Repair of Preduodenal Portal Vein Injury with Polytetrafluoroethylene Graft with Midgut Rotation and Left Sided Inferior Vena Cava
Zuber Ansari1, Tuhin Subhra Mandal2, Koustav Jana3, Avik Sarkar4
1 Post Doctoral Trainee, Department of Surgical Gastroenterology, School of Digestive and Liver Disease Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
2 Assistant Professor, Department of Surgical Gastroenterology, School of Digestive and Liver Disease Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
3 Senior Resident, Department of Surgical Gastroenterology, School of Digestive and Liver Disease Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
4 Assistant Professor, Department of GI Radiology, School of Digestive and Liver Disease Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Tuhin Subhra Mandal, 244, AJC Bose Road, Department of Surgical Gastroenterology, School of Digestive and Liver Disease, Institute of Postgraduate Medical Education and Research, Kolkata, West Bengal, India.
E-mail: drtuhin.subhra@gmail.com
Preduodenal Portal Vein (PDPV) is a rare congenital anomaly. The presence of PDPV carries the risk of injury to Portal Vein (PV) during operations involving biliary duct, duodenum and pancreas. This report is about a 50-year-old female patient with PDPV associated with midgut malrotation and left sided Inferior Vena Cava (IVC). The patient was operated for Recurrent Pyogenic Cholangitis (RPC) and associated biliary stones. The patient sustained iatrogenic injury to PV during surgery which was subsequently repaired with Polytetrafluoroethylene (PTFE) graft doppler showed patent graft at three months of follow-up. This report highlights the fact that pre-existing inflammatory conditions of bile duct and hepatoduodenal ligament further increase the risk of injury to PDPV during surgery.
Bile duct, Cholangitis, Computed tomography, Duodenum, Pancreas
Case Report
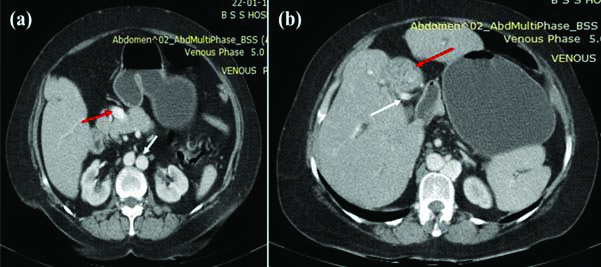
A 50-year-old female patient presented with complaints of recurrent fever and pain in upper abdomen since past three months. Patient had history of open cholecystectomy for symptomatic cholelithiasis, 12 years ago. Physical examination was unremarkable. Her blood investigations and 2D-Echocardiography were normal. Ultrasonography and Magnetic Resonance cholangiography revealed multiple stones in Common Bile Duct (CBD) and bilateral second order bile ducts. The patient was thus diagnosed as a case of RPC based on medical history and imaging. Diagnosis of Choledochal cyst was excluded by confirming the absence of dilated bile duct on previous imaging records. Contrast-Enhanced Computed Tomography (CECT) of the abdomen revealed PDPV coursing anterior to pancreas and right to lateral border of dilated and stone filled Common Hepatic Duct (CHD) [Table/Fig-1a,b]. IVC was coursing left to abdominal Aorta [Table/Fig-1a, white arrow]. Midgut malrotation was present. Patient was planned for CBD exploration with removal of intra-hepatic ductal stones and Roux-En-Y Hepatico-jejunostomy (RYHJ).
a) CECT scan showing portal vein (red arrow) coursing anterior to pancreas, IVC (white arrow) coursing left to aorta. b) CECT scan showing dilated CHD filled with calculi (red arrow), portal vein coursing right lateral side to CHD (white arrow).
IVC: Inferior venacava; CHD: Common hepatic duct; CECT: Contrast-Enhanced Computed Tomography
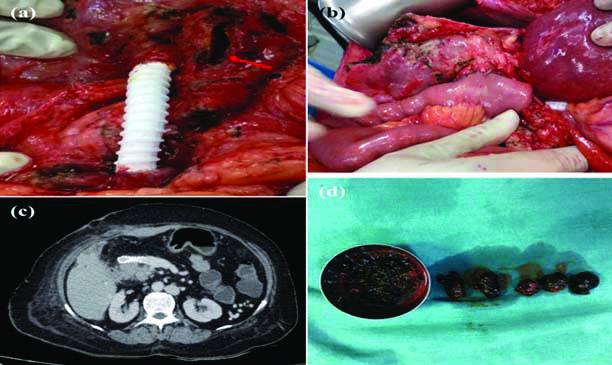
At surgery, adhesions were present around porta hepatis due to previous attacks of cholangitis. Multiple stones were present in dilated CBD and secondary biliary radicles. Bile duct wall was thickened [Table/Fig-2a, red arrow]. PV was densely adhered to side of wall CHD. Hard intraductal stones in CHD were impinging on PV. Complete transactional injury to PV occurred on giving traction to bile duct during dissection. Immediate vascular control of both transacted end was achieved by vascular clamps. Primary repair of PV was not possible as both ends were wide apart; therefore, PV was repaired by PTFE graft of 6 cm in length and 8mm in diameter in end to end anastomosis with Prolene 5.0 [Table/Fig-2a]. Biliary reconstruction was done with RYHJ after complete stone clearance [Table/Fig-2b]. Ladd’s procedure was added for malrotation of intestine. Total operative time was 380 minutes and total intraoperative blood loss was 400 mL. Patient had an uneventful recovery except wound infection which was managed by regular dressing and secondary suturing. Postoperative CECT scan showed intact graft lying anterior to pancreas [Table/Fig-2c]. Doppler study on postoperative days 1,4 and 8 showed patent graft. Patient was not given prophylactic anticoagulants or antiplatelets after surgery. Doppler showed patent graft at three months. Patient was asymptomatic with normal liver function test after five months of follow-up.
