Evaluation of Routine Coagulation Parameter in Suspected Acute Myocardial Infarction Patients Attending Emergency Department of Tertiary Care Hospital
Mritunjay Kumar Mishra1, DVSS Ramavataram2, Tejas Shah3
1 Ph.D. Scholar, Department of Biochemistry, SBKSMI and RC, Sumandeep Vidyapeeth University, Vadodara, Gujarat, India.
2 Professor, Department of Biochemistry, SBKSMI and RC, Sumandeep Vidyapeeth University, Vadodara, Gujarat, India.
3 Associate Professor, Department of Biochemistry, SBKSMI and RC, Sumandeep Vidyapeeth University, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. DVSS Ramavataram, Professor, Department of Biochemistry, SBKSMI and RC, Sumandeep Vidyapeeth, Waghodia, Piparia, Vadoadara-391760, Gujarat, India.
E-mail: dvss.ramavataram@gmail.com
Introduction
Heart attack in medical terminology is generally called as Acute Myocardial Infarction (AMI). When blood flow is abruptly cut-off to the heart muscle, it damages the myocardial tissue. This could be the consequence of blocked coronary arteries. The plaque formed due to the deposition of cholesterol and other fatty material over a period of time is the leading cause of this blockage.
Aim
To assess the level of Prothrombin Time (PT) and activated Partial Thromboplastin Time (aPTT) in cardiac and non-cardiac chest pain and their association to Body Mass Index (BMI).
Materials and Methods
The present study was an observational case-control type of study which included 100 subjects of age group 30-65 years from March 2019 to April 2020. Out of them 50 were non-cardiac chest pain individuals which were control and 50 Cardiac chest pain arrived within 6-8 hours of chest pain who suspected to be Myocardial Infarction (MI) from Emergency Department, Dhiraj General Hospital, Gujarat, India. BMI was calculated by height and weight. PT and aPTT analysis was carried out using STAGO-S.A.S. coagulation analyser.
Results
There were increased levels of PT and aPTT (statistically significant) in AMI cases compared to corresponding age and sex matched controls (p<0.0001). Pearson correlation analysis in AMI patients, a slightly positive correlation between BMI and aPTT was observed (r=0.19, p<0.001) and also between PT and aPTT (r=0.66, p<0.001).
Conclusion
There was a slightly positive correlation found between BMI and aPTT which indicated that the weight and height of the patients do not affect the plasma PT and aPTT levels on anticoagulant therapy.
Activated partial prothrombin time, Body mass index, Partial prothrombin time, ST-elevated myocardial infarction
Introduction
A gradual development of atherosclerotic plaque takes place after the deposition of lipids in the arteries over the years. AMI is most often caused by a disruption of an atherosclerotic plaque with the activation and aggregation of platelets, thrombin, and fibrin generation leading to formation of a thrombus [1].
The rupture of an atheromatous plaque in coronary artery is the primary cause of AMI. The rupture exposes a thrombogenic surface initiating thrombin generation, platelet formation and finally formation of thrombus [2]. To monitor the anticoagulant effect of intravenous Unfractionated Heparin (UFH), aPTT is used. Using this test, the doses are adjusted to achieve a predefined “therapeutic range” [3,4]. In Post-MI infarction incident, there will be instability of the endothelium and the activation of platelets and the coagulation system putting the patient to high risk of new thrombotic events [5]. The basis of pathogenesis of various complications of Coronary Artery Disease (CAD) including recurrent MI is due to disturbance in the functions related to haemostasis [6]. PT and its derived methods of Prothrombin Ration (PR), international normalised ratio are comprised in the various measures of the extrinsic pathway of coagulation. Different changes of blood coagulation may play role in the vascular complications such as endothelial damage, platelet hyperactivity etc., [7-9]. Platelet adhesion to the sub endothelial matrix of injured vessel walls requires adhesion of plasma von Willebrand factor (vWF) to collagen or platelet adhesion to subendothelially located vWF. In addition, vWF enhances the adhesion of platelets to fibrin clots and stabilises coagulation factor VIII, which interestingly and may probably predict the risk of cardiovascular diseases [10]. A peptide, known as fibrinopeptide-A is an important marker in the early assessment of enhanced risk leading finally to subsequent death in the patients with MI. If the levels are increased significantly, this marker indicates chances of high mortality. Howsoever, the utility of these markers is very much limited due to its short half-life [11].
