Hypospadias is one of the most common congenital anomaly among males. It is a common condition occurring in 1:250 to 1:300 new born males [1]. Hypospadias repair aims at the creation of a cosmetically normal meatal opening near the tip with an adequate meatus. It gives the patient a satisfaction to urinate in standing position and good sexual function [2]. The ideal time to operate on such cases is in the early life as it has significant psychological impact on the urinary and sexual function in the adult life [3]. There is a general opinion about a significant difference in the tissue quality and vascular supply corresponding to the patient’s age and therefore the success of operating at an early age seems higher [1,4]. Success is also related to the number of surgeries the patient has undergone. Literature is available about the surgical results and long term follow-up assessment of hypospadias repair in the paediatric population, but there is lack of sufficient studies on comparative analysis and long term follow-up studies of similar repairs in the adolescent and adult age groups [3,4].
Hypospadias repair in the adolescent and adults can be of three varieties: the primary cases, the patients who have been operated earlier but now presented with late complications and the patients who have undergone multiple surgeries but in vain, referred to as the hypospadias cripples. The reported rates of complications in adult hypospadias undergoing first time repair ranges from 10-37% [5]. There are several studies reporting a higher complication rates in the adult hypospadias surgery. In one such notable study, Barbagli G et al., operated on 60 adult hypospadias patients and concluded that adults presenting with complications following childhood hypospadias repair are a difficult population to treat with high risk of failure [6,7]. Whereas others did not find any significant difference in terms of wound healing, infection and complications using the similar surgical techniques in the adult population [6,8].
