Brachial plexus blockade is the most often performed anaesthetic technique for upper limb surgeries. Axillary Brachial Plexus Block (ABPB) is commonly used to achieve upper limb regional anaesthesia and it is inceasingly performed by blocking the terminal branches of the brachial plexus. A common notion for block failure was attributed to needle displacements or existance of septa inside the plexus sheath in the axillary region [1]. Higher volumes upto 60 mL have been implicated in brachial plexus blocks aiming to highten the success rates [2]. Nevertheless, employing larger volumes of local anaesthetics will only culminate in systemic toxicity [3]. Therefore, reducing the mass of the local anesthetic involved in the blockade will safegaurd the patient from systemic complications.
Presently, the advent and utility of peripheral nerve stimulator and ultrasound, targets precise needle placement in relation to the complex eventually reducing the local anaesthetic volume employed for a nerve blockade [4]. USG guided local anaesthetic volume reduction have been well-documented in interscalenic brachial plexus blocks [5,6], femoral nerve blocks [7-9], and ilioinguinal/iliohypogastric [10] nerve blocks without jeoparadising the quality. However, there are paucity of studies [11,12] on the minimum effective volume of local anesthetic employed for axillary brachial plexus blockade which infer that lower volumes can provide effective anaesthesia and increase the safety of the procedure.
Hence, this study was aimed to assess efficacy of two different low volumes of 0.375% bupivacaine in cases receiving ultrasound-guided axillary block. The primary parameters studied were onset and duration of sensory and motor blockade, duration of postoperative pain relief and secondary outcomes were haemodyamic parameters namely Heart Rate (HR), Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) and complications.
Materials and Methods
This double blinded randomised controlled study was conducted in Department of Anaesthesiology, during the period of January 2014 to June 2015. The study was approved by the Institutional Ethics Committee (IEC:RC/13/101) prior to the commencement and written informed consent from patients was obtained.
Inclusion criteria: Sixty American Society of Anesthesiologists (ASA) I and II patients between age group 18 to 60 years undergoing elective forearm and hand surgeries of two hours duration were included.
Exclusion criteria: Patients with infection at the site of injection, clinically significant coagulopathy, previous nerve muscle degenerative disorders, severe cardiopulmonary diseases, hepatic or renal dysfunctions, pregnancy and lactation and those taking opioids or chronic analgesic therapy for any other illnesses were excluded from the study.
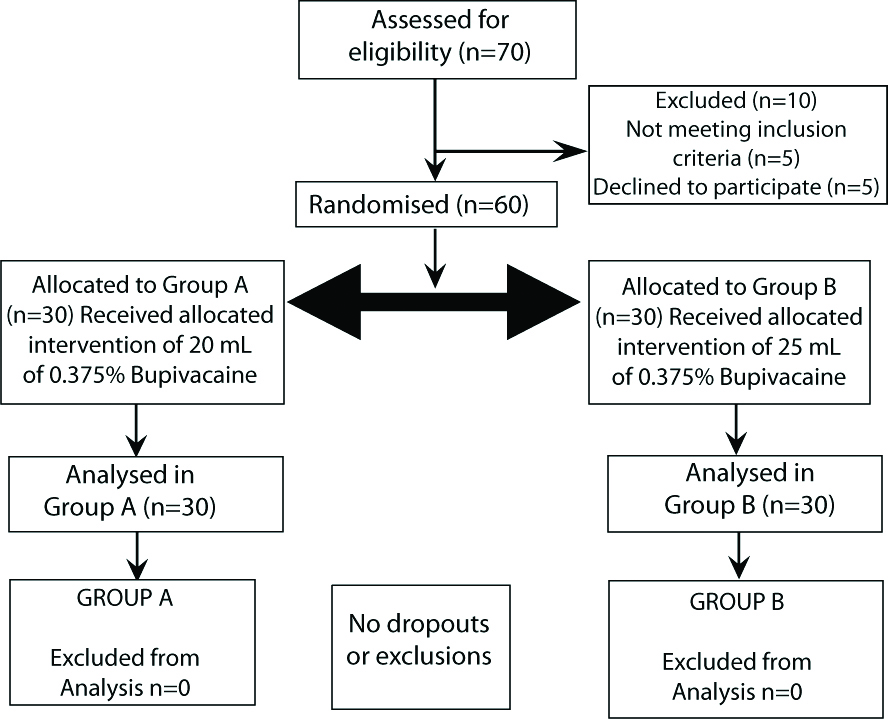
Patients were allocated in a randomised manner by computer generated randomisation chart into two groups of 30 each. Group A received 20 mL of 0.375% bupivacaine and Group B received 25 mL of 0.375% bupivacaine as depicted in a consort flow diagram in [Table/Fig-1].
