Study of Prevalence of Neuropsychiatric Symptoms in Elderly Dementia Patients
Mohan Mahale1, Pradeep Behal2, Nitul M Bewal2, Vivek Aggarwal3, Anuj Singhal4, Arun Kumar Yadav5, Vivek Vasdev6
1 Assistant Professor, Department of Internal Medicine, 158 Base Hospital, Bagdogra, West Bengal, India.
2 Assistant Professor, Department of Geriatrics, Armed Forces Medical College, Pune, Maharashtra, India.
3 Assistant Professor, Department of Internal Medicine, Armed Forces Medical College, Pune, Maharashtra, India.
4 Associate Professor, Department of Geriatrics, Armed Forces Medical College, Pune, Maharashtra, India.
5 Professor, Department of Internal Medicine, Armed Forces Medical College, Pune, Maharashtra, India.
6 Associate Professor, Department of Community Medicine, Armed Forces Medical College, Pune, Maharashtra, India.
7 Professor and Head, Department of Geriatrics, Armed Forces Medical College, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Anuj Singhal, Professor, Department of Internal Medicine, Armed Forces Medical College, Pune, Maharashtra, India.
E-mail: purnimanuj@gmail.com
Introduction
Prevalence of dementia is increasing with rapidly ageing population. Neuropsychiatric Symptoms (NPS) are common in certain types of dementia and increases with duration of dementia in Alzheimer’s disease and are causes significant psychosocial and management issues.
Aim
To study the prevalence and type of NPS in patients of dementia presenting to a Tertiary Care Hospital and to find out the association between NPS and the type of dementia and to assess the association of the caregiver stress in this setting.
Materials and Methods
The present cross-sectional observational study was conducted at Tertiary Care Government Hospital of Western Maharashtra. All patients with suspected dementia were initially screened by a Mini-Cog questionnaire and patients with a score of three or less were assessed with Hindi Mental Status Examination (HMSE). The inclusion criteria were patients with HMSE of less than or equal to 23. All the diagnosed patients with dementia were screened for common psychiatric symptoms using Neuropsychiatric Inventory (NPI). The presence of NPS was noted based on either presenting complaint of the patient or as per the history given by the primary caregiver for these symptoms in last one month. These questions were administered in focused group discussion form to the primary caregiver by the physician. The data was collected and analysed using descriptive statistics and Chi-square test with SSPS 20.0.
Results
The most common neuropsychiatric manifestation was sleep and night-time behavioural disorder (51.5%). It was followed by depression (44%). Neuropsychiatric manifestations were much more common in demented patients of probable Dementia with Lewy Bodies (DLB) and dementia with B12 deficiency. More than 50% of the patients had two or more psychiatric symptoms. The most common psychiatric symptom in patients with probable Alzheimer’s disease was sleep and night-time disturbance in 54.9%. Common neuropsychiatric manifestations seen in DLB were visual hallucinations (100%), followed by irritability (88%). More than 90% of the caregivers were not aware of the psychiatric manifestations of dementia and did not know how to cope up with these symptoms.
Conclusion
NPS were more common in patients with DLB dementia and dementia with B12 deficiency, with depression been more common symptom in patients with Parkinson’s related dementia. It is therefore, very important to look for NPS in all elderly patients which can help us to diagnose dementia earlier.
Caregiver burden, Dementia, Hindi mental status examination, Neuropsychiatric inventory
Introduction
Dementia is a common problem in the elderly and the prevalence is on the rise with rapidly aging population [1]. With a rapidly aging population number of dementia patients is increasing and is a major cause of morbidity in the elderly. NPS in dementia patients is a common occurrence and difficult to manage leading to increase in the care giver stress [2]. This may lead to elderly abuse and to early institutionalisation of these dementia patients [3].
Early NPS like apathy, irritability and depression may be common in early dementia but are often missed [4]. Early identification of these NPS is extremely important to diagnose dementia at an earlier stage so as to either slow or retard the progression if possible and educate the family about the likely course of the disease. This will reduce the caregiver burden and improve quality of life of a patient as well the caregiver.
Awareness and education of the caregiver on common psychiatric symptoms and various methods to deal with them is very poor. A study done from India showed that prevalence of NPS in dementia patients were high and were noted in 70% of the elderly patients [5]. However, data from India is very scarce and may vary from place to place. Hence, recognising them early and treating and addressing them appropriately will help to spread the awareness of these symptoms and reduce the caregiver stress and improve the quality of care in these patients.