The primary aim was to assess whether there is any difference in outcome of hypospadias surgeries among the adolescent and adult population. The secondary aim was to assess whether using a TV second layer barrier flap can prevent complications such as urethrocutaneous fistula among these patients.
Materials and Methods
This was a retrospective observational study of all the adolescent (12-18 years) and adult hypospadias surgeries done in a tertiary care hospital from January 2016 till July 2019.
This study followed all Institutional Ethical guidelines in place at the time when this work was done. It also followed Helsinki declaration (2013) while doing this study.
This study was a retrospective assessment of the outcome of operating on all the 17 adolescent (12-18 years) and 11 adult hypospadias cases using the routine surgeries done in this institute. In all these patients, TV second layer barrier flap was used as per the institute’s protocol. The data assessment was done based on the age group of presentation, presenting complaints, site of hypospadias, any history of previous surgery, development of any complications and recurrence.
Inclusion criteria: Patients aged >12 years with primary hypospadias or recurrence following previous surgery were included in this study.
Exclusion criteria: Patients who had bleeding diathesis or were found unfit to undergo surgery under anaesthesia were excluded from the study.
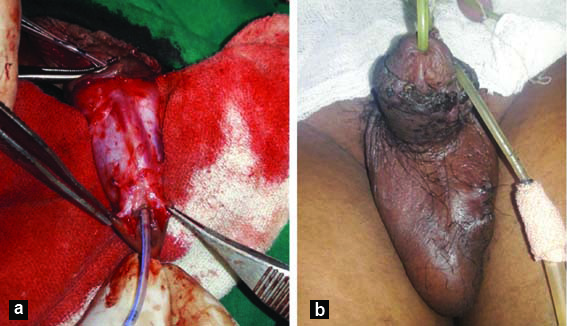
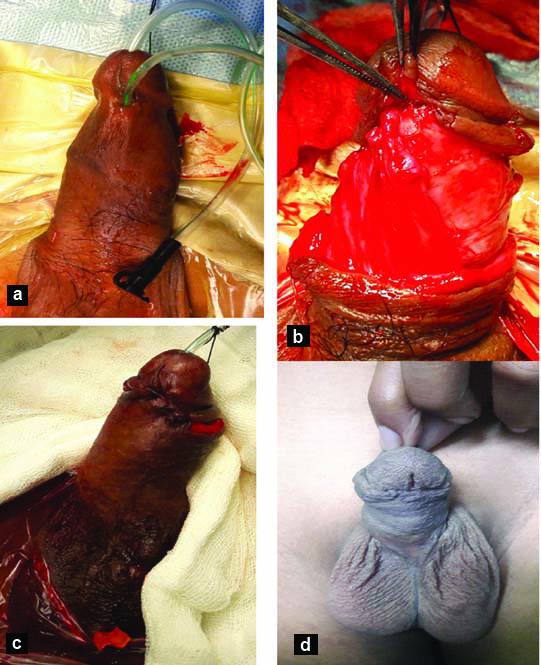
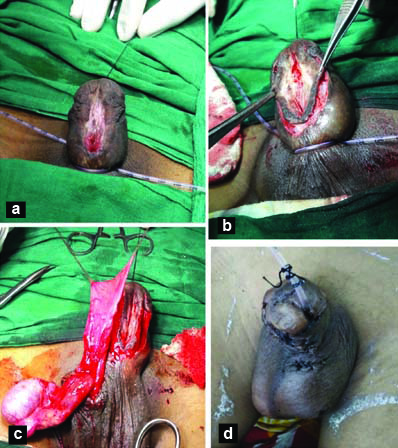
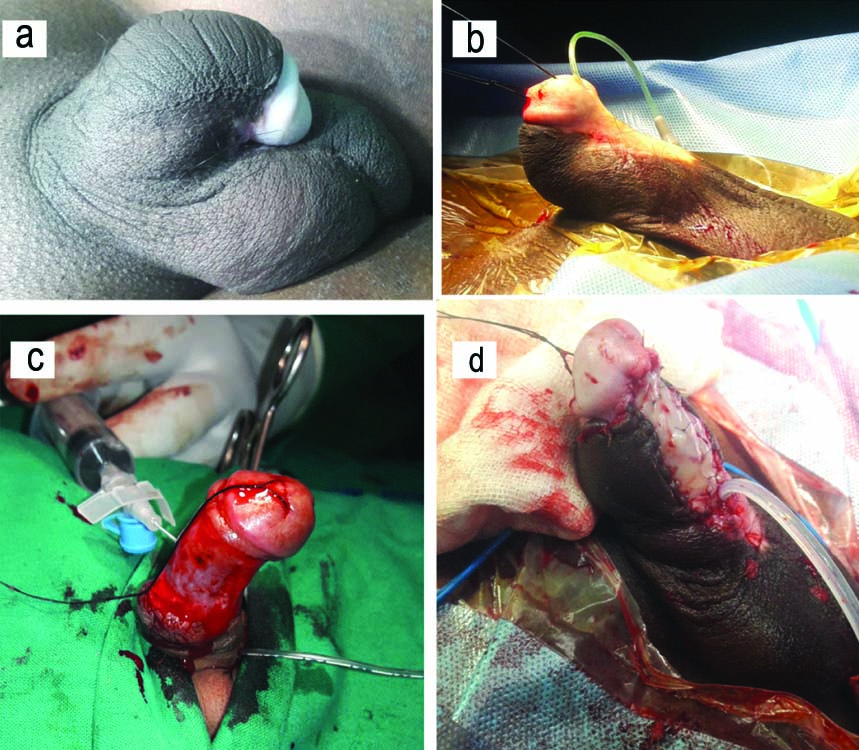
The choice of surgery was made based on the location and calibre of the meatus, previous surgery and appearance of the urethral plate. Routine procedures as per the hospital protocol such as Snodgrass technique (TIP-Tubularised incised plate) of repair was preferred for distal and mid-penile hypospadias without significant chordee [Table/Fig-1]. For proximal penile hypospadias or history of previously failed procedure or hypospadias cripple, staged repair with buccal or labial mucosa graft was preferred [Table/Fig-2,3]. In all cases, TV flap was used as interposition second layer [Table/Fig-2].
