Giant Cell Tumour of Clivus: A rare Case Report
Swapan Shantiram Goswami1, Sonal Jain2, Shalin Nagori3
1 Professor, Department of Pathology, Smt.B.K. Shah Medical College, Sumandeep Vidyapeeth Deemed to be university, Vadodara, Gujarat, India.
2 Second Year Resident, Department of Pathology, Smt.B.K. Shah Medical College, Sumandeep Vidyapeeth Deemed to be university, Vadodara, Gujarat, India.
3 Second Year Resident, Department of Pathology, Smt.B.K. Shah Medical College, Sumandeep Vidyapeeth Deemed to be university, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shalin Nagori, 113, Gargi Sumandeep Vidyapeeth, Vadodara, Gujarat, India.
E-mail: shalinnagori07@gmail.com
Giant Cell Tumours (GCT) of the skull is rare, being less than 0.05% of all skeletal tumours. They are usually located in the middle cranial fossa affecting the temporal, sphenoid, petrosal and occipital bone. Clival GCT is rarer and 15 cases are described in the literature. Authors report a case of a female patient aged 20 years, who complained of headache with decrease in vision of left eye. Neurological examination revealed left optic nerve palsy. Laboratory test of Vitamin B12, blood urea, Serum Creatinine, Serum Electrolytes were within normal range. Complete blood count showed mild anaemia. The serum calcium and parathyroid hormones were within normal range. Computed Tomography (CT) scan and Magnetic Resonance Imaging (MRI) were done, which demonstrated expansile destructive lytic lesion involving sphenoid bone and clivus, reaching upto sellar, parasellar regions, sphenoid sinus and left posterior ethmoid sinus, effacing left optic foramina and posteriorly effacing prepontine cistern. The left internal carotid artery was partially encased by the mass. The tumour was partially removed by endoscopic trans-nasal trans-sphenoidal approach. Histopathology confirmed it as a benign GCT. Surgical treatment of clival GCTs are fraught with complication because of its close proximity to vital structures. High vascularity, potential malignant behaviour, inaccessibility and very few published cases preclude a definite outcome of this lesion. Histopathology is necessary to differentiate various lytic lesion like chordoma, aneurysmal bone cyst, invasive pituitary adenoma, chondrosarcoma and brown tumour (parathyroidism).
Left optic nerve palsy, Osteoclastoma, Skull base tumour
Case Report
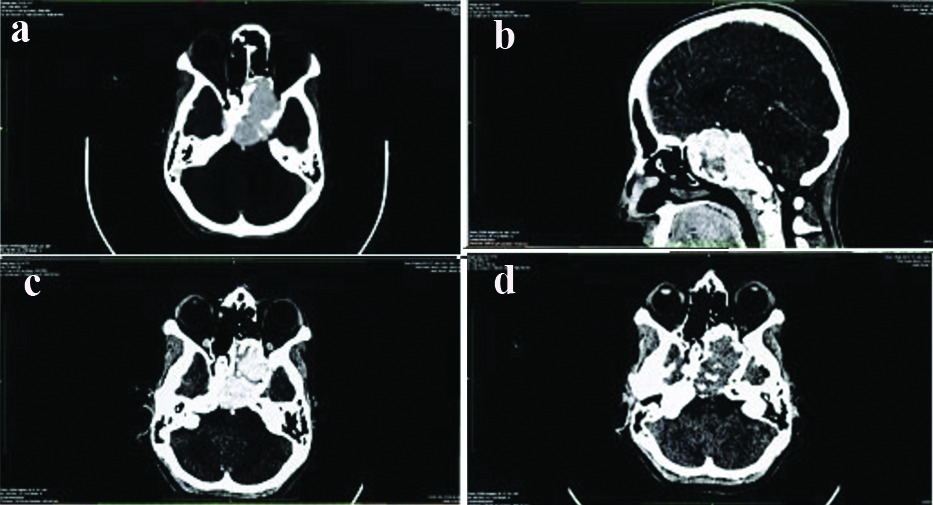
