Effects of Different Doses of Dexmedetomidine on Intraocular Pressure after Suxamethonium in Non-ocular Surgeries: A Randomised Controlled Trial
Saswati Das1, Mousumi Das2, Lingaraj Sahu3, Gayatree Mohanty4, Akshya Kumar Parida5
1 Assistant Professor, Department of Anaesthesia, Kalinga Institute of Medical Sciences, Bhubaneswar, Odisha, India.
2 Assistant Professor, Department of Anaesthesia, Kalinga Institute of Medical Sciences, Bhubaneswar, Odisha, India.
3 Associate Professor, Department of Anaesthesia, Kalinga Institute of Medical Sciences, Bhubaneswar, Odisha, India.
4 Assistant Professor, Department of Ophthalmology, Kalinga Institute of Medical Sciences, Bhubaneswar, Odisha, India.
5 Professor, Department of Anaesthesia, Kalinga Institute of Medical Sciences, Kalarahanga, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Lingaraj Sahu, Associate Professor, Department of Anaesthesia, KIIT University, Bubaneswar-751024, Odisha, India.
E-mail: drlingarajsahu.2008@gmail.com
Introduction
Succinylcholine causes a rise in Intraocular Pressure (IOP) and is deleterious in patients with open globe injuries. Dexmedetomidine, by its virtue of central sympatholytic action can help prevent this rise in IOP.
Aim
To find out the optimal dose of Dexmedetomidine in preventing the rise of IOP after administration of Suxamethonium.
Materials and Methods
One hundred American Society of Anesthesiologists (ASA) I or II patients posted for non-ophthalmic surgery were included in this randomised, prospective, double blind study. Patients were randomly allocated to four groups. Group A (n=25) received Dexmedetomidine 0.6 μg/kg, Group B (n=25) received Dexmedetomidine 0.8 μg/kg, Group C (n=25) received Dexmedetomidine 1 μg/kg, Group D (n=25) received Normal Saline (NS) over a period of 10 minutes and IOP was measured at different points in time.
Results
Premedication with Dexmedetomidine at doses of 0.6 μg/kg, 0.8 μg/kg and 1 μg/kg intravenous (IV) were equally effective in attenuation of the rise in IOP associated with Succinylcholine administration. The IOP recorded was 15.53±1.10 mm of Hg in Group A, 14.49±0.94 mm of Hg in Group B, 14.72±1.03 mm of Hg in Group C as compared to 20.12±1.40 mm of Hg in the control group (Group D) after 60 seconds of injecting Suxamethonium. It also significantly obtunded the sympathetic response to laryngoscopy and intubation. However, the incidence of side effects increased with incremental doses.
Conclusion
Dexmedetomidine 0.6 μg/kg IV premedication is the optimum dose to be used for attenuating the rise in IOP associated with Succinylcholine administration in situations where rise of IOP may be detrimental.
Elective surgery, Open globe injury, Rapid sequence intubation
Introduction
Control of IOP within the physiological range is necessary to maintain the anatomy of the eye for optimal vision. It normally varies between 10 and 21.7 mmHg and is considered abnormal above 22 mmHg [1,2]. IOP is increased by laryngoscopy and intubation [3]. Sympathetic stimulation accompanying laryngoscopy and intubation causes adrenergic stimulation leading to vasoconstriction and increased central venous pressure, both of which are closely associated with elevation of IOP. Sympathetic surge may also cause a decrease in outflow of aqueous humor by increasing the resistance in the trabecular mesh work between anterior chamber and canal of Schlemn. This in turn causes an acute increase in IOP. Thus, there is a close relationship between haemodynamic response and IOP. This explains the role of pretreatment for stress attenuation during laryngoscopy and intubation which may help to blunt the rise of IOP [2,4].