Distal primary hypospadias repair by the Snodgrass technique.
Failed proximal hypospadias repair in an adult patient using Snodgrass technique and Tunica Vaginalis (TV) interposition barrier flap.
Staged repair of a hypospadias cripple with multiple failed surgeries using buccal mucosal graft for neo-urethral plate creation in the first stage. Followed by tubularisation in the second stage. TV barrier flap was used in the second stage.
Surgery was done by the same primary surgeon utilising different teams. The patients were asked to follow-up for a minimum period of 12 months after the procedure. The aim was to look for the resolution of the symptoms of patient in terms of good urinary stream, cosmesis and development of any complications at the end of the follow-up period.
Statistical Analysis
For data analysis, relevant statistical methods were used. It included tables and columns. Fisher’s-exact test was used to find the association and calculate the p-value. The p-value <0.05 was considered to be statistically significant. SPSS 21.0 was used for data analysis.
Results
Twenty eight (28) patients were assessed, of which 17 patients were adolescents (12 to 18 years) and 11 were adult. Of these cases, 20 were primary and eight cases had been operated earlier (secondary) and now presented following failed surgery in the childhood.
The mean age of the adolescent population in this study was 14.6 years. (±1.66 years). The mean age of the adult population was 22.7 years (±3.51 years). Distribution of patients with respect to the location of the meatus is shown in [Table/Fig-4].
Distribution of patients with respect to the location of the urethral meatus.
| Location of the meatus | Adolescents (n) | Adults (n) | Number (n) |
|---|
| Distal penile | 12 | 6 | 18 |
| Proximal penile | 4 | 5 | 9 |
| Severe chordee without hypospadias | 1 | 0 | 1 |
| Total | 17 | 11 | 28 |
Distribution of hypospadias cases among the adolescent and adult population with respect to presentation is shown in [Table/Fig-5]. Majority of the adolescents were primary cases.
Distribution of hypospadias cases among the adolescent and adult population with respect to timing of presentation.
| Hypospadias cases | Adolescent (n) | Adult (n) | Total |
|---|
| Primary cases | 13 | 7 | 20 |
| Secondary cases | 4 | 4 | 8 |
| Total | 17 | 11 | 28 |
The most common presenting complaints among the adolescent population was narrow stream of urine (47%) and among the adults was dribbling of urine (45.4%). The presenting complaints among the hypospadias cases are shown in [Table/Fig-6].
Distribution of presenting complaints among the hypospadias patients.
| Location of meatus | Narrow stream n (%) | Dribbling of urine n (%) | Cosmetic n (%) | Total |
|---|
| Adolescent cases | 8 (47) | 5 (29.5) | 4 (23.5) | 17 |
| Adult cases | 2 (18.1) | 5 (45.4) | 4 (36.3) | 11 |
The details on the types of surgeries have been described in [Table/Fig-7,8,9 and 10]. The average follow-up period among the adolescent population was 13.7 months and among the adult population was 11.8 months. The common complications of the procedures were urethrocutaneous fistula, wound infection, haematoma and suture line dehiscence. In both the groups Urethrocutaneous fistula was the most common complication and therefore it was considered as the main complication of surgery affecting the final outcome. The comparative analysis of the recurrence/complications between the adolescent and adult population are shown in [Table/Fig-11].
Type of repair done in the distal penile hypospadias cases.
| Primary hypospadias (total 15) | a) In 14 of the cases Snodgrass/TIP was done [Table/Fig-1]b) In 1 case Snod graft (Patch of buccal/labial grafting) was done for narrow urethral plate [Table/Fig-8] |
| Secondary hypospadias (total 3) | a) In 2 cases with urethro-cutaneous fistula, repair of fistula was done only with interposition of Tunica Vaginalis flap.b) In other case with complex urethro-cutaneous fistula staged repair was done.In first stage neo-urethral plate reconstruction with buccal mucosal graft was done. In second stage tubularisation of the neo-urethral plate was done [Table/Fig-3]. |
TIP: tubularised incised plate
Snod grafting done in a patient of secondary hypospadias with –narrow urethral plate.
