Keratitis Due to a Rare Fungus Colletotrichum dematium: A Case Report
Archana Bhimrao Wankhade1, Vijaya Sahu2, Pratibha Sharma3, Padma Das4
1 Associate Professor, Department of Microbiology, AIIMS, Raipur, Chhattisgarh, India.
2 Associate Professor, Department of Ophthalmology, AIIMS, Raipur, Chhattisgarh, India.
3 Senior Resident, Department of Microbiology, AIIMS, Raipur, Chhattisgarh, India.
4 Additional Professor, Department of Microbiology, AIIMS, Raipur, Chhattisgarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Archana Bhimrao Wankhade, Associate Professor, Department of Microbiology, AIIMS, Raipur, Chhattisgarh, India.
E-mail: achukeche@gmail.com
Keratitis is a very serious clinical condition caused by bacteria, fungi or parasites. It is associated with serious complications like blindness or endophthalmitis if remained undiagnosed. A 42-year-old male patient with the history of foreign body inoculation presented with mild pain and redness. After clinical examination, fungal keratitis was diagnosed. Corneal scrapping was sent for microbiological investigation. A very rare fungi Colletotrichum dematium was isolated and identified. Patient was managed with Natamycin tab fluconazole and atropin eye drops. To know the geographical distribution of the rare fungi, more and more cases should be studied and reported, which will help in management of rare fungi and standardisation of therapy.
Corneal ulcer, Dematitious fungi, Fungal keratitis, Unuseal fungi
Case Report
A 42-year-old male patient presented with complaint of redness, watering, pain, and photophobia associated with diminution of vision in the Left Eye (LE) since three weeks. He encountered unidentified foreign body exposure to LE while riding as a pillion rider. After which he experienced pain, redness and watering in LE. Pain was non-radiating and mild in nature. Patient also gave history of gradual progressive diminution of vision. Patient had visited a nearby clinic and was put on topical medications of which detail was not available with patients but found no relief.
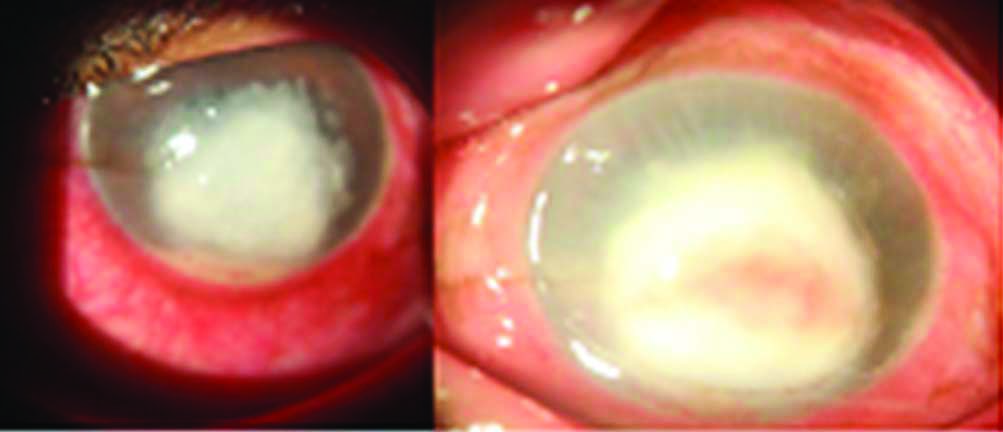
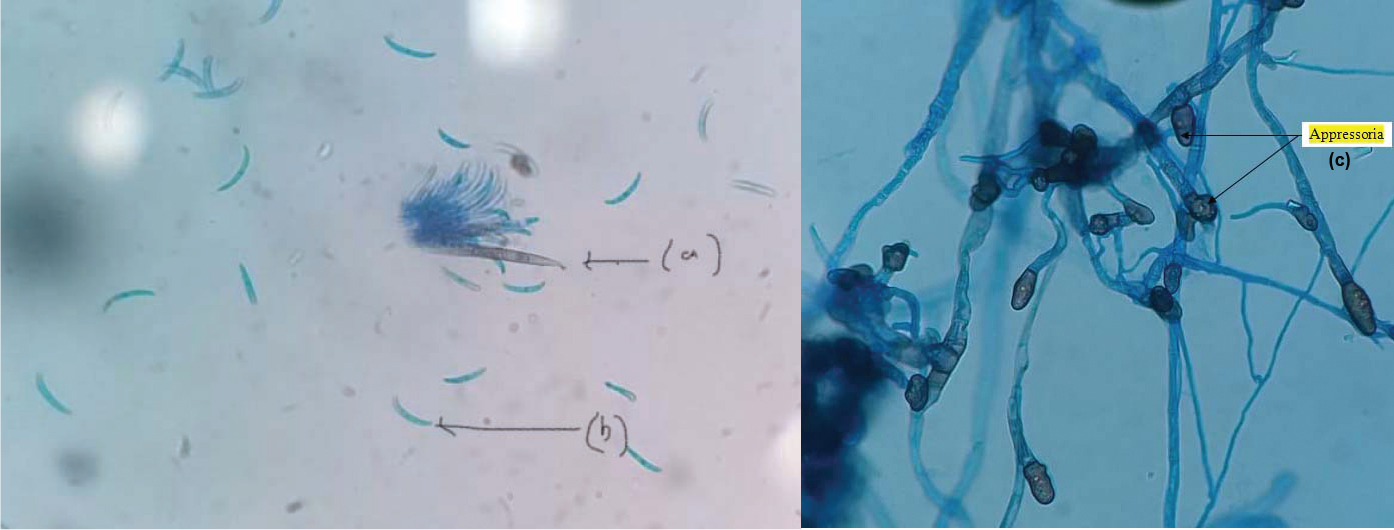