In the process of determining various markers of risk for assessment of complications of MI, many parameters have been seed and various markers have been identified. An elevated level of the degraded products of fibrin in plasma which is reflective of enhanced fibrin turnover is one such marker which could be considered. To identify patients with unstable angina with Electrocardiography (ECG) is of not much useful as it has not been found to be much informative. In such scenario, soluble fibrin analysis has been found to be useful. Especially for the early identification of patients with unstable angina [12].
In the literature, it has been found that the pattern of soluble fibrin in AMI is higher than that of corresponding controls indicating a strong predictor value of this parameter especially in younger patients [13]. PT and aPTT measures, extrinsic and intrinsic pathways of coagulation respectively and are used in the laboratories to determine bleeding or clotting tendency of blood [14].
In the current study, it was planned to investigate the level of PT and aPTT in cardiac (Cases-AMI) and non-cardiac chest pain (control) and their association with BMI after anticoagulant therapy.
Materials and Methods
The present study was an analytical/observational type of case control study with a duration of one year i.e., from March-2019 to April-2020 year. As per the minimum study requirement and looking into the feasibility of the availability of patients as per the inclusion criteria, purposive sampling method was chosen for sample collection, where sample size was calculated with 20% allowable error at 95% Class Interval (CI).
The present study was a carried out in the Department of Biochemistry and Department of Cardiology, Smt. BK Shah Medical Institute and Research Centre and Dhiraj General Hospital (DGH) Sumandeep Vidyapeeth, Piparia, Vadodara, Gujarat, India. With the verbal consent from the participants, a total 100 subjects of age group 30-65 years of either sex (Male and Female) were enrolled in this study after getting an ethical approval from Institutional Ethical Committee (SVIEC/ON/MEDI/PhD/18015). Out of them, 50 were enrolled in non-cardiac chest pain individuals and they formed control group and 50 patients having cardiac chest pain came at Emergency Department of Dhiraj Hospital within 6 to 8 hours of chest pain suspected to be due to unstable angina or MI were enrolled and comprised of study group.
Inclusion criteria: Patients willing to participate with following criteria:
✓ Selection of the patients was made after the critical review done by cardiologist on the basis of assessment including both clinical and routine cardiac biomarkers.
✓ The set diagnostic criteria for AMI were that a minimum of the following mentioned criteria must be fulfilled. These criteria were: (i) Clinical history of patients (Characteristic and duration of chest pain); (ii) Cardiac troponin I (cTnI) is above 99th percentile (>0.10 ng/mL) {as per our Hospital}; (iii) ST-segment elevation of >0.2 mV in two contagious leads for STEMI and depression of >0.1 mV in ST segment of two contagious leads for NSTEMI in their ECG presentation.
✓ All the patients had been supplemented with anticoagulant therapy (i.e., Heparin 5000 Units iv bolus) and received aspirin (85-325 mg) with different drug regimen.
✓ Non-cardiac chest pain (basically epigastric pain) comprised as controls.
Exclusion criteria: Patients with diabetes mellitus, chronic muscle disease, renal disease, autoimmune disease, arthritis, any inflammatory disease, recent surgery and any other disease except AMI were excluded from the study.
Sample collection and processing: Approximately, five mL blood sample was taken from each and every individual having ischemic type of chest i.e., AMI and controls under all aseptic precautions and was left for 30 minutes for clotting. Clotted samples were centrifuged at 3000 rpm for 10 to 20 minutes. Supernatant (plasma) was collected in clean and dry test tube for analysis of PT and aPTT were estimated by STAGO-SAS coagulation analyser. The patient confidentiality was maintained at each and every levels.