Suxamethonium, a depolarising muscle relaxant is used widely as it provides rapid and excellent intubating conditions. It is preferred in patients with full stomach and anticipated difficult airway. However, it causes 25-30% increase in IOP [4] which lasts for 5-10 minutes [4,5]. This rise in IOP may be critical in patients with acute glaucoma, impending perforation of the eye and perforating eye injuries. Rise in IOP can cause retinal artery occlusion or retinal ischemia [3,4]. In an open eye injury, this increase can lead to loss of intraocular contents, haemorrhage, and permanent vision loss. Dexmedetomidine, the pharmacologically active d-isomer of Medetomidine, is a highly selective and specific alpha-2 adrenoceptor agonist. The effect of dexmedetomidine on the IOP may be due to its direct vasoconstrictor effect on the afferent blood vessels of the ciliary body leading to a reduction of aqueous humor production. It may also facilitate the drainage of aqueous humor by reducing sympathetically mediated vasomotor tone of the ocular drainage system. Dexmedetomidine, by its central sympatholytic action, promotes haemodynamic stability which also contributes to the reduction of IOP [6,7]. Half life of dexmedetomidine is of approximately six minutes [6], so it can be used successfully for attenuating the response to succinylcholine administration, laryngoscopy and intubation.
Though many studies have been done taking different doses of dexmedetomidine and its effect on IOP, none of them have compared more than two doses [8,9]. So, the primary objective of the present study was to assess the optimum dose of dexmedetomidine that prevents rise of IOP caused due to suxamethonium, with minimal side-effects.
Materials and Methods
The present study was a randomised double-blind study which was conducted after the approval from the Institutional Ethics Committee (KIMS/KIIT/IEC/65/2018). One hundred patients consenting to participate were included. The study was registered with Clinical Trials Registry- India (CTRI): CTRI/2018/07/0148. This study was conducted in Kalinga Institute of Medical Sciences, Bhubaneswar, Odisha, India from November 2018 to August 2020.
By adopting the reported IOP measurements associated with different doses [10], i.e., 16.9, 17.04, 18.75 and within group variance of 3.28 at 1% level of significance and 80% of the minimum power of study, the required sample size is 24 in each group. Therefore, 100 subjects were randomised into four groups in the study. Patients aged 18-60 years with ASA Physical Status (PS) class I or II, with normal IOP posted for non-ophthalmic surgery under general anaesthesia were included in the study.