With patients consent, Slit lamp examination with diffused light was performed which revealed a mild lid oedema in his LE with mixed type of congestion, central corneal ulcer with epithelial defect of size 7×7 mm, stromal infiltration of size 8×8 mm, with multiple radiating descemet folds around central ulcer. There was streak hypopyon and intra-stromal bleed at centre with superficial corneal vascularisation at limbus at 360 degrees [Table/Fig-1]. There were no satellite lesions. The details of lens and posterior segment could not be assessed due to hazy view. Visual acuity in patients LE was only hand movement with accurate projection of rays in all four quadrants. Direct pupillary reaction assessed from periphery, found dilated pupil, might be under effects of drugs used by patient. B-scan was found normal with anechoic vitreous cavity. The corneal scraping was obtained with 15 number surgical blade under topical anaesthesia. It was sent for KOH, Gram stain and Fungal culture. KOH mount revealed plenty of hyaline septate hyphae [Table/Fig-2] while Gram stain revealed no organisms. So, the patient was treated with tablet fluconazole 150 mg, 5% natamycin, 1% Atropine eye drops. But there were no signs of improvement after start of treatment. It is cultured on Sabouraud’s Dextrose Agar (SDA) plate and incubated at 27°C. It started with white filamentous growth which turned mouse grey with woolly mycelium. After a week, it turned much darker with dark brown reverse [Table/Fig-3]. Lactophenol Cotton Blue (LPCB) mount of colonies showed septate hyphae and sickle-shaped conidia with acute apex of size 20-30×2.0-3.5 μm. Presence of falciform conidia without septation and presence of brown coloured pear shaped, irregular appressoria (Thick walled swelling at the end of hyphae or germ tube useful for the attachment to the host surface) with setae (thick walled dark pigmented sterile hyphae usually pointed at the tip) were observed [Table/Fig-4a-c]. On the basis of these characteristic morphological features, it was identified as Colletotrichum dematium. The virological seromarkers for HIV and Hepatitis B were within normal limits.
Clinical presentation of patient with whitish large ulcer.
KOH mount showing plenty of thin septate hyphae.

Growth on SDA medium; white filaments which became mouse grey, woolly aerial mycelium and turned felt-like. Reverse was dark brown.

LPCB mount of colonies showing characteristics features of Colletotrichum: a) Setae; b) Fusiform conidia without septations; c) Appressoria (in arrow). LPCB: Lacto phenol cotton blue
After culture confirmation Amphotericin B was added. There was improvement in lesion which was observed till two weeks. Later on, he did not report for further follow-up.
