Laser Excision of Large Peripheral Ossifying Fibroma, Histological and Radiographic Interpretation: A Case Report
Preeti Karhana1, Vidushi Sheokand2, Amit Bhardwaj3, Neha Munjal4
1 Postgraduate Student, Department of Periodontology, SGT Dental College, Gurugram, Haryana, India.
2 Reader, Department of Periodontology, SGT Dental College, Gurugram, Haryana, India.
3 Professor and Head, Department of Periodontology, SGT Dental College, Gurugram, Haryana, India.
4 Postgraduate Student, Department of Periodontology, SGT Dental College, Gurugram, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Vidushi Sheokand, Shree Guru Gobind Singh Tricentenary (SGT) University, Gurugram, Haryana, India.
E-mail: vidushi.sheokand@gmail.com
In oral cavity, the site for localised growth is usually gingiva which is considered as reactive in nature. Many of these lesions can be identified only on the basis of typical and consistent histomorphology and are difficult to identify clinically. One such reactive lesion which is clinically similar in presentation is Peripheral Ossifying Fibroma (POF). Females are affected more often than males. The presented case report is of a 45-year-old female with a significant growth of large POF in the anterior maxilla. The various clinical, radiological and histological features and diagnosis of POF with its treatment of choice are explained.
Calcifications, Calcifying fibroblastic granuloma, Gingival growth, Gingival hyperplasia
Case Report
A 45-year-old female patient presented to the Department of Periodontics, with the chief complaint of difficulty in closing mouth [Table/Fig-1], due to the growth of tissue in upper anterior region since two years. Patient had given a history of a swelling in upper front tooth region that had gradually increased in size, since the last 5-6 years. The past medical and family history was non-significant.
Lesion showing difficulty in closing mouth.

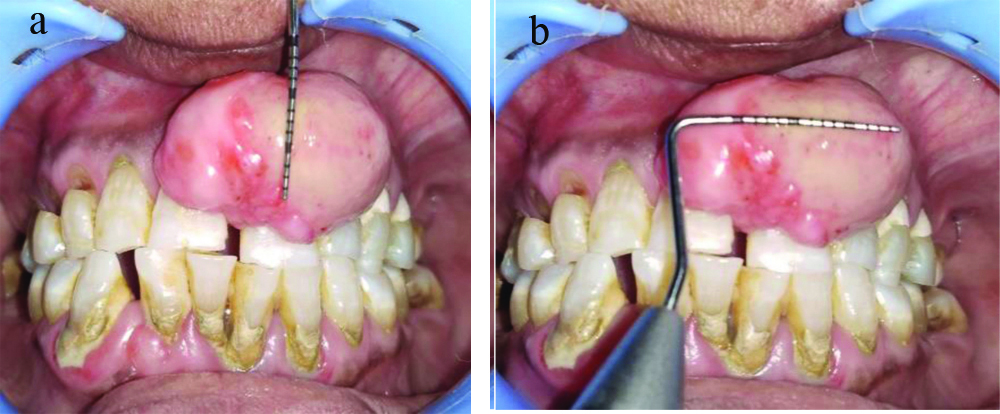
On extraoral examination, the lips were incompetent and swelling was seen in upper anterior region. The intraoral examination revealed a large solitary, hard pedunculated mass and lobulated pale pink exophytic growth with some erythematous areas involving the attached gingiva and buccal interdental papilla in relation to 11, 21, 22 and 23 [Table/Fig-2]. The lesion was pink in colour with a smooth and shiny surface, measuring approximately 13 cm [Table/Fig-3a, occluso-gingivally] and 20 cm [Table/Fig-3b, mesio-distally irt 11,21,22]. Any surface ulceration was not noted. The lesion was non tender and firm in consistency on palpation. No bleeding on probing or pus discharge was seen.
Clinically lesion interfering in the growth.