Patients with anticipated difficult airway, psychiatric disorders, acute or chronic eye diseases, with raised intracranial pressure, receiving any drug known to alter IOP, pregnant or lactating patients or hypertensive patients receiving any antihypertensive drugs were excluded. During the process, patients requiring prolonged laryngoscopy and more than one attempt to intubation were also excluded from the study.
Randomisation was done using computer software research randomiser and patients were allocated to four different groups [Table/Fig-1]:
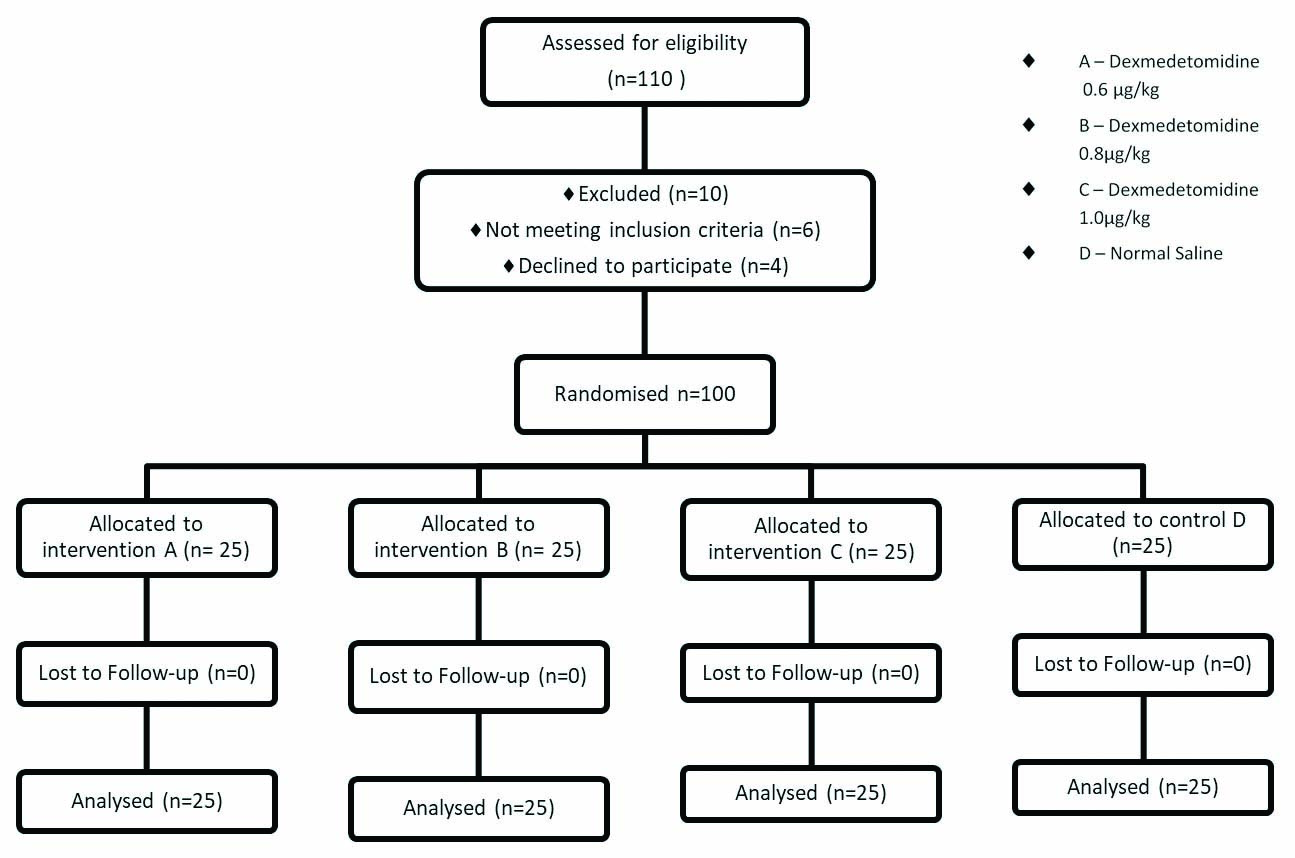
Group A (n=25) received dexmedetomidine 0.6 μg/kg
Group B (n=25) received dexmedetomidine 0.8 μg/kg
Group C (n=25) received dexmedetomidine 1 μg/kg
Group D (n=25) received NS
As per the randomisation list, either 0.6 μg/kg or 0.8 μg/kg or 1 μg/kg injection dexmedetomidine was diluted to 20 mL with NS or 20 mL of NS only (placebo) were prepared by a resident doctor who was not a part of the study. After shifting to OT, monitors were attached and the prepared solution was started using syringe pump. The solution was infused intravenous (IV) over 10 minutes. IV fluids was started with Ringer Lactate (RL) solution at the rate of 4 mL/kg/hr simultaneously. Monitoring included three lead ECG, pulse oximetry, capnography and non-invasive blood pressure. Patients were premedicated with Inj. nalbuphine 0.1 mg/kg IV. After pre-oxygenation for three minutes patients were induced with injection propofol 2 mg/kg and succinylcholine 1.5 mg/kg IV. After cessation of fasciculations, laryngoscopy followed by intubation was done. Maintenance of anaesthesia was done with isoflurane and injection vecuronium. IOP was measured using Schiotz tonometer by an ophthalmologist at different points in time. To avoid the diurnal variation associated with the changes in IOP, all the surgeries that were taken for the study were posted in the morning. Systemic side-effects like bradycardia and hypotension were treated with either atropine or ephedrine respectively. In case of unresponsive bradycardia and/or hypotension the solution was stopped and the patients were dropped from the study.
The IOP were measured as:
T1: baseline on Operation Theatre (OT) table (after topical 4% lignocaine instillation to cornea).
T2: just after pre-medication.
T3: just after propofol injection
T4: 60 seconds after suxamethonium.
T5: immediately after intubation.
T6-15: every 1 min up to 10th minute after intubation.
Statistical Analysis
Data were collected, tabulated, coded in MS excel sheet and the statistical analysis was carried out using standard statistical software Statistical Package for the Social Sciences (SPSS) 22.0. All the qualitative parameters were represented as frequency and percentage whereas continuous parameter will be reported as mean±standard deviation. As regard to continuous variables; student’s t-test was used. One-way ANOVA was used to find out association between two categorical variables. The p-value was considered as significant if <0.05 and highly significant if <0.001.