Type of repair done in Proximal hypospadias cases.
| Primary hypospadias cases (total 4) | In 3 cases Snodgrass/TIP was done with Tunica Vaginalis flap interposition as the second layerIn 1 case with narrow urethral plate, Snod graft (labial graft placed dorsally) with TIP was done. TV flap was used as interposition second layer. |
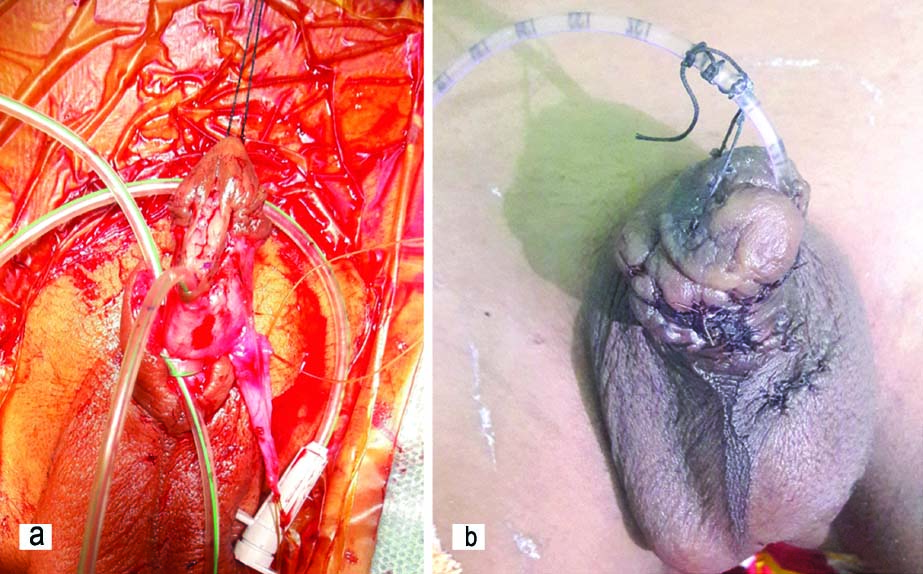
| Secondary hypospadias cases (total 6) | In 3 cases fistula repair with TV flap interposition was done.In 3 cases, one with complex fistula and another with crippled hypospadias staged repair was done. It included a first stage neo-urethral plate creation with BMG and in second stage tubularisation was done [Table/Fig-10] |
Staged repair of hypospadias cripple with severe chordee using buccal mucosal graft.
Recurrences and complications.
| Study groups | No recurrencen (%) | Recurrence/Urethro-cutaneous fistula n (%) | Total | p-value (Fisher’s-exact test) |
|---|
| Adolescent group | 15 (88.2) | 2 (11.7) | 17 | 0.581 |
| Primary-13 | Primary-1 |
| Secondary-2 | Secondary-1 |
| Adult group | 9 (81.8) | 2 (18.1) | 11 |
| Primary-6 | Primary-1 |
| Secondary-3 | Secondary-1 |
| Total | 24 (85.7) | 4 (14.2) | 28 |
Therefore, no association could be demonstrated between the adolescent and adult hypospadias patients in terms of development of complications following surgery. The overall complication rate of the study population was 14.2% (4/28). The success rate of repair among the adolescent group was 88.2% and among the adult group was 81.8%
Discussion
The success rate of hypospadias surgery done in childhood is reported to be high [9]. But studies comparing the results of adolescent and adult hypospadias are scarce. There is enough evidence to suggest that hypospadias in adult life is different from that in childhood. Most of these patients presenting in the adulthood are likely to have undergone at least one previous attempt of repair with further distortion of architecture and vasculature. When such patients are operated, there is a higher risk of complications and failure of surgery, eventually leading to patient dissatisfaction [5,7].
