Tubercular Mediastinal Abscess in Non-immunocompromised Patient: A Rare Case Presentation
Yash Rana1, Vijendra Chouhan2, Saket Kumar3, Kusum V Shah4, Arti D. Shah5
1 Assistant Professor, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
2 Second Year Resident, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
3 Third Year Resident, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
4 Professor, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
5 Professor and Head, Department of Respiratory Medicine, Smt. S.B.K.S. Medical Institute and Research Centre, Sumandeep Vidyapeeth Deemed to be University, Vadodara, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Vijendra Chouhan, D-103, Shailraj Complex, Opposite to Baroda Dairy, Makar Pura Road, Tarsali, Vadodara-390009, Gujarat, India.
E-mail: vijendrachouhan5050@gmail.com
Mediastinal tuberculosis is a rare infection resulting from direct inoculation of organisms or through hematogenous spread. Infected lymph nodes may also transfer the bacilli through lymphatic route. Mediastinal tuberculosis may resemble a pyogenic abscess or tumour which might indicate tubercular aetiology and remains a clinical challenge. In tuberculosis endemic countries like India, all the abscesses indolent to routine treatment need investigation to rule out mycobacterial causes. Authors hereby report a case of 60-year-old male with anterior mediastinal tubercular abscess.
Hematogenous spread, Immuno-competent, Mediastinal lymph node, Pyogenic abscess
Case Report
A 60-year-old male farmer ex-smoker non-immunocompromised patient presented to the emergency department with complaints of cough with expectoration, shortness of breath {Modified Medical Research Council (MMRC) grade-3} and fever on and off, right-sided chest pain from past 2 months which was aggravated from past 20 days. Patient had complaints of loss of appetite, weight loss and generalised weakness from past 2 months. Earlier patient was treated with empirical antibiotics for 15 days but symptoms did not resolve. On auscultation, bilaterally decreased breath sound intensity was noted with crepitation’s in right inter scapular region.
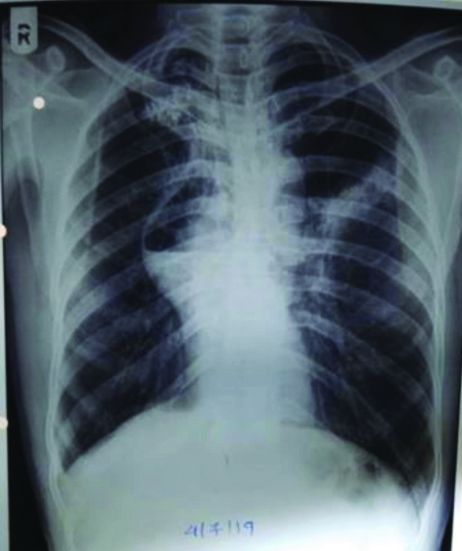
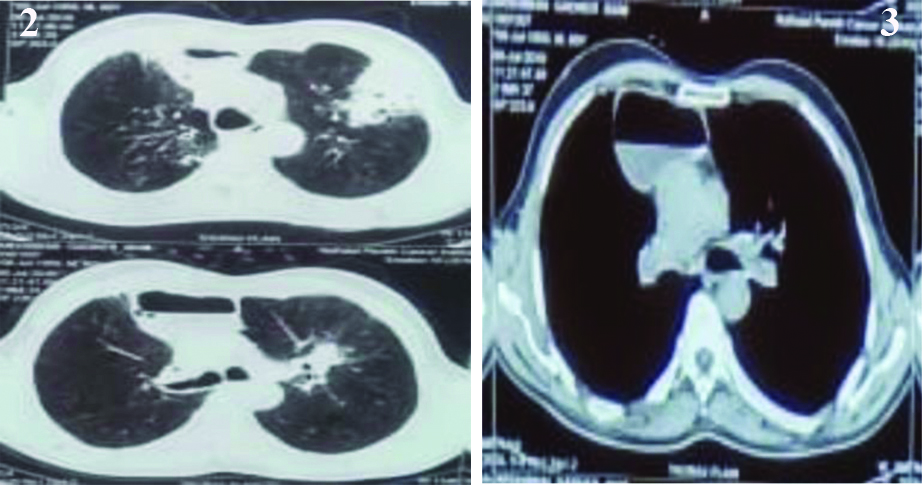
Chest X-ray Posterio-Anterior (PA) view suggested air-fluid level obscuring right hilar region with loss of contour of right diaphragm and some fibrotic bands over left mid zone [Table/Fig-1]. Computed Tomography (CT) thorax suggestive of a thick walled cavitatary lesion of 6.6 × 9.5 cm sized at anterior mediastinum with air-fluid level. Consolidation and subsegmental collapse is noted in adjacent right upper lobe anterior segment with some fibrotic granulomas and fibro-bronchiectasis changes. Centri-lobular emphysema and fibrotic bands noted bilateral basal lobes with multiple lymphadenopathies in prevascular and pretracheal regions with enhancing simple cyst in liver [Table/Fig-2,3]. Patient’s sputum sample was sent for Acid Fast Bacilli (AFB) and smear was negative but Cartridge-Based Nucleic Acid Amplification (CBNAAT) suggested Mycobacterium Tuberculosis (MTB). Rifampicin resistance was not detected by CBNAAT and sample was tested with Line Probe Assay (LPA) in which MTB was detected and were sensitive to Rifampicin and Isoniazid.