Discussion
Keratitis usually associated with bacterial, fungal, parasitic and viral infection that invades the cornea which leads to destruction of the corneal structures [1]. Comparatively fungal keratitis found to be more virulent and difficult to diagnose and treat. The cause of fungal keratitis is usually associated with history of trauma with some vegetative matter or contaminated soil particles while in the present case the patient was exposed to unidentified foreign body while riding as a pillion rider. Non-traumatic keratitis due to Colletotrichum was also reported [1,2].
There are variations in environmental distribution of fungi geographically, so there is variability in the fungi recovered from keratitis. In developing countries like India, mycotic keratitis comprises up to 40% of the all microbial causes and Aspergillus is the most commonly encountered fungus amongst all other causes [3].
Herewith, reported a case of corneal ulcer due to Colletotrichum which is known to cause plant diseases and rarely can cause human infections. Colletotrichum cases are reported from various parts in world and India, but not from Chhattisgarh [1].
The genus Colletotrichum is a pigmented fungus of coelomycetous group and is a most important plant pathogen causing anthracnosis. They are known to cause keratitis but they can also cause subcutaneous and systemic infection among immunosuppressed patients [4]. There are various species of Colletotrichum but only five have been reported to cause human infections and these are Colletotrichum coccodes, C crassipes, C graminicola, C dematium, C gloeosporioides [2,4-7].
On artificial media, Colletotrichum generally produces filamentous pigmented colonies which are quite similar to colonies of some pheoid fungus such as Alternaria and Curvularia [7]. Key morphological features of Colletotrichum are acervular conidiomata along with setae having elongated conidia and appressoria. C.dematium and C.graminicola both are having sickled-shaped falcate conidia and have to be differentiated from septate conidia of Fusarium species which is frequently encountered fungus causing keratitis. Appressoria of C.dematium are more or less clavate while of C.graminicola are wider and irregular [5].
Patient was having large ulcer with comparatively less pain and history of association with foreign body exposure found to be significant suspicion of fungal keratitis. It is important to identify the species as species-wise disparity was reported in the therapeutic response to anti-fungal agents. Natamycin continues to be the first line treatment in fungal keratitis in the present case Natamycin with fluconazole was started after KOH report [3]. But patient had not responded to it. After culture report, considering it as rare fungi, Amphotericin B was added and patient responded well to the treatment. Though response to Natamycin has been noted in patients but Amphotericin B still remains the first choice for the treatment of this group of infections [6]. Differing statement was reported by Shukla PK et al., regarding Amphotericin B and reported it as less sensitive than Clotrimazole and Micanozole [8].
To do Minimum Inhibition Concentration (MIC) of filamentous fungi is not usual protocol of many laboratories and is performed in special cases only for study purposes [9]. The MIC data from two more studies suggested that Colletotrichum species are well susceptible to Amphotericin B, Itraconazole, Miconazole, Micafungin, Voriconazole, but resistance or high MIC to Natamycin [6,10]. Another study by Serfling A et al., concluded that use of azoles in agricultural field leads to resistant of these agents among plant pathogens [11]. As it is not isolated routinely, its therapy is yet to be standardised. Response to Amphotericin B, Natamycin, Fluconazole, Voriconazole was reported in literature search [8,11-13]. So as it is depicted from some studies that data regarding treatment of Colletotrichum species needs to be evaluated further [12-14]. So, reporting of more and more cases is needed to standardise the specific therapy against the rare fungal diseases.
Limitation(s)
The limitation of this study was that Authors could not perform the MIC of anti-fungal drugs for this Colletotrichum isolate.