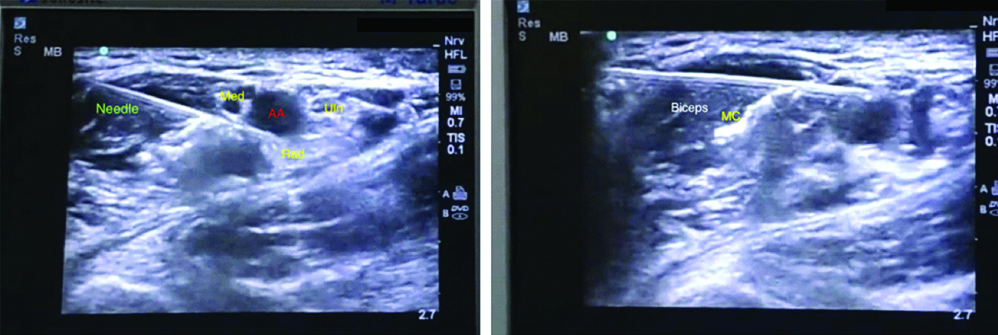
Anaesthesiologist involved in the data collection as well as the patients were blinded to the content of the study solution. All patients were pre-medicated with oral antacid (Tab. Ranitidine 150 mg) and anti-anxiety medications (Tab. Diazepam 5 mg) the night before as well as in the morning on the day of surgery. Pre-operatively, 18G IV cannula was secured and IVF (Ringer lactate) was initiated at 5 mL/kg/hr. The patients were then shifted to the operation theatre and monitors namely electrocardiogram, non-invasive BP, and pulse oximeter were attached and baseline readings were taken according to ASA standard recommendations. All patients received Inj. Midazolam 1.5 mg intravenously before the procedure. A 4 cm linear transducer with frequency of 5 to 10 MHz and a 100 mm 22 gauge insulated short bevel needle (Stimuplex; B. Braun, Germany) was used for performing the block in all patients. For positioning of the limb, both arm and elbow of the surgical hand were placed in 90° abduction in relation to each other as a conventional way of performing axillary block. After identification of the neural (median, ulnar, radial nerve) muscular (biceps and triceps muscle) and vascular structures (axillary artery and vein), the needle was introduced in plane to the transducer and local anaesthetic solution was deposited in and around the terminal branches of the plexus through subcutaneous needle manipulation under ultrasound guidance through a single needle entry point with one-fourth of the study medication deposited per nerve [Table/Fig-2]. The local anaesthetic solution was administered by experienced anaesthesiologists. Sensory assessment was performed by pinprick method with a 23 gauge hypodermic needle at 5, 10, 15, 20 and 30 minutes after completion of drug ingestion. Cutaneous innervation pertaining to median, ulnar, radial and musculocutaneous nerve were assessed by the following scale [13]; 2 as Normal sensation, 1 as Hypoasthesia and 0 as No sensation felt. Onset of sensory blockade was confirmed with a score of 0 on all nerve territories.