a) PTFE graft after reconstruction coursing anterior to duodenum. Dilated cut end of Common Hepatic Duct (CHD) showing inflammatory thickened wall (red arrow), b) biliary reconstruction by RYHJ, c) CECT scan showing intact graft lying anterior to pancreas, d) multiple stones retrieved from CHD and intrahepatic ducts.
PTFE: Poly tetrafluoroethylene; RYHJ: Roux-En-Y Hepatico-jejunostomy
Discussion
PDPV anomaly was first reported by Knight in 1921 [1]. It usually presents in paediatric patients with intestinal obstruction due to duodenal compression. In adults, it is often asymptomatic and incidental finding during intra-bdominal surgery for unrelated condition [2]. The anomalous vein carries a risk of injury during pancreatic-biliary surgery which can result in massive haemorrhage with high morbidity and mortality. It is even rarer in adults. Associated intestinal and cardiac anomalies such as polysplenia, asplenia, biliary atresia, intestinal malrotation, situs inversus are frequent findings with PDPV [2]. No cardiac anomaly was identified in the patient, however, presence of left sided IVC with PDPV which was present had not been described to be associated with PDPV in previous literature. There is scarcity of literature on the repair of iatrogenic PDPV injury. This case report highlights the mechanism of iatrogenic PDPV injury and its subsequent repair with PTFE graft in a patient who underwent surgery for RPC. Many methods for reconstruction of PV injury have been described in literature including lateral venorrhaphy, primary end to end anastomosis, portocaval shunt, ligation of PV, autologous graft and prosthetic grafts. Reconstruction of PV with short segment loss can be done with end-to-end tension free anastomosis [3]. Reconstruction of longer segments requires graft which may be either autograft or prosthetic graft. In terms of size, autologous internal jugular vein is appropriate for reconstruction [4]. In urgent scenario such as this, PTFE graft has many advantages over autologous vein graft including easily availability, perfect selection of diameter and length, easy handling, avoidance of complications related to autologous vein harvest, less operative time and less blood loss. Graft thrombosis and infection are major potential complications of PV repair [4-6].
Most studies refer only to a single case report rather than a series of patients with PV injury. However, the role of prosthetic graft in PV or hepatic vein repair is well established by vascular reconstruction results in pancreaticobiliary malignancies and liver transplant [4-7]. Excellent short-term and long-term patency rate of PTFE graft have been described in studies, ranging between 90%-100% [6]. However, there is lack of uniform algorithm of postoperative graft surveillance and use of prophylactic anti-coagulants or anti-platelets agents due to lack of randomised studies and their role in routine prophylaxis is controversial at present. However, studies have shown no additional risk of graft thrombosis without prophylactic anti-coagulants [6,8]. For postoperative follow-up in this patient, institutional protocol was followed based on which, serial three-monthly graft surveillance was done using doppler study for first year. This was followed by every six-monthly evaluation. Patients are put on therapeutic oral anticoagulants only in presence of PV thrombosis on imaging. Routine prophylactic anticoagulant or antiplatelet agent is not recommended, in PV repair with PTFE graft.
PTFE has shown to be resistant to infection compared to other graft material [9]. Studies have examined vascular resection in abdominal surgery and shown good outcome with PTFE graft even in the presence of abdominal sepsis [6,10,11]. Two separate studies found no case of graft infection in patients that underwent pancreatic resection, respectively [6,12]. PDVD increases the risk of iatrogenic injury to PV during biliary surgery [13]. Although, PDPV course and its relation to adjacent structures can easily be detected on CECT scan before surgery but risk of PDPV injury during surgery must be considered in all pancreatic-biliary surgeries even in the presence of preoperative identification of anomaly. In this case, multiple factors such as bile duct inflammation, presence of large stone burden [Table/Fig-2d] in dilated bile duct which was impinging on PV contributed to the injury to PDPV.