Conclusion(s)
To conclude, fungal keratitis due to Colletotrichum dematium may not be rare but is not reported from all parts of India. Reporting of the more cases will help to study the epidemiological distribution and standardisation of therapy for the rare fungal infections.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 01, 2020
Manual Googling: Oct 19, 2020
iThenticate Software: Jan 20, 2021 (7%)
[1]. Mendiratta DK, Thamke D, Shukla AK, Narang P, Keratitis due to Colletotrichum dematium- A case reportIndian J Med Microbiol 2005 23(1):5610.4103/0255-0857.1387615928425 [Google Scholar] [CrossRef] [PubMed]
[2]. Natarajan SV, Rekha NS, Sharda RD, Mahalingam N, Colletotrichum keratitis: A rare but definite clinical entityJ Clin Diagn Res 2013 7(7):1430-33.10.7860/JCDR/2013/5513.315623998083 [Google Scholar] [CrossRef] [PubMed]
[3]. Ansari Z, Miller D, Galor A, Current thoughts in fungal keratitis: diagnosis and treatmentCurr Fungal Infect Rep 2013 7(3):209-18.10.1007/s12281-013-0150-124040467 [Google Scholar] [CrossRef] [PubMed]
[4]. Guarro J, Svidzinski TE, Zaror L, Forjaz MH, Gené J, Fischman O, Subcutaneous Hyalohyphomycosis Caused by Colletotrichum gloeosporioidesJ Clin Microbiol 1998 36(10):3060-65.10.1128/JCM.36.10.3060-3065.19989738070 [Google Scholar] [CrossRef] [PubMed]
[5]. Cano J, Guarro J, Gené J, Molecular and morphological identification of colletotrichum species of clinical interestJ Clin Microbiol 2004 42(6):2450-54.10.1128/JCM.42.6.2450-2454.200415184418 [Google Scholar] [CrossRef] [PubMed]
[6]. Kotwal A, Biswas D, Kakati B, Bahadur H, Gupta N, Non traumatic keratitis due to colletotrichum coccodes: A case reportJ Clin Diagn Res 2015 9(2):DD01-02.10.7860/JCDR/2015/10843.552925859457 [Google Scholar] [CrossRef] [PubMed]
[7]. Yamamoto N, Matsumoto T, Ishibashi Y, Fungal keratitis caused by Colletotrichum gloeosporioidesCornea 2001 20(8):902-03.10.1097/00003226-200111000-0002711685077 [Google Scholar] [CrossRef] [PubMed]
[8]. Shukla PK, Kumar M, Keshava GB, Mycotic keratitis: an overview of diagnosis and therapyMycoses 2008 51(3):183-99.10.1111/j.1439-0507.2007.01480.x18399899 [Google Scholar] [CrossRef] [PubMed]
[9]. Reiss, Errol fundamental medical mycology/Errol Reiss, H.Jean Shadomy, and G.Marshall Lyon III 2012 New JerseyWiley-Blckwell10.1002/9781118101773 [Google Scholar] [CrossRef]
[10]. Fernandez V, Dursun D, Miller D, Alfonso EC, Colletotrichum keratitisAm J Ophthalmol 2002 134(3):435-38.10.1016/S0002-9394(02)01576-3 [Google Scholar] [CrossRef]
[11]. Serfling A, Wohlrab J, Deising HB, Treatment of a Clinically relevant plant-pathogenic fungus with an agricultural azole causes cross-resistance to medical azoles and potentiates caspofungin efficacyAntimicrob Agents Chemother 2007 51(10):3672-76.10.1128/AAC.00654-0717620378 [Google Scholar] [CrossRef] [PubMed]
[12]. Buchta V, Nekolová J, Jirásková N, Bolehovská R, Wipler J, Hubka V, Fungal Keratitis caused by colletotrichum dematium: Case study and reviewMycopathologia 2019 184(3):441-53.10.1007/s11046-019-00335-w30949880 [Google Scholar] [CrossRef] [PubMed]
[13]. Giaconi JA, Marangon FB, Miller D, Alfonso EC, Voriconazole and fungal keratitis: A report of two treatment failuresJ Ocul Pharmacol Ther 2006 22(6):437-39.10.1089/jop.2006.22.43717238810 [Google Scholar] [CrossRef] [PubMed]
[14]. Squissato V, Yucel YH, Richardson SE, Alkhotani A, Wong DT, Nijhawan N, Colletotrichum truncatum species complex: Treatment considerations and review of the literature for an unusual pathogen causing fungal keratitis and endophthalmitisMed Mycol Case Rep 2015 9:01-06.10.1016/j.mmcr.2015.06.00126137437 [Google Scholar] [CrossRef] [PubMed]