3a- Measurements from the middle thirds of the crown as lower border to the vestibular region as upper border
3b- Measurements- from distal aspect irt 11 to the mesial aspect irt 22,23.
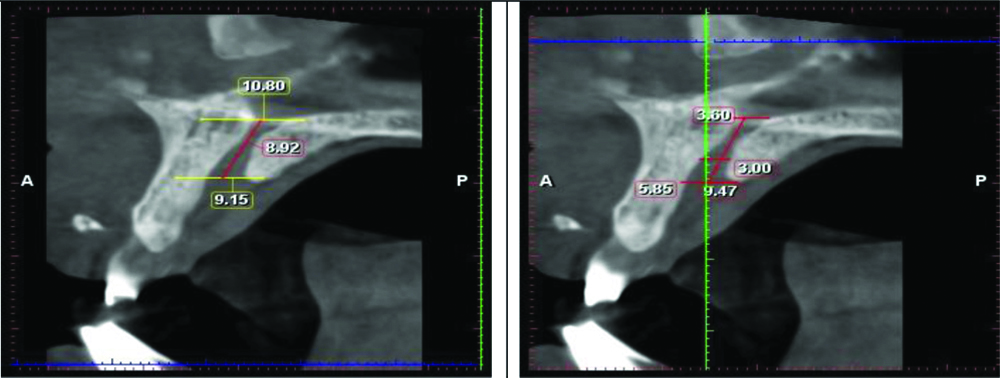
Patient had no previous dental history. Cone Beam Computed Tomography (CBCT) was performed for more accurate radiographic diagnosis and revealed two calcific foci of size approximately 4.97 × 1.54 mm and 3.66 × 1.01 mm. The lesion is approximately 4 mm away from the root (middle third portion) of 21. There is loss of labial cortical plate at the level of cervical and upper middle third portion of the root approximately 3 mm away from the CEJ, suggestive of cupping resorption secondary to soft tissue lesion [Table/Fig-4]. A blood examination was done in the pathology laboratory of the Dental College and no significant changes were found. Treatment of choice was the surgical excision of the lesion upto the entire removal of the diseased tissue. Complete treatment plan was explained to the patient and consent form was taken prior to the surgery.
Axial sections of CBCT showing measurements of the lesion irt 21.
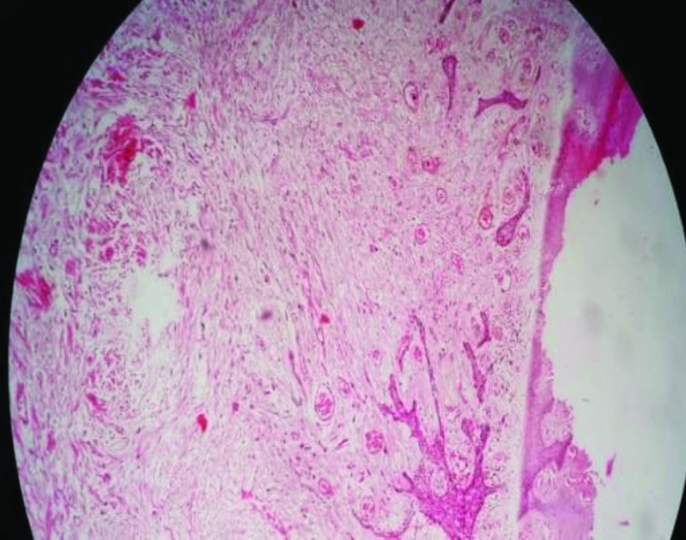
To eliminate the irritating factors, complete scaling and root planing was performed and after a week complete surgical excision of the lesion was planned. Complete lesion was excised with the help of laser (zolar diode laser of 810 nm wavelength at 3 watts with contact mode) under local anaesthesia [Table/Fig-5,6 and 7]. Precautions were taken not to harm the adjacent healthy tissues during excision. Neither sutures placed nor coe-pack given. The specimen was measured [Table/Fig-8] and sent to the oral pathology laboratory for histological examination [Table/Fig-9]. Postoperative instructions were given to take ibuprofen as analgesic when needed. Patient was advised to apply capsule evion twice for three days. Patient was advised to maintain oral hygiene and not to touch the lesion to prevent interference with the healing. The histopathological features were diagnostic of POF showing epithelium and connective tissue stroma. Epithelium was proliferative, stratified squamous. Underlying connective tissue composed of dense collagen bundles, numerous blood vessels, extravasated Red Blood Cells (RBCs) and in one area calcifications were seen [Table/Fig-10]. Healing was uneventful and patient was followed-up for 2-3 weeks [Table/Fig-11]. The protuberances over the lesion area were suggestive of recountouring of the bone. Flap was reflected [Table/Fig-12], resective osseous therapy done [Table/Fig-13], flap was sutured back [Table/Fig-14] and coe-pack placement (GC COE-PAK) was done [Table/Fig-15]. Again oral hygiene instructions were reinforced. At one week recall visit, sutures (3-0 ethicon, mersilk sutures) were removed [Table/Fig-16]. Healing was uneventual with complete resolution of the lesion. It was seen that osseous recountouring resulted in the establishment of tissue morphology which is favourable for oral hygiene and plaque control. Follow-up was done every 1-2 months for one year. No recurrence and complication were reported by patient and noticed by the dentist [Table/Fig-17].
Placement of diode laser for excision.
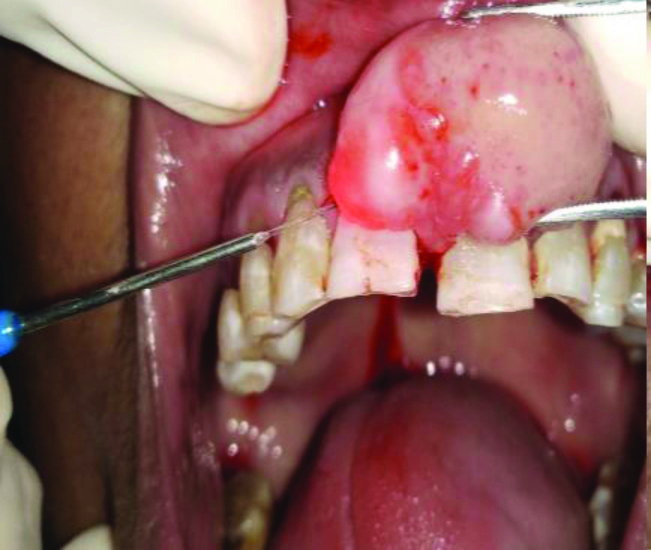
Tissue holding with forcep.