Results
There were no significant differences (p>0.05) among the groups regarding age, weight, duration of laryngoscopy and the preoperative IOP [Table/Fig-2].
| Variables | Group A | Group B | Group C | Group D | p-value (One-way ANOVA) |
|---|
| Age (years) (mean±SD) | 47.2±12.42 | 45.68±14.31 | 40.48±13.17 | 48.24±12.10 | 0.162 |
| Weight (kg) (mean±SD) | 63.68±7.56 | 62.08±8.12 | 58.8±11.77 | 64.28±7.41 | 0.134 |
| Duration of laryngoscopy (sec.) (Mean±SD) | 8.36±1.6 | 8.8±1.9 | 8.72±1.4 | 8.45±1.4 | 0.244 |
| Preoperative IOP (mmHg) (Mean±SD) | 14.94±0.83 | 15.22±0.49 | 15.34±0.88 | 14.99±0.67 | 0.189 |
SD: Standard deviation
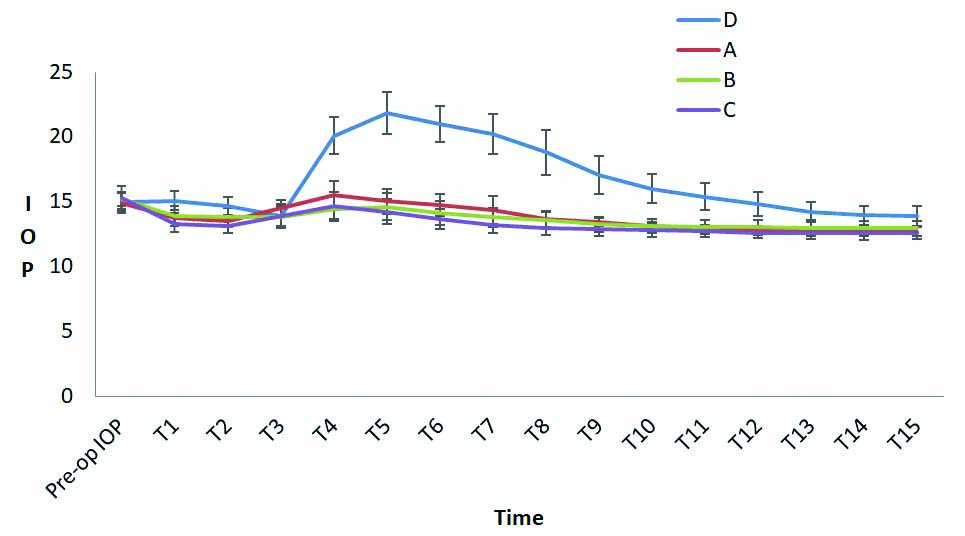
The mean IOP decreased after dexmedetomidine premedication in groups A, B and C (p<0.0001). Propofol administration further decreased IOP in all the groups. There was statistically significant difference in IOP between the control and study groups (p<0.0001). Succinylcholine administration and intubation caused a spike in the mean IOP of all the groups. The increase in IOP in control group was statistically significant when compared to the other groups (p<0.0001). But a comparison between the study groups showed no statistical significance even though the reduction in IOP was more in group C. The rise in IOP produced due to succinylcholine, laryngoscopy and intubation persisted upto five minutes after intubation. The difference in mean IOP between control and study groups remained statistically significant even after five minutes after intubation [Table/Fig-3,4].
Comparison of IOP (mmHg).