This study was aimed to study prevalence and type of NPS in the elderly patients with dementia presenting a tertiary care hospital of Western Maharashtra. The secondary objectives were to find out the association between NPS and the type of dementia and to assess the association of the caregiver stress in this setting.
Materials and Methods
It was a cross-sectional observational study done from September 2015 to August 2019 at Tertiary Care Government Hospital of Western Maharashtra. Institutional ethical clearance letter number IEC/2020/164, AFMC Pune was taken. The sample size was calculated assuming the prevalence of NPS in dementia as 75% and absolute precision of 6% with 95% Confidence interval [6]. The calculated sample size was 200.
Inclusion Criteria and Exclusion Criteria
The inclusion criteria were elderly OPD patients, aged more than 60 years of age with dementia (HMSE of less than or equal to 23). The exclusion criteria were patients with suspected delirium (fever of more than 100°F), dyselectrolytemia, suspected pneumonia or urinary tract infection, alcohol withdrawal/dependence) and known thyroid disorder.
All patients with suspected dementia were initially screened by a Mini-Cog questionnaire and patients with a Mini-Cog of three or less than three were assessed with HMSE [7,8]. All the diagnosed patients with dementia were screened for common psychiatric symptoms using NPI, which included depression, hallucinations, delusions, agitation, anxiety, apathy, euphoria, irritability, sleep and night time disturbance and disinhibition [9]. The presence of NPS was noted based on either presenting complaint of the patient or as per the history given by the primary caregiver for these symptoms in last one month. These questions were administered in focused group discussion form to the primary caregiver by the physician.
Dementia types were segregated based on history and clinical examination. Alzheimer’s and vascular dementias were segregated based on Hachinski’s score and neuroimaging [10].
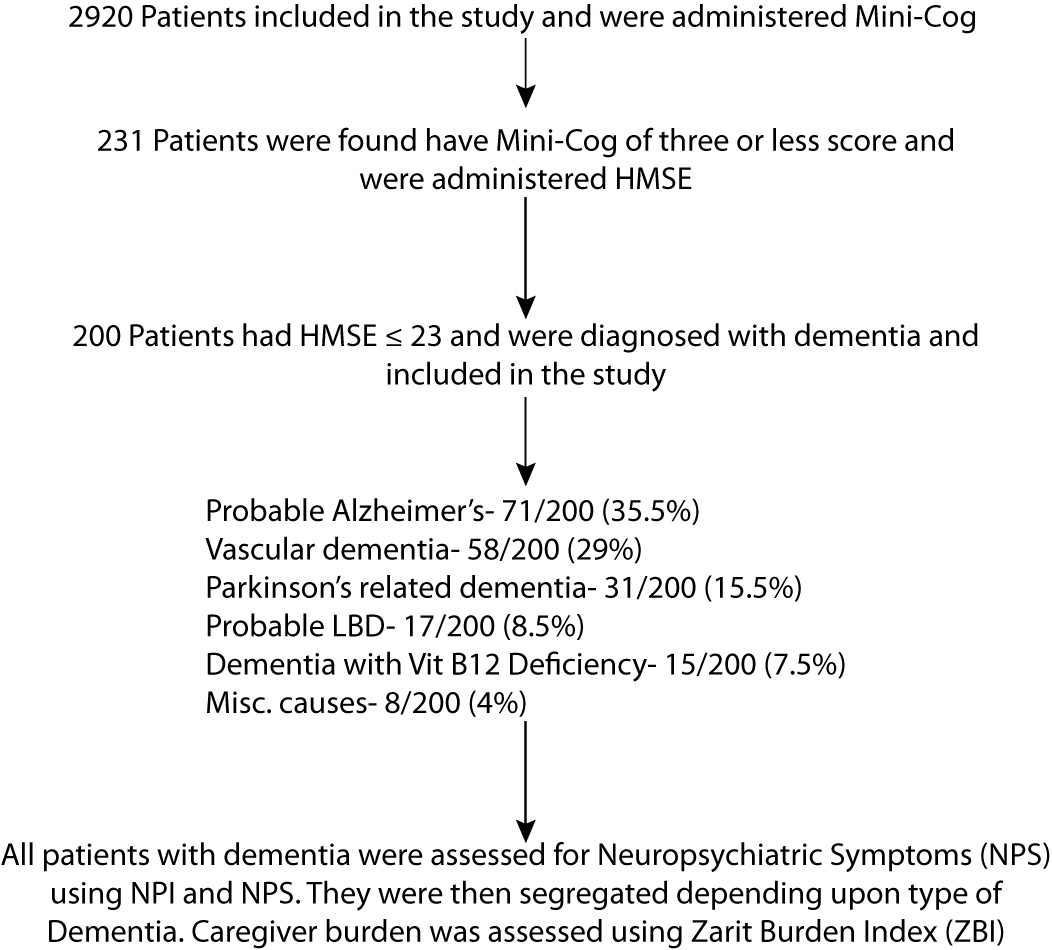
Probable cause of dementia was based on the history, neuroimaging and specific investigations which included ELISA for HIV, vitamin B12 levels by ELISA, thyroid functions tests by ELISA and syphilis serology by Veneral Disease Research Laboratory (VDRL) test. All the caregivers were educated about the common neuropsychiatric manifestations of dementia and the ways to cop up with these symptoms. Caregiver stress was assessed by Zarit Burden Index (ZBI) [11]. The detailed flow chart of inclusion criteria and assessment is mentioned in [Table/Fig-1].