Ultrasonographic Image. Left- Medial (Med), Ulnar (Uln) and Radial (Rad) nerves in relation to the Axillary artery and needle placement is marked. Right- Musculocutaneous nerve (MC) shown in matrix of biceps muscle.
Motor blockade was evaluated at 5, 10, 15, 20 and 30 minutes following the injection of the drug according to Lavoie J et al., [14]. The percentage of blockade was assesed as 0% when flexion and extension in the hand and arm against resistance are present, 33% when flexion along with extension in the hand and arm against gravity is present but not against resistance, 66% when flexion along with extension movements in the hand is present but not in the arm and 100% when no movements are possible in the entire upper limb.
The success rate of the blockade was determined by using Vester Anderson’s criteria [15] which classifies the nature of block success into three types. A complete block is when sensory block of the entire distribution of arm sparing the axillary nerve is achieved, an incomplete block when nil or incomplete sensory block is observed in some of the nerve territories and a failed block when there was complete absence of sensory block in all major nerve territories or presence of sensory block in only one of the major nerve territories.
Intraoperative events like need for supplementary analgesia, seizure, cardiac dysrhythmias, oxygen desaturations and any signs of local anaesthetic systemic toxicity were noted. In situations of insufficient analgesia for the surgical procedure, the block was systemically supplemented with Inj.fentanyl (0.5 mcg/kg) or Inj.fentanyl (0.5 mcg/kg) plus Inj.propofol infusion (50-75 mcg/kg/min). Any block failure was excluded from the study and general anaesthesia was administered to proceed further with the surgical procedure.
Postoperative monitoring was done in the Postanaesthesia Care Unit (PACU). Postoperative pain was evaluated by Visual Analogue Scale (VAS) score every 30 minutes for the first two hours and every hour then on until a score of more than 3 or patients subjective complain of pain. A VAS score of more than 3 any time postprocedure was recorded as end point of duration of analgesia and Inj. Diclofenac sodium 75 mg intramuscularly was given as rescue analgesia.
Taking into consideration, the onset time of sensory blockade as the main outcome of interest and from a previous study in which, the mean value of sensory onset being 25±14.8 minutes in the study group and 15.8±6.8 minutes in the control group with a power of study of 80% and with significance level of 5%, the sample size was calculated as 25 in each group; considering allowance for 10% dropouts, the sample size was increased to 30 in each group [16].
Statistical Analysis
All data were entered in an Excel®-Sheet for documentation. For statistical analysis, the program Statistical Package for the Social Sciences (SPSS) version 20.0® for Windows was used. Differences in the onset times and anaesthesia between the four nerves were tested using Repeated Measures Analysis of Variance (ANOVA), t-test, Mann-Whitney test. Statistical significance was defined as p<0.05.
Results
In total, 60 patients were randomised, 30 patients per group. All patients received the allocated intervention. Baseline demographic profile of the two groups did not differ significantly [Table/Fig-3].
| Demographics | Group A | Group B | p-value |
|---|
| Age in years (Mean±SD) | 28.6±11.3 | 30.8±9.5 | 0.13 |
| Sex (M/F) | 27/3 | 25/5 | |
| Weight in kg | 58.8±10.1 | 63.6±10.9 | 0.08 |
| ASA (I/II) | 20/10 | 22/8 | |
| Duration of surgery (minutes) | 75±10 | 80±10 | |
M: Male; F: Female; SD: Standard deviation; ASA: American society of anesthesiologists
The mean time for onset of sensory block in group A (19.0±4.4 min) and group B (19.5±5.1 min) as well as the mean time for onset of motor block in group A (19.8±3.1 min) and group B (20.5±3.0 min) are shown in [Table/Fig-4]. No significant difference in onset of sensory as well as motor blockade between the two groups were observed as shown by students unpaired t-test with p-values of 0.69 and 0.40, respectively.