| Intraocular pressure | Group A | Group B | Group C | Group D | p-value |
|---|
| Before premedication (T1) | 13.77±0.41 | 13.92±0.74 | 13.27±0.59 | 15.1±0.75 | 0.40* |
| 0.11 ** |
| 0.10 *** |
| After premedication (T2) | 13.57±0.37 | 13.81±0.75 | 13.17±0.58 | 14.70±0.70 | 0.15* |
| 0.60 ** |
| 0.09 *** |
| After induction (T3) | 14.54±0.60 | 13.80±0.80 | 13.95±0.91 | 13.92±0.78 | 0.14* |
| 0.10 ** |
| 0.54 *** |
| 60 secs. after Suxamethonium (T4) | 15.53±1.10 | 14.49±0.94 | 14.72±1.03 | 20.12±1.40 | 0.12* |
| 0.10** |
| 0.41*** |
| Immediately After intubation (T5) | 15.04±0.98 | 14.64±1.04 | 14.228±0.96 | 21.86±1.61 | 0.17* |
| 0.50 ** |
| 0.15 *** |
| 1 min (T6) | 13.54±3.02 | 14.15±0.93 | 13.67±0.79 | 21.0±1.40 | 0.34* |
| 0.83 ** |
| 0.06 *** |
| 2 min (T7) | 14.37±1.06 | 13.82±0.73 | 13.22±0.62 | 20.25±1.54 | 0.39* |
| 0.09 ** |
| 0.30 *** |
| 3 min (T8) | 13.69±0.61 | 13.58±0.67 | 13.00±0.55 | 18.84±1.74 | 0.56* |
| 0.12 ** |
| 0.20 *** |
| 4 min (T9) | 13.46±0.33 | 13.28±0.59 | 12.91±0.50 | 17.04±1.46 | 0.19* |
| 0.11 ** |
| 0.19 *** |
| 5 min (T10) | 13.14±0.34 | 13.17±0.54 | 12.81±0.50 | 16.04±1.15 | 0.80* |
| 0.10 ** |
| 0.24 *** |
| 6 min (T11) | 14.74±0.86 | 13.08±0.53 | 12.78±0.47 | 15.4±1.04 | 0.44* |
| 0.38 ** |
| 0.43 *** |
| 7 min (T12) | 12.80±0.32 | 13.06±0.54 | 12.64±0.45 | 14.85±0.93 | 0.08* |
| 0.14 ** |
| 0.50 *** |
| 8 min (T13) | 12.73±0.33 | 13.01±0.59 | 12.62±0.46 | 14.23±0.74 | 0.47* |
| 0.33** |
| 0.12 *** |
| 9 min (T14) | 12.72±0.33 | 12.98±0.58 | 12.57±0.47 | 13.976±0.72 | 0.59* |
| 0.21 ** |
| 0.10 *** |
| 10 min (T15) | 12.72±0.33 | 12.96±0.58 | 12.596±0.48 | 13.91±0.78 | 0.80* |
| 0.29 ** |
| 0.20 *** |
*A vs B; **A vs C; ***B vs C
Distribution of Intraocular Pressure (IOP) in all groups (p<0.05 as compared to control group).
Hypertension was seen in seven patients in the control group and two patients in group C. The hypertension seen in group C was very short lived, not warranting any intervention. Hypotension was seen in four patients of group C, requiring Ephedrine and fluid boluses and two patients of group B, requiring a single bolus of Ephedrine. Bradycardia was seen in one patient in each of groups B and C, not warranting any treatment [Table/Fig-5].
Incidence of side-effects.
| Group | Hypertension | Hypotension | Bradycardia |
|---|
| A | 0 | 1 (4%) | 0 |
| B | 0 | 2 (8%) | 1/25 (4%) |
| C | 2/25 (8%) | 4/25 (16%) | 1/25 (4%) |
| D | 7/25 (28%) | 0 | 0 |
Discussion
In the present study, dexmedetomidine in all three doses were equally effective in preventing the rise of IOP associated with succinylcholine administration. However, the side-effects associated with the higher doses was a limiting factor.
The changes in IOP between the control and study groups correlated well with the studies done by Mowafi HA et al., and Pal CK et al., who also noted a similar trend in IOP after dexmedetomidine administration [8,10]. Jaakola ML et al., found a 34% reduction in IOP after a dexmedetomidine premedication alone [9]. On the contrary, Lee YY et al., found no effect of dexmedetomidine on IOP when supplemented with Isoflurane anaesthesia probably because their study used a much lower dose than the present study [11].
Dexmedetomidine when injected at the rate of 1 mcg/kg/hr is known to cause initial hypertension and a reflex bradycardia [7]. In the present study only two patients were recorded with such events may be because of premedication with inj. glycopyrolate and slow infusion of the drug over 10 minutes. Hypotension has been recorded in four patients in group C requiring Ephedrine and fluid boluses and in two patient of group B requiring a single bolus of Ephedrine each. The hypotension was probably exaggerated with induction dose of propofol therefore requiring treatment.