A 20-year-old female with one month history of headache and decreased vision in left eye. She had no history of trauma or surgery. No past medical history. Physical examination revealed overall good health. Neurological examinations revealed left optic nerve palsy. Laboratory tests were conducted, the blood biochemical tests included Urea-27 mg%, Serum Creatinine 0.8 mg%, Electrolytes Na+141 mμ/l, K+4.1 mμ/l, Cl+103 mμ/l. The complete blood count showed the following results Haemoglobin (Hb)-10.0 gm%, Total White Blood Cell (WBC) count-4200 cells/cumm, Differential count-61/30/04/05, Packed Cell Volume-31%, Mean Corpuscular Volume (MCV)-81.6fl, Mean Corpuscular Haemoglobin (MCH)-26.3, Mean Corpuscular Haemoglobin Concentration (MCHC)-32.3%, Total Red Blood Cell (RBC) Count-3.8Mil/μL, Red Cell Distribution Width (RDW)-13.3%, Platelet count-1.72 lac/cumm. Parathyroid hormone was 36.03 pg/mL (Normal range-15-65), Serum calcium was 9.2 mg/dL (Normal range 8.4-10.2). CT scan brain and Paranasal Sinuses (PNS) demonstrated expansile destructive lytic lesion which was seen involving sphenoid bone and clivus reaching up to sellar, parasellar regions, sphenoid sinus and left posterior ethmoidal sinus and effacing left optic foramina and posteriorly effacing prepontine cistern. Lesion was seen to partially encase the internal carotid artery. The mass lesion showed heterogenous enhancing soft tissue density component. Pituitary gland was not seen separately from the lesion. Small bulge was seen in the suprasellar region [Table/Fig-1].
a) Axial CT scan demonstrate expansile lytic lesion involving sphenoid bone. b) Sagittal CT scan demonstrate expansile lytic lesion involving sellar, suprasellar, sphenoid bone and clivus. c) Axial CT scan demonstrate expansile lytic lesion involving sellar and suprasellar region. d) Axial CT scan demonstrate expansile lytic lesion involving suprasellar regions left optic foramina.
Magnetic Resonance Imaging (MRI) scan was done using T1-weighted (T1W), T2-weighted (T2W), Diffusion Weighted (DW), Gradient Recalled Echo (GRE) and Fluid Attenuated Inversion Recovery (FLAIR) sequences in various planes. Expansile destructive soft tissue intensity heterogeneously enhancing mass lesion was seen in body of sphenoid bone/clivus appearing hyperintense on both T2W and FLAIR sequences. Mass was extending into the prepontine cistern posteriorly and parasellar region and was pushing the pituitary gland cranially. The left internal carotid artery was partially encased by mass. Fullness was seen in the region of optic foramen on left side with minimal erosion. The lesion was extending into sphenoid and left posterior ethmoid sinus. Chordoma and parathyroid tumour were considered in the differential diagnosis after clinical and radiological investigation.
Diagnostic cerebral angiography was done which showed clival tumour supplied by multiple small vessels of both left and right internal maxillary arteries and branches from left internal carotid artery through meningohypophyseal trunk. The tumour was removed using an endoscopic trans-nasal trans-sphenoidal method.
Then specimen was sent to the histopathology. Gross examination showed greyish white soft tissue bits aggregating 2×2×0.1 cm. Sections were stained with H&E.