Air-fluid level obscuring right hilar region with loss of contour of right diaphragm and some fibrotic bands over left mid zone.
CT thorax suggestive of a thick walled cavitary lesion of 6.6×9.5 cm sized at anterior mediastinum with air-fluid level. Consolidation and subsegmental collapse is noted in adjacent right upper lobe anterior segment with some fibrotic granulomas and fibro-bronchiectasis changes. Centri-lobular emphysema and fibrotic bands noted bilateral basal lobes with multiple lymphadenopathies in prevascular and pretracheal regions with enhancing simple cyst in liver.
Patient was treated with Anti-Tubercular Treatment (ATT) 4 drugs regimen consisting of Isoniazid (H), Rifampicin (R), Pyrazinamide (Z), Ethambutol (E) according to National Tuberculosis Eradication Programme (NTEP) guidelines. Patient was called for follow-up after 15 days and then after second month, patient improved clinically and radiologically the size of the abscess reduced drastically. ATT was continued for 9 months and at the completion of treatment, patient showed significant clinico-radiological improvement [Table/Fig-4].
Resolved of air fluid level along with fibrosis in right Hilar region with right costo-phrenic angle blunted & some fibrotic bands over left mid zone.

Discussion
Mediastinal masses are routinely encountered in clinical practice and show a wide range of differential diagnosis which includes [1]: lymphoma, thyoma, germ cell tumour, thyroid enlargement, vascular lesion, lymphadenopathy, cystic lesion (pleuro-pericardial or bronchogenic), and rarely tuberculosis.
According to the latest report from the World Health Organisation (WHO) in 2019, tuberculosis had an incidence of 10.0 million (range 8.9-11.0 million) [2]. Here, isolated involvement of mediastinum is a rare presentation of tuberculosis [3] because the lesions grossly simulate pyogenic abscess or tumour and do not respond to conventional therapeutic interventions.
Three mechanisms described in the pathogenesis of tubercular mediastinal abscess are [4,5]:
Direct extension from pleural or pulmonary parenchymal disease,
Hematogenous dissemination of a dormant tuberculous focus,
Direct extension from lymphadenitis of the chest wall.
Diagnosis in most of the cases is demanding and challenging as the lesions grossly simulate pyogenic abscess or tumour and do not respond to conventional treatment with empirical antibiotics.
In the present case, patient presented shortness of breath (MMRC grade 3), cough with expectoration, fever (on and off) and right sided chest pain for 2 months which aggravated since last 20 days. Patient also complained of having loss of appetite, weight loss and generalised weakness since last 2 months. Patient gave the history of visiting the local hospital multiple times for 2 months, where he was treated empirically but didn’t respond to it.
Then the patient visited us and detailed workup including Chest X-ray (PA view) suggesting air-fluid level obscuring right hilar region with loss of contour of right diaphragm. Computed Tomography of thorax suggested a thick walled cavitary lesion at anterior mediastinum with air-fluid level. Consolidation and subsegmental collapse was noted in adjacent right upper lobe anterior segment and fibrotic bands noted bilateral basal lobes with multiple lymphadenopathies in prevascular and pretracheal regions. The sample was sent for CBNAAT and AFB for MTB detection. MTB was detected and Rifampicin and Isoniazid sensitivity was confirmed by LPA on same sample.
Patient was put on ATT 4 drugs regimen consisting of Isoniazid (H), Rifampicin (R), Pyrazinamide (Z), Ethambutol (E) under NTEP programme and called for follow-up after 15 days. On follow-up after second month patient improved clinically and radiologically the size of the abscess reduced drastically. ATT continued for 9 months, at the completion of treatment, showed significant clinical improvement.
There are few known cases of tuberculosis isolated anterior mediastinal mass in nonimmune-competent patient. Comprehensive literature review reveals 10 related cases with the majority arising from the infant population of 2 years of age or younger. From the adult cases identified, all three patients were males, aged between 32 to 76 years [6-9]. All the three patients were given medical care. From the restricted written data available on adult manifestations of mediastinal tuberculosis in non-immunocompetent patients, announce that the presentation is typically correlated with the symptoms of mass effect and that a diagnosis was revealed only after histological evidence [10-14], but in our case scenario of 60-year-old male, the diagnosis was made after the sputum CBNAAT and LPA results.