Dexmedetomidine in all three doses were equally effective, but a better haemodynamic stability was achieved with a dose of 0.6 μg/kg/IV with a significant reduction in IOP. Sedation produced by dexmedetomidine in group C might have unblinded the clinician administering the anesthetic agents but as an ophthalmologist was measuring the IOP, it did not affect the results.
Limitation(s)
Using a fixed dose of propofol caused undesired hypotension in group C which could have been avoided, but it was necessary for adequate blinding. Serum catecholamine could have been measured to get a better correlation but it could not be done because of the cost constraints.
Conclusion(s)
Premedication with dexmedetomidine is effective in attenuation of the rise in IOP associated with succinylcholine administration. It also significantly obtunded the sympathetic response to laryngoscopy and intubation. But a more desirable haemodynamic stability though not statistically significant was achieved with the dose 0.6 μg/kg. Therefore dexmedetomidine 0.6 μg/kg IV premedication can be used for attenuating the rise in IOP associated with succinylcholine administration in situations where rise of IOP may be detrimental.
SD: Standard deviation
*A vs B; **A vs C; ***B vs C
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. No
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 20, 2020
Manual Googling: Jan 04, 2021
iThenticate Software: Jan 09, 2021 (12%)
[1]. Cook JK, The effect of suxamethonium on intraocular pressureAnaesthesia 1981 36:359-65.10.1111/j.1365-2044.1981.tb10238.x7246985 [Google Scholar] [CrossRef] [PubMed]
[2]. Edmondson L, Intraocular pressure and suxamethoniumBr J Anaesth 1997 79:14610.1093/bja/79.1.1469301408 [Google Scholar] [CrossRef] [PubMed]
[3]. Murphy DF, Anaesthesia and intraocular pressureAnaesth Analg 1985 64:52010.1213/00000539-198505000-00013 [Google Scholar] [CrossRef]
[4]. Chidiac EJ, Raiskin AO, Succinylcholine and the open eyeOphthalmol Clin North Am 2006 9:279-85. [Google Scholar]
[5]. Chiu CL, Jaais F, Wang CY, Effect of rocuronium compared with succinylcholine on intraocular pressure during rapid sequence induction of anaesthesiaBr J Anaesth 1999 82:757-60.10.1093/bja/82.5.75710536557 [Google Scholar] [CrossRef] [PubMed]
[6]. Miller RD, (2015) Miller’s Anesthesia8th EditionSan DiegoChurchil Livingstone:863-67. [Google Scholar]
[7]. Gerlach AT, Dasta JF, Dexmedetomidine: An updated reviewAnn pharmacother 2007 41:245-52.10.1345/aph.1H31417299013 [Google Scholar] [CrossRef] [PubMed]
[8]. Mowafi HA, Aldossary N, Ismail SA, Alqahtani J, Effect of dexmedetomidine premedication on the intraocular pressure changes after succinylcholine and intubationBr J Anaesth 2008 100:485-89.10.1093/bja/aen02018285392 [Google Scholar] [CrossRef] [PubMed]
[9]. Jaakola ML, Ali-Melkkila T, Kanto J, Kallio A, Scheinin H, Scheinin M, Dexmedetomidine reduces intraocular pressure, intubation responses and anaesthetic requirements in patients undergoing ophthalmic surgeryBr J Anaesth 1992 68:570-75.10.1093/bja/68.6.5701351736 [Google Scholar] [CrossRef] [PubMed]
[10]. Pal CK, Ray M, Sen A, Hajra B, Mukherjee D, Ghanta AK, Changes in intraocular pressure following administration of suxamethonium and endotracheal intubation: Influence of dexmedetomidine premedicationIndian J Anaesth 2011 55(6):573-77.10.4103/0019-5049.9061122223900 [Google Scholar] [CrossRef] [PubMed]
[11]. Lee YY, Wong SM, Hung CT, Dexmedetomidine infusion as a supplement to isoflurane anaesthesia for vitreoretinal surgeryBr JAnaesth 2007 98:477-83.10.1093/bja/aem04017332003 [Google Scholar] [CrossRef] [PubMed]