Histopathological examination, showed bony spicules, fibro collagenous tissue and presence of tumour tissue with diffusely scattered multi-nucleated giant cells within a stroma of spindle cells [Table/Fig-2a-c]. GCT showed two populations of cells,
a) The figure shows foci of bony spicules, fibro collagenous tissue and tumour tissue with evenly scattered multi-nucleated giant cells in a spindle to polygonal cell stroma (Stain: Haematoxylin and eosin, 40×). b) Giant Cell Tumour (GCT) with a mixture of mononuclear spindle cells and multi-nucleated giant cells. (Stain: Haematoxylin and eosin, 100×). c) High power appearance of Giant Cell Tumour (GCT). (Stain: Haematoxylin and eosin, 400×)
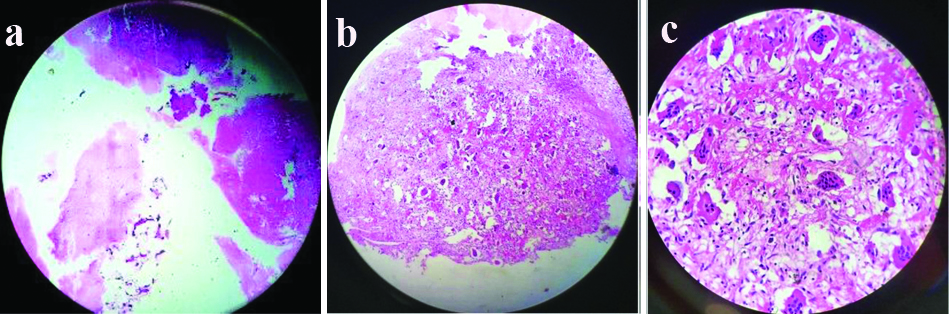
Mononuclear stromal cells
Osteoclast-type giant cells
The giant cells were large and had over 20 or 30 nuclei
The stromal cells did not showed any nuclear atypia. The differential diagnosis after histopathological examination was aneurysmal bone cyst and GCT. Finally, the diagnosis of GCT of clivus was made. The treatment of the patient included surgical removal of tumour by endoscopic trans-nasal transsphenoidal method followed by radiotherapy in a dose of 54 Gy in 27 fraction over six weeks. The patient was well, till one year after operation in mid December 2020. Further contact was not possible.
Discussion
The GCT is tumours involving the bone and constitutes about 5% of all primary tumours of the skeletal system [1]. It usually occurs in the long bones around the joints in the epimetaphyseal regions of the bone on reaching maturity. Flat bone involvement of the skull, facial bones, pelvis and spine are rare, and GCT involving the skull constitutes <1% of the GCTs involving the skeletal system [2]. Clival GCT remains a very rare tumour forming 0.05% of primary skeletal tumour and less than 15 cases are described [3]. The tumour affects females and males equally. It is commonly seen between 20 years to 40 years of age.
GCTs are usually benign, but may be locally aggressive. Histopathologically, osteoclast like multi-nucleated giant cells are seen evenly dispersed in a background of stromal mononuclear cells and histiocytes. It is this stromal cell which forms the neoplastic component and may display malignant characteristics which may even metastasize rarely to the lungs [4]. GCTs are seen comparatively more in the Asian population affecting Chinese and Indians from 14.2 to 20.3% of the primary bone tumours [1,5]. Clinical features vary according to the site of tumour and involvement of particular cranial nerves I, II, III, IV, and VI. Past cases reported on GCT of clivus have been tabulated and discussed briefly in [Table/Fig-3] [2-4,6-16].
Review of literature of GCT of clivus [2-4,6-16].