Detailed data assessment flow chart.
Statistical Analysis
The data was noted and tabulated as frequency and percentages. Chi-square test was used to analyse data using SSPS 20.
Results
Total 200 patients were diagnosed with dementia. All these patients were then screened for presence of NPS. Mean age of patients was 71 years and mean duration of symptoms of dementia was 39.2 months. All patients were more than 60 years of age, with maximum being in the 60-80 year age category (81%). Only 19% were older than 80 years. The differences between the age groups were not significant (p-0.503 by Chi-square test) [Table/Fig-2].
Age distribution of the elderly patients with dementia.
| Age (years) | Frequency | Alzeihmer’s disease n=71 | Vascular disease n=58 | Lewy body dementia n=17 | Dementia with B12 deficiency n=15 | Parkinson’s related dementia n=31 | Miscellneous n=8 |
|---|
| 60-69 | 87 | 30 | 29 | 3 | 6 | 18 | 1 |
| 70-79 | 75 | 26 | 22 | 8 | 8 | 6 | 5 |
| >80 | 38 | 15 | 7 | 6 | 1 | 7 | 2 |
NPS were observed in 84% of the patients of dementia. The most common neuropsychiatric manifestation was sleep and night time behavioural disorder (51.5%) followed by depression (44%). Neuropsychiatric manifestations were much more common in demented patients of probable DLB and dementia with B12 deficiency. More than 50% of the patients had two or more psychiatric symptoms.
The most common psychiatric symptom in patients with probable Alzheimer’s disease was sleep and night time disturbance in 54.9% followed by depression in 49.3%. Common neuropsychiatric manifestations seen in DLB were visual hallucinations (100%), in B12 deficiency dementia was sleep disturbance and in Parkinson’s related dementia it was depression. The details of disease wise NPS in common diseases are tabulated in [Table/Fig-3].
Neuropsychiatric manifestation in different types of dementia.
| Signs | Frequency | Alzheimer disease (n=71) | Vascular disease (n=58) | Parkinson’s related dementia (n=31) | Lewy body dementia (n=17) | B12 deficiency dementia (n=15) | Miscellneous Causes (n=8) | p-value |
|---|
| Hallucinations | 21 (10.5%) | 1 (1.4%) | 0 | 1 (3.22%) | 17 (100%) | 2 (13.3%) | 0 | <0.001 |
| Delusions | 23 (11.5%) | 3 (4.2%) | 0 | 2 (6.4%) | 14 (82.4%) | 2 (13.3%) | 2 (25%) | <0.001 |
| Agitation | 34 (17%) | 10 (14.1%) | 3 (5.2%) | 2 (6.4%) | 13 (76.5%) | 3 (20%) | 3 (37.5%) | <0.001 |
| Depression | 88 (44%) | 35 (49.3%) | 25 (43.1%) | 21 (67.74%) | 5 (29.4%) | 1 (6.7%) | 1 (12.5%) | 0.002 |
| Anxiety | 37 (18.5%) | 9 (12.7%) | 13 (22.4%) | 5 (16.12%) | 6 (35.3%) | 4 (26.7%) | 0 | 0.158 |
| Apathy | 53 (26.5%) | 18 (25.4%) | 16 (27.6%) | 10 (32.25%) | 4 (23.5%) | 2 (13.3%) | 3 (37.5%) | 0.773 |
| Irritability | 70 (35%) | 23 (32.4%) | 14 (24.1%) | 12 (38.70%) | 15 (88.2%) | 4 (26.7%) | 1 (12.5%) | <0.001 |
| Sleep/Night time disturbances | 103 (51.5%) | 39 (54.9%) | 17 (29.3%) | 20 (64.51%) | 17 (100%) | 9 (60%) | 2 (25%) | <0.001 |
| Motor symptoms | 55 (27.5%) | 2 (2.8%) | 26 (44.8%) | 13 (41.93%) | 10 (76.5%) | 2 (13.3%) | 1 (12.5%) | <0.001 |
| Disinhibition | 26 (13%) | 3 (4.2%) | 0 | 2 (6.4%) | 16 (94.1%) | 2 (13.3%) | 3 (37.5%) | <0.001 |
| Euphoria | 16 (8%) | 2 (2.8%) | 0 | 2 (6.4%) | 7 (41.2%) | 3 (20%) | 1 (12.5%) | <0.001 |
p<0.001 is considered as statistically significant
It was also noted that caregiver stress was significantly higher in patients with two or more psychotic symptoms especially in patients with DLB where hallucinations and delusions were very common as measured by ZBI. Mean age of the caregivers was 47 (SD 12.21) years with 55% (110/200) being females and 45% (90/200) being males. Spouse was a primary caregiver in 55% (110/200) of the dementia patients. Caregiver burden increased with duration and severity of dementia. More than 90% (182/200) of the caregivers were not aware of the psychiatric manifestations of dementia and did not know how to cope up with these symptoms. It was also noted that 54% (108/200) of the caregivers had a ZBI of more than 60 which was suggestive of severe caregiver stress and 42.5% (85/200) of caregivers had a ZBI score between 40 and 60 suggestive of moderate to severe caregiver stress. Thus, more than 90% of the caregivers of dementia had moderate to severe caregiver stress [Table/Fig-4].