Area of lesion after its excision.

Excised tissue with measurements.
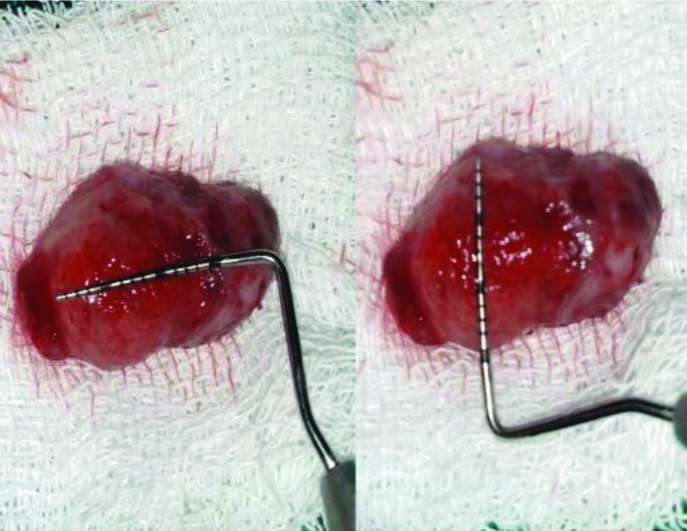
Specimen sent to oral pathology lab for histological analysis.