A previous study by Bracka A showed the results of long term psychological and physical sequelae of 213 patients who had undergone previous hypospadias repair over a 30 years period. The findings suggest that patient education and long term follow-up until maturity is required for patient satisfaction [10]. The rate of complications ranges from 27-63% in patients with at least one previous repair attempt [11]. Prat D et al., in their 3 decade long series (from 1978-2009) on childhood hypospadias repair showed that 4.6% of the 820 patients studied required further revision surgery in the adolescence [12].
Older patients undergoing primary repair are often less satisfied and have a worse genital view than the younger population. This is apparent after puberty as increased self-awareness and sexual interest develops. Failed repairs can be devastating to patients and families. The patients may need repair of complications of previous surgery like urethro-cutaneous fistula, urethral stricture, diverticula, persistent chordee, urinary retention, neomeatal stenosis and recurrent urinary tract infections. The median time for diagnosing complications such as fistula, strictures and meatal stenosis is around six months [13]. Bracka A in his study reported that the complication rate of surgeries done in patients with previous attempted repair ranged from 12.4 to 48% [10]. Dodson JL et al., reported that delaying the primary repair in early age was associated with unacceptable results [6]. Hensle TW et al., reported 38% complication rates among the adult patients who had undergone primary repair of hypospadias using the similar techniques used in children [5]. Complications were mostly related to the difference in wound healing rates among the adult population. Histological changes in the skin associated with aging might be the prime factor behind such discrepancies in results. Silva EA et al., described certain age related changes in the urethral plate. The extracellular matrix had more collagen content (type 1 and 3), rare elastic fibres, fewer cells and vascular sinusoids were absent [14].
Complication rate of this series was 14.2% which was less than the reported series among adult patients [7]. In this study, there was no significant difference in complication rates among the adolescent and adult population. Some of the recent studies also reveal that there were no difference in the outcome among the repairs done in children and adults. Sharma G reported good results of TIP procedure done among the adult hypospadias patients and concluded that there were no significant difference in terms of wound healing [8]. In a recent report by Snodgrass W et al., it was concluded that there were no difference in outcome of such surgeries between children and adults [15].
In the index study, the neourethra was covered with a TV flap as the interposition second layer. It has several advantages in the form of easy availability, good vascularity and remains unaffected by different penile disorders. Snow used this flap for the first time while covering the neourethra and it had good results. Since then studies have been done utilising the TV flap where it was used to augment the hypospadias repair or to cover complex fistula repairs [16-18]. The technique of TV flap harvest is simple but requires meticulous dissection. The flap is transferred over the neourethra either via the same incision or by tunnel technique.
However, the overall success rate of distal and proximal hypospadias repair among the adolescent and adult population was 85%, which is in unison with that of the published series comparing the results among the adult and paediatric population [10,13,16]. There was no significant difference in the final outcome of surgery between the adolescent and adult population in this study.
Therefore adolescent and adult hypospadias repair done in a meticulous fashion has a high success rate. Use of TV flap as a second layer interposition can improve the outcome in such patients. Appropriate technique should be tailored to each patient.
Limitation(s)
This study did not include the paediatric population and therefore a direct comparison of results was not possible. The sample size was small and no control group was used to compare the outcomes. The period of follow-up in these patients was also short to determine the final outcome of such surgeries.
Conclusion(s)
Delayed hypospadias repair in the adolescent and adult population is a challenging clinical scenario. When repair is done in a systematic and meticulous fashion, the outcome is satisfactory. There is no significant difference in outcome of hypospadias repair surgery done in the adolescent and adult population. Use of TV flap as a second layer interposition can improve the outcome in such patients. Long term follow-up of these patients would help us to understand the outcome of the surgery and identify potential complications that one may develop.
TIP: tubularised incised plate