Severity of caregiver stress in various types of dementia.
| Severity of ZBI and type of dementia correlation | Type of dementia |
|---|
| Zarit burden index | Alzheimer disease | Vascular disease | Lewy body dementia | Dementia with B12 Def | Parkinson’s related dementia | Misc (NPH, FTH) | Total | p-value |
|---|
| 21-40 | 5 | 3 | 0 | 0 | 1 | 0 | 9 | 0.036 |
| 41-60 | 38 | 23 | 1 | 7 | 11 | 3 | 83 |
| >60 | 28 | 32 | 16 | 8 | 19 | 5 | 108 |
| Total | 71 | 58 | 17 | 15 | 31 | 8 | 200 |
Discussion
Primary objective of the study was to assess the prevalence and types of NPSs in elderly patients with dementia. It was noted that NPSs were common and are associated with increased caregiver burden in dementia patients. NPSs were seen in almost all types of dementia especially during the course of the disease progression [12]. In a study done by Lyketsos C in 2002, it was seen that almost 75% of the patients with dementia had atleast one and 55% had atleast two NPSs in the last one month as assessed by caregiver’s interview [13]. This is consistent with this study which shows the prevalence of NPS with atleast one psychiatric symptom in 84% and two psychiatric symptoms in more than half of the patients. Similar findings were also noted in a Canadian study done in elderly patients attending dementia clinics, where prevalence of NPSs was 89% [14].
Studies have shown that neuropsychiatric manifestations like apathy, irritability and depression can be an early symptom of Minimal Cognitive Impairment (MCI) before development of dementia and are often missed [15]. The risk of MCI with NPSs converting to dementia is around 25% per year [16]. This rapid increase in number of NPS in patients with MCI and dementia has led to a birth of new subspeciality called as Geriatric psychiatry which is an evolving field and is rapidly spreading its wings. It is important to recognise these NPS early so that dementia could be unmasked early and adequate measures to assess the probable cause of cognitive decline can be taken and reversible causes if any can be reversed. Even if dementia is irreversible or degenerative it is important to treat the risk factors, encourage mental exercises with cognitive stimulation to slow the progression of disease. In this study, depression was seen in 44% of patients with maximum prevalence of dementia in Parkinson’s related dementia (67.7%) followed by Alzheimer’s disease. Similar findings were noted in a study done by Ravina B et al., where depressive symptoms were present in around 50% of the patients with Parkinson’s disease. Depression in patients with Parkinson’s disease may even precede the onset of motor symptoms by a decade [17]. Depression in Parkinson’s disease is often missed and undertreated as it is frequently underestimated due to general appearance of the patient with Parkinson’s disease. Depression and dementia both go hand in hand as depression may lead to cognitive impairment (pseudo dementia) and demented patients are also at an increased risk of developing depression especially in AD [18]. It was seen that the prevalence of depression in DLB was 29% which is less than a published study where depression was seen in 50% of patients with DLB [19]. This may be due to underestimation of depression due to presence of psychotic symptoms, prominent hallucination/delusions compounded with early cognitive decline.