Statistical Analysis
Data were analysed with the help of software program Statistical Package for Social Sciences (SPSS version 21, Chicago). The statistical differences between cases and control were determined by student independent sample t-test. Relationship between BMI and PT and aPTT was determined by Spearman’s correlation analysis. The p-value <0.005 were considered as statistically highly significant.
Results
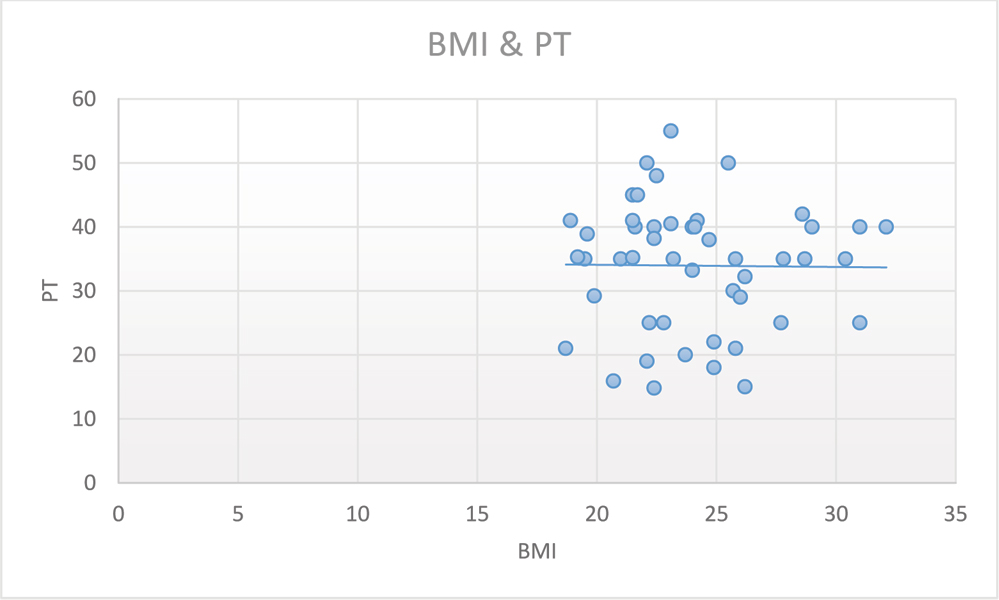
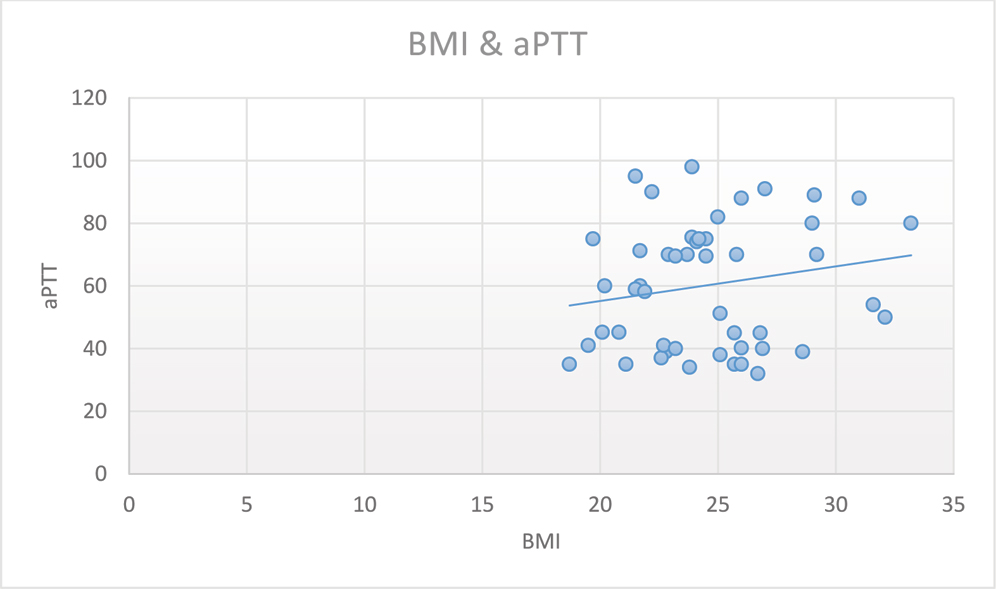
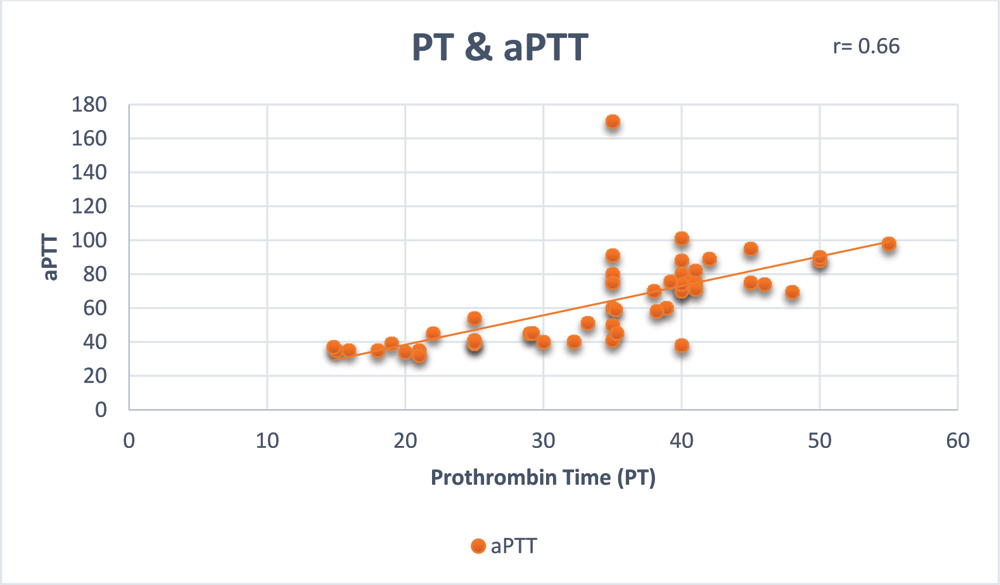
A total of 100 subjects were enrolled in this study, comprising of 50 cases of AMI and 50 were enrolled as controls. BMI was calculated taking into the account of height in cm and weight in kg as per the World Health Organisation (WHO) criteria (BMI in kg/m2 was calculated by formula height (m2 and weight (Kg)) in cardiac chest pain (Case group i.e., AMI) and non-cardiac chest pain (control group). The data of the present study was presented in the form of mean and standard deviation (SD) (Mean±SD). The mean age (years) of the cases was 50.60±11.76 years and controls was 47.84±10.28 years, and found to be statistically insignificant. The mean levels of BMI in cases was (24.75±3.43 kg/m2) compared to control subjects (21.74±2.37 kg/m2) (p<0.001). In comparison of coagulation parameter (PT and aPTT) in cases and controls, we found there is an increased mean levels of PT (34.29±9.83 seconds) and aPTT (63.22±25.73 seconds) in cases as compared with the respective controls (12.74±2.23 seconds and 28.12±4.64 seconds) and found to be statistical significant (p<0.0001) shown in [Table/Fig-1]. Weak negative correlation was found between BMI and PT, (r=-0.01, p<0.005) [Table/Fig-2]. A positive correlation (r=0.19, p<0.001) was found between BMI and activated Partial Thromboplastin Time (aPTT) [Table/Fig-3]. A significantly positive correlation (r=0.66, p<0.001) was observed when the relationship between PT and aPTT was studied [Table/Fig-4].