| Author, publication year, Reference | Age (years/sex) | Clinical features | Size (cm) | Duration of symptoms | MRI imaging T1/T2 | Vascularity | Surgery | RT | Outcome | Follow-up (months) |
|---|
| Wolfe JT et al., 1983 [8] | 16/Female | Headache, diplopia, visual disturbances | NA | 4-7 weeks | NA | NA | STR | Yes | Alive with residual tumour | 96 |
| Kattner KA et al., 1998 [9] | 9/Female | Headache, diplopia | NA | 1 month | Space enhancing lesionT2-hypointense and isointense | Moderately vascular | Biopsy (TSS) | Yes | Alive with residual tumour | 12 |
| Sharma RR et al., 2002 [10] | 18/Female | Headache, progressive hearing loss, facial paresis | NA | 6 months | Space enhancing lesionT1-isointenseT2-hyperintense | Moderately vascular | NTR | Yes | Alive | 12 |
| Sharma RR et al., 2002 [10] | 12/Female | Headache, progressive hearing loss, facial paresis, nasal regurgitation, nasal twang | NA | 3 months | Space enhancing lesionT1-isointenseT2-hyperintense | Moderately vascular | GTR | Yes | Alive | 12 |
| Zorlu F et al., 2006 [11] | 14/Female | Headache, diplopia | 6*4*3.5 | 2.5 months | Space enhancing lesionDemostrated a lytic expansile lesion | NA | STR | Yes | Alive with residual tumour | 24 |
| Gupta R et al., 2008 [12] | 17/Female | Headache, diplopia, amenorrhea, visual disturbance | 7.6*5.4 | 6 months | Space enhancing lesion | Moderatey vascular | STR | Yes | Alive with residual tumour | 24 |
| SasagawaY et al., 2012 [13] | 26/Male | Headache, diplopia | 3*3 | NA | Space enhancing lesionT1-isointenseT2-hyperintense | Highly vascular, massive bleeding | STR | Yes | Death | 9 |
| Iacoangeli M et al., 2013 [14] | 31/Male | Headache, diplopia | NA | NA | Space enhancing lesion, large GCT originating from the clivus | Highly vascular, massive bleeding, ICA rupture | NTR | No | Alive with residual tumour | 24 |
| Roy S et al., 2013 [15] | 19/Male | Headache, facial hyperasthesia | 5.6*3.6*3.5 | 6 months | T1-large expansile massT2-hyperintense | High vascularity | GTR | Yes | Alive with residual tumour | 18 |
| Agrawal A et al., 2014 [6] | 62/Male | Headache, diplopia | NA | 3 months | Space enhancing lesion | NA | Endoscopy f/b STR | NA | No | NA |
| Shibao S et al., 2015 [2] | 25/Male | Diplopia | 5.1*3.1*4.9 | 1 month | Space enhancing lesion T1-isointenseT2-hyperintense | Highly vascular, massive bleeding, brain stem invasion | STR | Yes | Death | 31 |
| Patibandla MR et al., 2017 [4] | 20/Male | Left hemicranial headache, vomiting, dropping of eyelid | NA | 6 weeks | T1/T2- isointense | NA | STR | Yes | Alive with residual tumour | 3 |
| Satapathy A et al., 2018 [16] | 25/Male | Headache, diplopia, diminished vision | 5.7*4.5*5.7 | 4 months | Space enhancing lesion, large mass centered on clivus | Moderately vascular | GTR | Yes | Alive | 8 |
| Scotto di Carlo F et al., 2018 [3] | 55/Male | Headache, vomiting | NA | NA | Space enhancing lesion lobulated mass originating from clivus till sella and epitropheus | NA | Sub-occipital approach f/b redosurgery | Yes | alive | 36 |
| Scotto di Carlo F et al., 2018 [3] | 25/M | Headache, diplopia | NA | NA | Space enhancing lesion lobulated mass | NA | Endoscopic endonasal approach | No | Alive | 72 |
| Singh S et al., 2020 [7] | 35/Female | Headache, diplopia, blurred vision | 4*2.5*0.5 | 6 months | Space enhancing lesion homogenously enhancing lesion | Highly vascular | Endoscopic endonasal trans-sphenoidal subtotal resection | Yes (60Gy/45fr) | Alive with residual tumour | 6 |
| Goswami SS et al., 2021 (Present Case) | 20/Female | Headache diminished vision | NA | 1 month | Space enhancing lesionExpansile lytic lesion T2/FLAIR - hyperintense | NA | Endoscopic trans-nasal transsphenoidal resection | Yes (54Gy/27fr) | Alive with residual tumour | 12 |
NA: Not available; STR: Subtotal resection; TSS: Trans-sphenoidal sinus surgery; GTR: Gross total resection; ICA: Internal carotid artery; NTR: Near total resection; GCT: Giant cell tumour; f/b: followed by
The patient presents with headache, visual disturbances, defects in visual fields, diplopia, weakness and paralysis of eye muscles, proptosis, loss of hearing, endocrine dysfunction and dysfunction of third and sixth cranial nerves [4,6].