According to the studies, Alzheimer’s disease is associated with very high prevalence of psychiatric symptoms and around 80% of the patients may have psychiatric symptoms [20]. In a study done by Mega MS et al., in USA, the common NPS in patients with Alzheimer’s disease were apathy in 72% followed by anxiety in 60% [21]. In this study, the most common psychiatric manifestation in patients with probable Alzheimer’s disease was sleep and night time disturbance followed by depression. Apathy and anxiety was seen in only one fourth of the patients which is much less than the studies done in developed countries [22]. Irritability and motor symptoms were more common in dementia related to Parkinson’s disease and Parkinson’s plus syndromes like DLB whereas anxiety was more common in DLB. Agitation and disinhibition were also more common in DLB. Thus, NPS were commonly seen in this study which was the main cause of caregiver burden.
Limitation(s)
Mixed dementia was not categorised separately and cognitive decline due to depression was not assessed. Another limitation was that it is a hospital-based study and it tends to overestimate NPS in dementia patients as patients of dementia with NPS are more likely to visit a hospital. A community-based study will be more desirable to assess the exact prevalence of NPS in dementia patients.
Conclusion(s)
It was seen in this study that NPS were common in dementia patients and was associated with increased caregiver stress. NPS were more common in patients with DLB dementia and dementia with B12 deficiency, and depression been more common symptom in patients with Parkinson’s related dementia.
p<0.001 is considered as statistically significant
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 27, 2020
Manual Googling: Jan 01, 2021
iThenticate Software: Jan 12, 2021 (6%)
[1]. Brayne C, Miller B, Dementia and aging populations—A global priority for contextualized research and health policyPLOS Medicine 2017 14(3):e100227510.1371/journal.pmed.100227528350794 [Google Scholar] [CrossRef] [PubMed]
[2]. Chen P, Guarino PD, Dysken MW, Pallaki M, Asthana S, Llorente MD, Neuropsychiatric symptoms and caregiver burden in individuals with Alzheimer’s Disease: The TEAM-AD VA cooperative studyJ Geriatr Psychiatry Neurol 2018 31(4):177-85.10.1177/089198871878389729966477 [Google Scholar] [CrossRef] [PubMed]
[3]. Cooper C, Livingston G, Mental Health/Psychiatric issues in elder abuse and neglectClin Geriatr Med 2014 30(4):839-50.10.1016/j.cger.2014.08.01125439645 [Google Scholar] [CrossRef] [PubMed]
[4]. Lanctôt KL, Amatniek J, Ancoli-Israel S, Arnold SE, Ballard C, Cohen-Mansfield J, Neuropsychiatric signs and symptoms of Alzheimer’s disease: New treatment paradigmsAlzheimers Dement (N Y) 2017 3(3):440-49.10.1016/j.trci.2017.07.00129067350 [Google Scholar] [CrossRef] [PubMed]
[5]. Das S, Pal S, Ghosal M, Dementia: Indian scenarioNeurology India 2012 60(6):618-24.10.4103/0028-3886.10519723287325 [Google Scholar] [CrossRef] [PubMed]
[6]. Lyketsos CG, Lopez O, Jones B, Fitzpatrick AL, Breitner J, DeKosky S, Prevalence of neuropsychiatric symptoms in dementia and mild cognitive impairment: Results from the cardiovascular health studyJAMA 2002 288(12):1475-83.10.1001/jama.288.12.147512243634 [Google Scholar] [CrossRef] [PubMed]
[7]. Borson S, Scanlan JM, Chen P, Ganguli M, The Mini-Cog as a screen for dementia: Validation in a population-based sampleJ Am Geriatr Soc 2003 51(10):1451-54.10.1046/j.1532-5415.2003.51465.x14511167 [Google Scholar] [CrossRef] [PubMed]