Mean levels of coagulation parameters, BMI and age in AMI cases and controls.
| Variables | Non-cardiac chest pain (Control) | Cardiac chest pain (Case-AMI) | p-value |
|---|
| Age (years) | 47.84±10.28 | 50.60±11.76 | 0.21# |
| BMI (Kg/m2) | 21.74±2.37 | 24.75±3.43 | 0.001** |
| PT (Seconds) | 12.74±2.23 | 34.29±9.83 | 0.001** |
| aPTT (Seconds) | 28.12±4.64 | 63.22±25.73 | 0.001** |
**p≤0.001: highly statistical significant, *p≤0.005: statistically significant and p≥0.005; #Statistically– non-significant; PT: Prothrombin time; aPTT: Activated partial thromoboplastin time; BMI: Body mass index
Correlation between BMI and PT in Case group.
Slightly negative relationship between BMI and Prothrombin Time (PT) (r=-0.01); p-value <0.005
Correlation between BMI and aPTT in case group.
Positive correlation between BMI and aPTT (r=0.19); p-value <0.001
Correlation between PT and aPTT in case group.
Positive and significant relationship between PT and aPTT (r=0.66); p-value <0.001
Discussion
In the extrinsic (tissue factor) pathway of coagulation, the coagulation parameters are one of the functional determinants. It is sensitive to the vitamin K dependent clotting factors (factor- II- i.e., prothrombin, VII and X). Tissue factor (factor-III) is a transmembrane protein that is widely expressed on cells of non-vascular origin, which activates factor -VII during initiation of cascade mechanism results in fibrin production and clot formation [15]. Haemostatic function has been linked to the pathogenesis of the complications of CAD including recurrent MI. To understand the pathophysiology of these events, there is a need for the development of treatment strategies including rapid reperfusion, pharmacological agents and anticoagulant therapy, and that may help to improve the clinical outcome [16]. The primary objective was to analyse the relationship between BMI and PT and aPTT and the secondary objective was to see the relation between PT and aPTT in the early phases of AMI patients supplemented with UFH. In the present study, PT and aPTT was compared with BMI in cardiac chest pain (Cases) and non-cardiac chest pain (Controls). A statistically significant (p<0.0001) increase in the concentration of PT and aPTT in cases was observed compared to controls. PT along with aPTT is routinely well-established parameters for attempting invasive medical procedure so as to make sure the existence of normal clotting activity in admitted patients. The general trend is that patients admitted with the cardiac chest pain are more inclined towards undergoing invasive procedure. The results of the present study were in correlation with that of the results of the similar study reported by Khan HA et al., who have conducted the similar study on 67 patients of AMI and found significantly increased PT and aPTT levels in AMI as compared with control groups [17].
Heparin (Unfractionated or Low molecular weight) is considered as a standard therapy in the management of coronary events. The anticoagulant therapy (Heparin/Warfarin) affects the function of the coagulation cascade and helps to inhibit the formation of clot. The coagulation parameters (PT, aPTT and INR) are used to monitor the effectiveness of the anticoagulants [16]. To analyse the relationship between BMI and PT and aPTT, Pearson correlation analysis was used. A weak negative relationship (r=-0.01) was observed between BMI and PT. aPTT is the common screening test done to evaluate the intrinsic clotting system and it is a common test to monitor heparin therapy. Based on that, relationship between BMI and aPTT was also analysed. The relationship was slightly positive (r=0.19). That means the association shows that if supplemented with weight based heparin regimen to patients could be beneficial in achieving of aPTT threshold with 24 hours of time period. Present results also strongly agree the findings of other workers regarding ineffectiveness of non-weight based heparin regimen in the achievement of aPTT threshold within the stipulated time period [18].
aPTT has also been used as a marker for assessing anticoagulant with UFH. Earlier workers (16) have used Rashake nomogram, which provides an achievement of aPTT within the target range of anticoagulation (60-85 seconds) [16].