In the present case, the patient had tumour involving the cranial nerves I and III and so presented with visual disturbances in the left eye. Histologically, the GCT showed scattered osteoclastic giant cells in the background of benign mononuclear stromal cells. Radical surgery with complete removal of the diseased bone is difficult in clival GCTs due to its peculiar anatomical location and approximation to adjacent vital neurovascular structures [1]. In the present case minimal invasive endoscopic surgery was carried out through the trans-nasal, transsphenoidal approach with partial resection of the tumour.
GCTs are resistant to radiotherapy and show a potential for malignant transformation. An adjunctive therapy may be recommended following partial tumour excision of skull base [1]. Chemotherapy with Adriamycin and bisphosphonates has been tried [4]. Radiographical and histological grading of the tumours don’t correlate with the clinical behaviour. It is the extent of resection in surgery which affects the prognosis. Usually the recurrences occur within a couple of years following treatment hence follow-up is necessary. Availability of very few recorded; published cases preclude a definite prognosis of clival GCTs. With the present case, totally 16 cases have been identified [7]. The male to female ratio is equal. The patient’s age ranged from 9 to 62 years. The duration of the tumour ranged from 1 to 6 months. The commonest complaints of the patients were headache with diplopia. The MRI findings revealed space enhancing lesions. The lesions were moderate to highly vascular. Fourteen patients had been treated with radiotherapy. Of the 16 patients, two have expired. The longest survivor is eight years on follow-up. In the present case the patient has been on follow-up for one year and is alive.
Conclusion(s)
GCT of clivus and sphenoid bone is very rarely seen. The tumour bone is located in the cranial cavity at inaccessible location and is in close approximation to vital structures, hampering complete excision. Histopathological examination is necessary due to presence of various osteolytic lesions in this location viz., chordoma, aneurysmal bone cyst, chondrosarcoma, parathyroid tumour and invasive pituitary adenoma. Malignant change in GCT has to be ruled out by histopathology as rare metastasis to lungs may occur.
NA: Not available; STR: Subtotal resection; TSS: Trans-sphenoidal sinus surgery; GTR: Gross total resection; ICA: Internal carotid artery; NTR: Near total resection; GCT: Giant cell tumour; f/b: followed by
Author Declaration:
Financial or Other Competing Interests: None
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 27, 2020
Manual Googling: Jan 08, 2021
iThenticate Software: Jan 23, 2021 (2%)
[1]. Zhao J, Qian T, Zhi Z, Li Q, Kang L, Wang J, Giant cell tumour of the clivus: A case report and review of the literatureOncol Lett 2014 8(6):2782-86.10.3892/ol.2014.252825364465 [Google Scholar] [CrossRef] [PubMed]
[2]. Shibao S, Toda M, Yoshida K, Giant cell tumours of the clivus: Case report and literature reviewSurg Neurol Int 2015 6(Suppl 25):S623-27.10.4103/2152-7806.17045926682086 [Google Scholar] [CrossRef] [PubMed]