[8]. Tsolaki M, Iakovidou V, Navrozidou H, Aminta M, Pantazi T, Kazis A, Hindi Mental State Examination (HMSE) as a screening test for illiterate demented patientsInt J Geriatr Psychiatry 2000 15(7):662-64.10.1002/1099-1166(200007)15:7<662::AID-GPS171>3.0.CO;2-5 [Google Scholar] [CrossRef]
[9]. Cummings JL, Mega M, Gray K, Rosenberg-Thompson S, Carusi DA, Gornbein J, The Neuropsychiatric Inventory: comprehensive assessment of psychopathology in dementiaNeurology 1994 44(12):2308-14.10.1212/WNL.44.12.23087991117 [Google Scholar] [CrossRef] [PubMed]
[10]. Kim YH, Kwon OD, Clinical correlates of hachinski ischemic score and vascular factors in cognitive function of elderlyBiomed Res Int 2014 2014:85278410.1155/2014/85278425247189 [Google Scholar] [CrossRef] [PubMed]
[11]. Zarit SH, Reever KE, Bach-Peterson J, Relatives of the impaired elderly: Correlates of feelings of burdenThe Gerontologist 1980 20(6):649-55.10.1093/geront/20.6.6497203086 [Google Scholar] [CrossRef] [PubMed]
[12]. Peters KR, Rockwood K, Black SE, Bouchard R, Gauthier S, Hogan D, Characterizing neuropsychiatric symptoms in subjects referred to dementia clinicsNeurology 2006 66(4):523-28.10.1212/01.wnl.0000198255.84842.0616505306 [Google Scholar] [CrossRef] [PubMed]
[13]. Lyketsos C, Neuropsychiatric Symptoms in Dementia: Overview and Measurement ChallengesThe Journal of Prevention of Alzheimer’s Disease 2015 2(3):155-56. [Google Scholar]
[14]. Geda YE, Roberts RO, Knopman DS, Petersen RC, Christianson TJ, Pankratz VS, Prevalence of neuropsychiatric symptoms in mild cognitive impairment and normal cognitive aging: Population-based studyArch Gen Psychiatry 2008 65(10):1193-98.10.1001/archpsyc.65.10.119318838636 [Google Scholar] [CrossRef] [PubMed]
[15]. Iaboni A, Rapoport MJ, Detecting and managing neuropsychiatric symptoms in dementia: What psychiatrists need to know and whyCan J Psychiatry 2017 62(3):158-60.10.1177/070674371667240928212493 [Google Scholar] [CrossRef] [PubMed]
[16]. Ravina B, Camicioli R, Como PG, Marsh L, Jankovic J, Weintraub D, The impact of depressive symptoms in early Parkinson diseaseNeurology 2007 69(4):342-47.10.1212/01.wnl.0000268695.63392.1017581943 [Google Scholar] [CrossRef] [PubMed]
[17]. Kehagia AA, Neuropsychiatric symptoms in Parkinson’s Disease: Beyond complications. Frontiers in PsychiatryFront Psychiatry 2016 7:11010.3389/fpsyt.2016.0011027445867 [Google Scholar] [CrossRef] [PubMed]
[18]. Dal Forno G, Palermo MT, Donohue JE, Karagiozis H, Zonderman AB, Kawas CH, Depressive symptoms, sex, and risk for Alzheimer’s diseaseAnn Neurol 2005 57(3):381-87.10.1002/ana.2040515732103 [Google Scholar] [CrossRef] [PubMed]
[19]. Klatka LA, Louis ED, Schiffer RB, Psychiatric features in diffuse Lewy body disease: A clinicopathologic study using Alzheimer’s disease and Parkinson’s disease comparison groupsNeurology 1996 47(5):1148-52.10.1212/WNL.47.5.11488909420 [Google Scholar] [CrossRef] [PubMed]
[20]. Lyketsos CG, Carrillo MC, Ryan JM, Khachaturian AS, Trzepacz P, Amatniek J, Neuropsychiatric symptoms in Alzheimer’s diseaseAlzheimer’s & dementia : The journal of the Alzheimer’s Association 2011 7(5):532-39.10.1016/j.jalz.2011.05.241021889116 [Google Scholar] [CrossRef] [PubMed]
[21]. Mega MS, Cummings JL, Fiorello T, Gornbein J, The spectrum of behavioural changes in Alzheimer’s diseaseNeurology 1996 46(1):130-35.10.1212/WNL.46.1.1308559361 [Google Scholar] [CrossRef] [PubMed]
[22]. Nobis L, Husain M, Apathy in Alzheimer’s diseaseCurr Opin Behav Sci 2018 22:07-13.10.1016/j.cobeha.2017.12.00730123816 [Google Scholar] [CrossRef] [PubMed]