In our country like India, that has massive pool of tuberculosis cases and in the background of priority to pick up open cases, there is a possibility that extra-pulmonary tuberculosis like mediastinal abscess may be missed or misdiagnosed. Because primary tubercular involvement of extra-pulmonary site like chest wall and mediastinal abscess is extremely rare. Identification of extra-pulmonary isolates would be absolutely essential for instituting right therapeutic intervention but with limited facilities for mycobacterial culture and sensitivity some kinds of linkages are required to provide support services to sites engaged in handling tuberculosis patients.
Conclusion(s)
Tuberculosis can appear in rare presentations like mediastinal abscess in non-immuno-compromised patients CBNAAT & LPA has better efficacy over traditional ZN staining in diagnosing pulmonary and extra-pulmonary tuberculosis, it not only helps in early diagnosis of MTB but also suggests drug resistance.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Nov 06, 2020
Manual Googling: Nov 23, 2020
iThenticate Software: Dec 24, 2020 (9%)
[1]. Strollo DC, Rosado de Christenson ML, Jett JR, Primary mediastinal tumours. Part 1: tumours of the anterior mediastinumChest 1997 112(2):511-22.10.1378/chest.112.2.5119266892 [Google Scholar] [CrossRef] [PubMed]
[2]. Global tuberculosis report 2020. Geneva: World Health Organization; 2020. Licence: CC BY-NC-SA 3.0 IGO [Google Scholar]
[3]. Khilnani GC, Jain N, Hadda V, Arava SK, Anterior mediastinal mass: A rare presentation of tuberculosisJ Trop Med 2011 2011:635385Epub 2011 Mar 710.1155/2011/63538521461350 [Google Scholar] [CrossRef] [PubMed]
[4]. Sakuraba M, Sagara Y, Komatsu H, Surgical treatment of tuberculous abscess in the chest wallAnnals of Thoracic Surgery 2005 79(3):964-67.10.1016/j.athoracsur.2004.09.00415734414 [Google Scholar] [CrossRef] [PubMed]
[5]. Cho KD, Cho DG, Jo MS, Ahn MI, Park CB, Current surgical therapy for patients with tuberculous abscess of the chest wallThe Annals of Thoracic Surgery 2006 81(4):1220-26.ISSN 0003-497510.1016/j.athoracsur.2005.10.04416564247 [Google Scholar] [CrossRef] [PubMed]
[6]. Tan CH, Kontoyiannis DP, Viswanathan C, Iyer RB, Tuberculosis: A benign imposterAJR Am J Roentgenol 2010 194(3):555-61.10.2214/AJR.09.305520173128 [Google Scholar] [CrossRef] [PubMed]
[7]. Jeong YJ, Lee KS, Pulmonary tuberculosis: Up-to-date imaging and managementAJR Am J Roentgenol 2008 191(3):834-44.10.2214/AJR.07.389618716117 [Google Scholar] [CrossRef] [PubMed]
[8]. Kim HY, Song KS, Goo JM, Lee JS, Lee KS, Lim TH, Thoracic sequelae and complications of tuberculosisRadiographics 2001 21(4):839-60.10.1148/radiographics.21.4.g01jl0683911452057 [Google Scholar] [CrossRef] [PubMed]
[9]. Leung AN, Brauner MW, Gamsu G, Mlika-Cabanne N, Ben Romdhane H, Carrette MF, Pulmonary tuberculosis: Comparison of CT findings in HIV-seropositive and HIV-seronegative patientsRadiology 1996 198(3):687-91.10.1148/radiology.198.3.86288558628855 [Google Scholar] [CrossRef] [PubMed]
[10]. Codecasa LR, Besozzi G, De Cristofaro L, Miradoli A, Sabolla L, Tagliaferri B, Epidemiological and clinical patterns of intrathoracic lymph node tuberculosis in 60 human immunodeficiency virus-negative adult patientsMonaldi Arch Chest Dis 1998 53(3):277-80. [Google Scholar]
[11]. Vincken W, Vandenbrande P, Roels P, Pirngadi J, Welch W, Isolated paratracheal mass of tuberculosis origin in an adult patientEur J Respir Dis 1983 64(8):630-35. [Google Scholar]
[12]. Jain N, Khilnani G, Hadda V, Iyer V, Cystic mediastinal mass: A rare presentation of tuberculosisChest 2013 144(4):212AMeeting Abstract10.1378/chest.1704236 [Google Scholar] [CrossRef]
[13]. Kumar N, Gera C, Philip N, Isolated mediastinal tuberculosis: A rare entityJ Assoc Physicians India 2013 61(3):202-03. [Google Scholar]
[14]. Maeder M, Ammann P, Rickli H, Schoch OD, Fever and night sweats in a 22-year-old man with a mediastinal mass involving the heartChest 2003 124(5):2006-09.10.1378/chest.124.5.200614605080 [Google Scholar] [CrossRef] [PubMed]