[3]. Scotto di Carlo F, Divisato G, Iacoangeli M, Esposito T, Gianfrancesco F, The identification of H3F3A mutation in giant cell tumour of the clivus and the histological diagnostic algorithm of other clival lesions permit the differential diagnosis in this locationBMC Cancer 2018 18(1):35810.1186/s12885-018-4291-z29609578 [Google Scholar] [CrossRef] [PubMed]
[4]. Patibandla MR, Thotakura AK, Rao MN, Addagada GC, Nukavarapu MC, Panigrahi MK, Clival giant cell tumour- A rare case report and review of literature with respect to current line of managementAsian J Neurosurg 2017 12(1):78-81.10.4103/1793-5482.14511228413541 [Google Scholar] [CrossRef] [PubMed]
[5]. Saikia KC, Bhuyan SK, Borgohain M, Saikia SP, Bora A, Ahmed F, Giant cell tumour of bone: An analysis of 139 Indian patientsJ Orthop Sci 2011 16(5):581-88.10.1007/s00776-011-0033-721833611 [Google Scholar] [CrossRef] [PubMed]
[6]. Agrawal A, Gali R, Shanthi V, Ramakrishna BA, Mohan KV, Giant cell tumour of the clivus with presence of epithelioid histiocytesAsian J Neurosurg 2014 9(1):48-49.10.4103/1793-5482.13107824891892 [Google Scholar] [CrossRef] [PubMed]
[7]. Singh S, Mankotia DS, Shankar KB, Siraj F, A rare tumour of clivus masquerading as pituitary adenomaAsian J Neurosurg 2020 15(4):1091-95.10.4103/ajns.AJNS_188_2033708696 [Google Scholar] [CrossRef] [PubMed]
[8]. Wolfe JT 3rd, Scheithauer BW, Dahlin DC, Giant-cell tumour of the sphenoid bone. Review of 10 casesJ Neurosurg 1983 59(2):322-27.10.3171/jns.1983.59.2.03226864300 [Google Scholar] [CrossRef] [PubMed]
[9]. Kattner KA, Stroink A, Gupta K, Fukushima T, Li C, Giant cell tumour of the sphenoid boneSkull Base Surg 1998 8(2):93-97.10.1055/s-2008-105858217171058 [Google Scholar] [CrossRef] [PubMed]
[10]. Sharma RR, Mahapatra AK, Pawar SJ, Sousa J, Dev EJ, Craniospinal giant cell tumours: Clinicoradiological analysis in a series of 11 casesJ Clin Neurosci 2002 9(1):41-50.10.1054/jocn.2001.096311749016 [Google Scholar] [CrossRef] [PubMed]
[11]. Zorlu F, Selek U, Soylemezoglu F, Oge K, Malignant giant cell tumour of the skull base originating from clivus and sphenoid boneJ Neurooncol 2006 76(2):149-52.10.1007/s11060-005-4343-516205965 [Google Scholar] [CrossRef] [PubMed]
[12]. Gupta R, Mohindra S, Mahore A, Mathuriya SN, Radotra BD, Giant cell tumour of the clivusBr J Neurosurg 2008 22(3):447-49.10.1080/0268869070181894318568739 [Google Scholar] [CrossRef] [PubMed]
[13]. Sasagawa Y, Tachibana O, Shiraga S, Takata H, Kinoshita E, Nojima T, Secondary malignant giant cell tumour of the clivus: Case reportClin Neurol Neurosurg 2012 114(6):786-88.10.1016/j.clineuro.2011.12.04122277296 [Google Scholar] [CrossRef] [PubMed]
[14]. Iacoangeli M, Di Rienzo A, Re M, Alvaro L, Nocchi N, Gladi M, Endoscopic endonasal approach for the treatment of a large clival giant cell tumour complicated by an intraoperative internal carotid artery ruptureCancer Manag Res 2013 5:21-24.10.2147/CMAR.S3876823403482 [Google Scholar] [CrossRef] [PubMed]
[15]. Roy S, Joshi NP, Sigamani E, Malik A, Sharma MC, Mohanti BK, Clival giant cell tumour presenting with isolated trigeminal nerve involvementEur Arch Otorhinolaryngol 2013 270(3):1167-71.10.1007/s00405-012-2249-323143505 [Google Scholar] [CrossRef] [PubMed]
[16]. Satapathy A, Tripathi M, Chauhan RB, Gurnaani J, Mohindra S, Giant cell tumour at the clivus: Not an area 51Neurol India 2018 66(3):861-64.10.4103/0028-3886.23228629766962 [Google Scholar] [CrossRef] [PubMed]