Histopathological section of the lesion H&E stain, 10x magnification.

Incision given and reflection done.

Vertical grooving done, resective surgery performed and debridement done.



Suture removal at one week.


Discussion
About 60% lesions occur anterior to molars in the maxilla [1]. Gardner coined the term POF. It should not be confused with PODF, which is the rare peripheral counterpart of central odontogenic fibroma. This lesion is thought to be derived from the periodontal ligament. Being odontogenic, it is still synonymously used by many for POF in North America [2]. It’s exclusive occurrence on gingiva, partly based on the demonstration of oxytalan fibers within its calcified structures and the evidence for its odontogenic origin is circumstantial. Unusual occurrence of POF associated with dental pulp has been reported [3]. Both the POF and Ossifying Fibroma (OF) originate from periodontal ligament cells and exhibit similar histomorphologic features. Both POF and OF have different proliferative activities, but both are a part of benign fibro-osseous lesion. POF is a reactive lesion and OF is neoplastic but benign [4]. The ulcerated lesions are usually painful, but it was not so in painful in the present case.
Within the soft tissue tumour mass, radiopaque foci are observed radiographically, if the calcified element is significant as the lesion was of longer duration of time. Initially, it may undergo subsequent fibrous maturation and calcification. In the progressive stage, the same spectrum of pathosis is represented [5]. The treatment for such lesions is the removal of other sources of irritants and thorough root scaling of adjacent teeth. An exuberant growth rate of reactive gingival lesions is exhibited and in a relatively short period of time a significant size is seen in children. It can interfere or delay eruption of the teeth, can displace the teeth, and can even cause erosion of the bone. Damage to teeth and bone can be avoided by early recognition of the lesion and its definitive surgical intervention [6].
Conclusion(s)
Peripheral Ossifying fibroma shares a varied clinico-pathological presentation. There exists a substantial overlap between various focal reactive overgrowths of gingiva for treatment, surgical excision is considered and compared with other reactive lesions, it may present a high recurrence rate. It is important to eliminate the etiological factors regardless of the surgical technique employed.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? NA
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 17, 2020
Manual Googling: Dec 07, 2020
iThenticate Software: Jan 19, 2021 (17%)
[1]. Walters JD, Will JK, Hatfield RD, Cacchillo DA, Raabe DA, Excision and repair of the peripheral ossifying fibroma: A report of 3 casesJ Periodontal 2001 72(3):939-44.10.1902/jop.2001.72.7.93911495143 [Google Scholar] [CrossRef] [PubMed]
[2]. Kale AM, Sethi KS, Karde PA, Peripheral ossifying fibroma of the anterior maxilla: A case report and brief reviewJ Oral Res Rev 2020 12(1):38-41. [Google Scholar]
[3]. Gardner DG, The peripheral odontogenic fibroma: An attempt at clarificationOral Surg Oral Med Oral Pathol 1982 54(1):40-48.10.1016/0030-4220(82)90415-7 [Google Scholar] [CrossRef]
[4]. Mesquita RA, Orsini SC, Sousa M, Araújo NS, Proliferative activity in peripheral ossifying fibroma and ossifying fibromaJ Oral Pathol Med 1998 27(2):64-67.10.1111/j.1600-0714.1998.tb02095.x9526731 [Google Scholar] [CrossRef] [PubMed]
[5]. Prasad S, Reddy SB, Patil SR, Kalburgi NB, Puranik RS, Peripheral ossifying fibroma and pyogenic granuloma. Are they interrelated?N Y State Dent J 2008 74(2):50-52. [Google Scholar]
[6]. Kenney JN, Kaugars GE, Abbey LM, Comparison between the peripheral ossifying fibroma and peripheral odontogenic fibromaJ Oral Maxillofac Surg 1989 47(4):378-82.10.1016/0278-2391(89)90339-X [Google Scholar] [CrossRef]