The relationship between PT and aPTT was also analysed in the early phases of AMI cases and observed that there was a significant positive correlation between PT and aPTT levels (r=0.66, p<0.001) [Table/Fig-4]. This association indicates mutual interaction between extrinsic and intrinsic pathways of blood coagulation as PT is used to measure the integrity of extrinsic pathways, whereas aPTT used to measure the integrity of intrinsic pathways [17].
Khan HA et al., have conducted the similar study on 67 patients of AMI and found significantly increased PT and aPTT levels in AMI as compared with control groups [17]. These workers also did not find any correlation between these coagulation factors and gender, BMI and commented that age should not take into consideration while interpreting these coagulation markers, though a slight correlation was observed but we did not observe a strong relationship between BMI and aPTT. Heparin is commonly used anticoagulant in the Cath laboratory for thinning of blood clot and its dose depends on the severity of the thrombus or clot present in the artery. Coagulation markers (mainly aPTT) can be used to accomplish the therapeutic threshold and along with existing cardiac biomarkers (cTnI or CK-MB) could be beneficial to see the status of clot after initial doses of heparin supplementation.
Limitation(s)
The sample size of the present study was small hence a definitive conclusion cannot be drawn. One of the difficult aspect of this type of study is the availability of patients within the set time limit as lots of variations are observed during their visit in an emergency condition with heart attack manifestations. Patient classification on ECG representation was not done as per the feasibility of the type of patients. Also, authors were not able to follow the Roshake nomogram for heparin supplementation. Further study is needed to establish the concept as present study has limitations in sample size which was small.
Conclusion(s)
The increased levels of PT and aPTT may serve as indices for evaluating haemostatic abnormalities in AMI patients and the increased plasma concentration is also helpful to determine the bleeding and clotting tendencies in AMI patients. There is a slightly positive correlation found between BMI and aPTT indicates that the weight and height of the patients do not affect the plasma PT and aPTT levels on the outcome of anticoagulant therapy.
**p≤0.001: highly statistical significant, *p≤0.005: statistically significant and p≥0.005; #Statistically– non-significant; PT: Prothrombin time; aPTT: Activated partial thromoboplastin time; BMI: Body mass index
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Sep 15, 2020
Manual Googling: Nov 21, 2020
iThenticate Software: Dec 29, 2021 (12%)
[1]. Corti R, Farkouh ME, Badimon JJ, The vulnerable plaque and acute coronary syndromesAm J Med 2002 113(8):668-80.10.1016/S0002-9343(02)01344-X [Google Scholar] [CrossRef]
[2]. Fuster V, Badimon L, Badimon JJ, Chesebro JH, The pathogenesis of coronary artery disease and the acute coronary syndromesN England J Med 1992 326(5):242-50.10.1056/NEJM1992012332604061727977 [Google Scholar] [CrossRef] [PubMed]
[3]. Hirsh J, Warkentin TE, Shaughnessy SG, Anand SS, Halperin JL, Raschke R, Heparin and low-molecular weight heparin: Mechanisms of action, pharmacokinetics, dosing considerations, monitoring, efficacy, and safetyChest 2001 119(1 Suppl):64s-94s.10.1378/chest.119.1_suppl.64S11157643 [Google Scholar] [CrossRef] [PubMed]