Conclusion(s)
Pre-existing inflammatory conditions of bile duct and other structures in hepatoduodenal ligament increase the risk of injury due to combination of distorted anatomy and distorted dissection planes. In such scenario, precise dissection in appropriate tissue planes and application of minimal traction is required. Facility and availability of instruments and graft material for vascular reconstruction and surgeon’s experience in vascular surgery should be considered before operating on such complex patients. PTFE graft is feasible option for PV repair in urgent situation.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 30, 2020
Manual Googling: Dec 15, 2020
iThenticate Software: Jan 20, 2021 (9%)
[1]. Knight HO, An anomalous portal vein with its surgical dangersAnnals of Surgery 1921 74(6):697-99.10.1097/00000658-192112000-0000417864564 [Google Scholar] [CrossRef] [PubMed]
[2]. Mordehai J, Cohen Z, Kurzbart E, Mares AJ, Preduodenal portal vein causing duodenal obstruction associated with situs inversus, intestinal malrotation, and polysplenia: A case reportJournal of Pediatric Surgery 2002 37(4):E510.1053/jpsu.2002.3164311912540 [Google Scholar] [CrossRef] [PubMed]
[3]. Fraga GP, Bansal V, Fortlage D, Coimbra R, A 20-year experience with portal and superior mesenteric venous injuries: Has anything changed?Eur J Vasc Endovasc Surg 2009 37(1):87-91.10.1016/j.ejvs.2008.09.01818993088 [Google Scholar] [CrossRef] [PubMed]
[4]. Stauffer JA, Dougherty MK, Kim GP, Nguyen JH, Interposition graft with polytetrafluoroethylene for mesenteric and portal vein reconstruction after pancreaticoduodenectomyBr J Surg 2009 96(3):247-52.10.1002/bjs.648319224515 [Google Scholar] [CrossRef] [PubMed]
[5]. Smoot RL, Christein JD, Farnell MB, Durability of portal venous reconstruction following resection during pancreaticoduodenectomyJ Gastrointest Surg 2006 10(10):1371-75.10.1016/j.gassur.2006.09.00117175456 [Google Scholar] [CrossRef] [PubMed]
[6]. Chu CK, Farnell MB, Nguyen JH, Stauffer JA, Kooby DA, Sclabas GM, Prosthetic graft reconstruction after portal vein resection in pancreaticoduodenectomy: A multicenter analysisJ Am Coll Surg 2010 211(3):316-24.10.1016/j.jamcollsurg.2010.04.00520800187 [Google Scholar] [CrossRef] [PubMed]
[7]. Lee SH, Na GH, Choi HJ, Kim DG, You YK, Impact of the reconstruction material on the patency of middle hepatic vein in living donor liver transplantation using the right liverTransplant Proc 2019 51(8):2745-49.10.1016/j.transproceed.2019.03.07531563244 [Google Scholar] [CrossRef] [PubMed]
[8]. Hazama K, Miura H, Shimada T, Okuda Y, Murashita T, Nishibe T, Relationship between fibril length and tissue ingrowth in the healing of expanded polytetrafluoroethylene graftsSurg Today 2004 34(8):685-89.10.1007/s00595-004-2774-915290399 [Google Scholar] [CrossRef] [PubMed]
[9]. Shell DH 4th, Croce MA, Cagiannos C, Jernigan TW, Edwards N, Fabian TC, Comparison of small-intestinal submucosa and expanded polytetrafluoroethylene as a vascular conduit in the presence of gram-positive contaminationAnn Surg 2005 241(6):995-1004.10.1097/01.sla.0000165186.79097.6c15912049 [Google Scholar] [CrossRef] [PubMed]
[10]. Bower TC, Nagorney DM, Cherry KJ Jr, Toomey BJ, Hallett JW, Panneton JM, Replacement of the inferior vena cava for malignancy: An updateJ Vasc Surg 2000 31(2):270-81.10.1016/S0741-5214(00)90158-7 [Google Scholar] [CrossRef]
[11]. Cho JS, Carr JA, Jacobsen G, Shepard AD, Nypaver TJ, Reddy DJ, Long-term outcome after mesenteric artery reconstruction: A 37-year experienceJ Vasc Surg 2002 35(3):453-60.10.1067/mva.2002.11859311877692 [Google Scholar] [CrossRef] [PubMed]
[12]. Müller SA, Hartel M, Mehrabi A, Welsch T, Martin DJ, Hinz U, Vascular resection in pancreatic cancer surgery: Survival determinantsJ Gastrointest Surg 2009 13(4):784-92.10.1007/s11605-008-0791-519137380 [Google Scholar] [CrossRef] [PubMed]
[13]. Bansal R, Dhillon KS, Kaushal G, Preduodenal portal vein: A recipe for disaster during laparoscopic cholecystectomyJournal of Minimal Access Surgery 2019 15(1):63-64.10.4103/jmas.JMAS_73_1829737323 [Google Scholar] [CrossRef] [PubMed]