, 2020
Manual Googling: Nov 18, 2020
iThenticate Software: Jan 21, 2021 (10%)
[1]. Fatourechi V, Subclinical hypothyroidism: An update for primary care physiciansMayo Clin Proc 2009 84(1):65-71.10.4065/84.1.6519121255 [Google Scholar] [CrossRef] [PubMed]
[2]. Kochupillai N, Clinical endocrinology in IndiaCurrent science 2000 79(8):1061-67. [Google Scholar]
[3]. Vanderpump MPJ, Epidemiology of thyroid diseaseBritish Medical Journal 2011 99(1):39-51.10.1093/bmb/ldr03021893493 [Google Scholar] [CrossRef] [PubMed]
[4]. Velayutham K, Selvan SS, Unnikrishnan AG, Prevalence of thyroid dysfunction among young females in a South Indian populationIndian J Endocrinol Metab 2015 19(6):781-84.10.4103/2230-8210.16754626693428 [Google Scholar] [CrossRef] [PubMed]
[5]. Rugge B, Balshem H, Sehgal R, Relevo R, Gorman P, Helfand M, Screening and treatment of subclinical hypothyroidism or hyperthyroidism [Internet] 2011 Rockville (MD)Agency for Healthcare Research and Quality (US)Report No.: 11(12)-EHC033-EF [Google Scholar]
[6]. Sato K, Han DC, Fujii Y, Tsushima T, Shizume K, Thyroid hormone stimulates alkaline phosphatase activity in cultured rat osteoblastic cells (ROS 17/2.8) through 3,5,3’-triiodo-L-thyronine nuclear receptorsEndocrinology 1987 120(5):1873-81.10.1210/endo-120-5-18733569118 [Google Scholar] [CrossRef] [PubMed]
[7]. Dhanwal DK, Thyroid disorders and bone mineral metabolismIndian J Endocrinol Metab 2011 15(Suppl 2):S107-12.10.4103/2230-8210.8333921966645 [Google Scholar] [CrossRef] [PubMed]
[8]. Kavitha MM, Pujar S, Hiremath CS, Prasad S, Mahanthesh Evaluation of serum electrolytes in hypothyroid patientsMed Pulse-International Medical Journal 2014 1(8):393-95. [Google Scholar]
[9]. Roopa M, Gladys S, Changes in electrolyte and lipid profile in hypothyroidismInternational Journal of Life Science and Pharma Research 2012 2(3):L185-94. [Google Scholar]
[10]. Goswami K, Mookherjee S, Mazumdar I, Calibration verification for olympus au480 and meril autoquant aq 400i automatic biochemistry auto analyser using seven analytesEuropean Journal of Biomedical and Pharmaceutical Sciences 2017 4(11):682-86. [Google Scholar]
[11]. Madeo B, Kara E, Cioni K, Vezzani S, Trenti T, Santi D, Serum Calcium to Phosphorous (Ca/P) ratio is a simple, inexpensive, and accurate tool in the diagnosis of primary hyperparathyroidismJBMR Plus 2017 2(2):109-17.10.1002/jbm4.1001930283895 [Google Scholar] [CrossRef] [PubMed]
[12]. Mane AY, Bhagwat VR, Assessment of some biochemical markers of bone turnover in thyroid dysfunction stateIJPBS 2012 3(3):B126-33. [Google Scholar]
[13]. Shivaleela MB, Poornima RT, Jayaprakash MDS, Serum calcium and phosphorus levels in thyroid dysfunctionIJFALS 2012 2(2):179-83. [Google Scholar]
[14]. Begic-Karup S, Wagner B, Raber W, Schneider B, Hamwi A, Waldhäusl W, Serum calcium in thyroid diseaseWien Klin Wochenschr 2001 113(1-2):65-68. [Google Scholar]
[15]. Vestergaard P, Mosekilde L, Fractures in patients with hyperthyroidism and hypothyroidism: A nationwide follow-up study in 16,249 patientsThyroid 2002 12:411-19.10.1089/10507250276004350312097203 [Google Scholar] [CrossRef] [PubMed]
[16]. Grimnes G, Emaus N, Joakimsen RM, Figenschau Y, Jorde R, The relationship between serum TSH and bone mineral density in men and postmenopausal women: The Troms studyThyroid 2008 18:1147-55.10.1089/thy.2008.015818925834 [Google Scholar] [CrossRef] [PubMed]
[17]. Demartini Ade A, Kulak CA, Borba VC, Cat MNL, Dondoni RS, Sandrini R, Bone mineral density of children and adolescents with congenital hypothyroidismArq Bras Endocrinol Metabol 2007 51:1084-92.10.1590/S0004-2730200700070001018157383 [Google Scholar] [CrossRef] [PubMed]
[18]. Marwaha RK, Garg MK, Tandon N, Kanwar R, Narang A, Sastry A, Thyroid function and bone mineral density among Indian subjectsIndian J Endocrinol Metab 2012 16(4):575-79.10.4103/2230-8210.9801422837919 [Google Scholar] [CrossRef] [PubMed]
[19]. Lee K, Lim S, Park H, Woo HY, Chang Y, Sung E, Subclinical thyroid dysfunction, bone mineral density, and osteoporosis in a middle-aged Korean populationOsteoporos Int 2020 31(3):547-55.10.1007/s00198-019-05205-131720711 [Google Scholar] [CrossRef] [PubMed]
[20]. Segna D, Bauer DC, Feller M, Schneider C, Fink HA, Aubert CE, Association between subclinical thyroid dysfunction and change in bone mineral density in prospective cohortsJ Intern Med 2018 283(1):56-72.10.1111/joim.1268829034571 [Google Scholar] [CrossRef] [PubMed]
[21]. Di Mase R, Cerbone M, Improda N, Esposito A, Capalbo D, Mainolfi C, Bone health in children with long-term idiopathic subclinical hypothyroidismItal J Pediatr 2012 38:5610.1186/1824-7288-38-5623088718 [Google Scholar] [CrossRef] [PubMed]