[4]. Brill-Edwards P, Ginsberg JS, Johnston M, Hirsh J, Establishing a therapeutic range for heparin therapyAnn Intern Med 1993 119(2):104-09.10.7326/0003-4819-119-2-199307150-000028512158 [Google Scholar] [CrossRef] [PubMed]
[5]. Reganon E, Vila V, Martinez-Sales V, Vaya A, Aznar J, Inflammation, fibrinogen and thrombin generation in patients with previous myocardial infarctionHematological 2002 87(7):740-45. [Google Scholar]
[6]. Kostis JB, Baughman DJ, Kuo PT, Association of recurrent myocardial infarction with hemostatic factors: A prospective studyChest 1982 81(5):571-75.10.1378/chest.81.5.5717075276 [Google Scholar] [CrossRef] [PubMed]
[7]. Schrader J, “Stroke and hypertension,”Der Internist 2009 50(4):423-32.10.1007/s00108-008-2291-919308341 [Google Scholar] [CrossRef] [PubMed]
[8]. Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH, Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: The ENCORE studyArchives of Internal Medicine 2010 170(2):126-35.10.1001/archinternmed.2009.47020101007 [Google Scholar] [CrossRef] [PubMed]
[9]. Alhamami OM, AL-Mayah JY, AL-Mousawi NR, AL-Mousawi HI, Pleiotropic effects of antihypertensive drugsThe Islamic University Journal 2007 15(1):01-12. [Google Scholar]
[10]. Martin F, Ingrid F, Judith M, Kety LH, Vlcek M, Losert H, Platelet function predicts myocardial damage in patients with acute myocardial infarctionCirculation 2004 110(11):1392-97.10.1161/01.CIR.0000141575.92958.9C15313953 [Google Scholar] [CrossRef] [PubMed]
[11]. Li YH, Teng JK, Tsai WC, Tsai LM, Lin LJ, Guo HR, Prognostic significance of elevated hemostatic markers in patients with acute myocardial infarctionJ American College of Cardiology 1999 33(6):1543-48.10.1016/S0735-1097(99)00081-9 [Google Scholar] [CrossRef]
[12]. Galvani M, Ferrini D, Ottani F, Eisenberg PR, Early risk stratification of unstable angina/ non-Q myocardial infarction: Biochemical markers of coronary thrombosisInt J Cardiology 1999 68(1):S55-S61.10.1016/S0167-5273(98)00292-7 [Google Scholar] [CrossRef]
[13]. Saigo M, Waters DD, Abe S, Biro S, Minagoe S, Maruyama I, Soluble fibrin, C-reactive protein, fibrinogen, factor VII, antithrombin, proteins C and S, tissue factor, D-dimer, and prothrombin fragment 1 + 2 in men with acute myocardial infarction ≤45 years of ageAm J Cardiol 2004 94(11):1410-13.10.1016/j.amjcard.2004.07.14415566913 [Google Scholar] [CrossRef] [PubMed]
[14]. Ardissino D, Merlini PA, Bauer KA, Galvani M, Ottani F, Franchi F, Coagulation activation and long-term outcome in acute coronary syndromesBlood 2003 102(8):2731-35.10.1182/blood-2002-03-095412843003 [Google Scholar] [CrossRef] [PubMed]
[15]. Kitchen S, Preston FE, Standarisation of prothrombin time in laboratory control and oral anticoagulant therapySemin Thrombo Hemost 1999 25(1):17-25.10.1055/s-2007-99641910327216 [Google Scholar] [CrossRef] [PubMed]
[16]. Mitrovaska S, Jovanova S, Low molecular weight heparin enoxaparin in the treatment of acute coronary syndrome without ST segment elevationBratisi lek listy 2009 100(1):45-48. [Google Scholar]
[17]. Khan HA, Alhomida AS, Rammah TYA, Sobki SH, Ola MS, Khan AA, Alterations in prothrombin time and activated partial thromboplastin time in patients with acute myocardial infarctionInt J Clinical Experiments 2013 6(4):294-97. [Google Scholar]
[18]. Granger CB, Hirsch J, Califf RM, Col J, White HD, Betriu A, Activated partial thromboplastin time and outcome after thrombolytic therapy for acute myocardial infarction: Results from the GUSTO-I trialCirculation 1996 93(5):870-78.10.1161/01.CIR.93.5.8708598077 [Google Scholar] [CrossRef] [PubMed]