Time for onset of sensory and motor block (Min).
| Onset time (min) | Group A | Group B | p-value |
|---|
| Sensory onset time | 19.0±4.4 | 19.5±5.1 | 0.69 |
| Motor onset time | 19.8±3.1 | 20.5±3.0 | 0.40 |
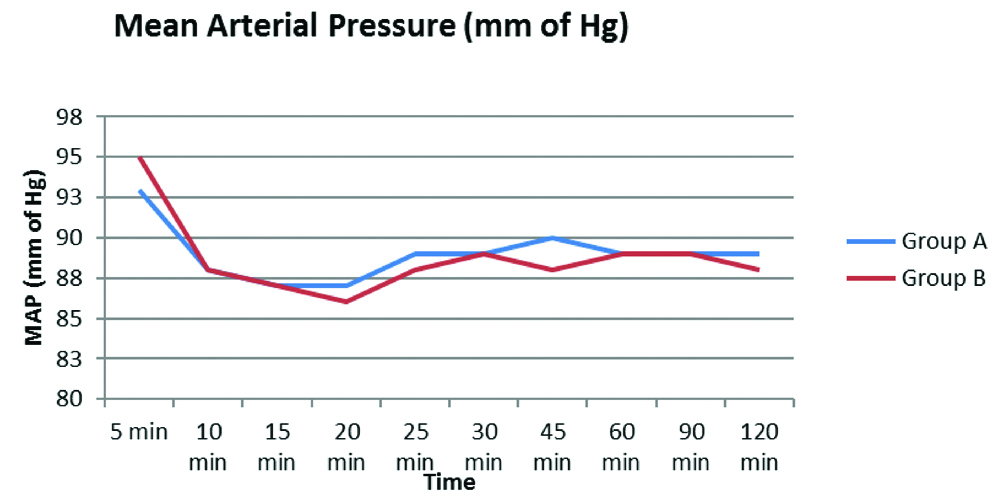
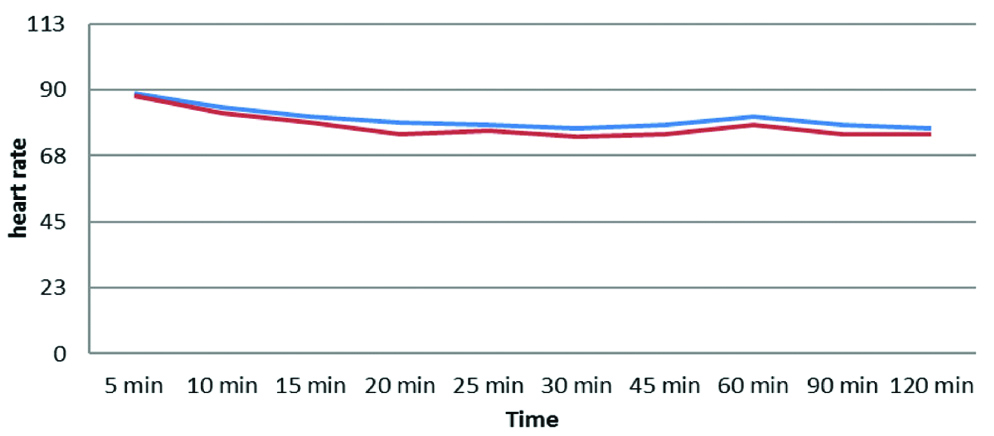
The mean duration of block in group A was 8.5±2.7 hours and group B was 12.2±3.4 hours. Group B had a significantly longer duartion of blockade in comparison to group A showed by students unpaired t-test with p-values <0.001 as in [Table/Fig-5]. Intraoperatively, two patients in group A and three patients in group B had mild pain which was controlled by Inj. fentanyl 25 mcg bolus intravenously. HR, systolic BP, Mean Arterial Pressure (MAP), diastolic BP, were recorded before performing the block and every 5 minutes for the first 30 minutes then every 15 minutes until the first hour and at 90 and 120 minutes respectively. The statistical analysis by Repeated measures ANOVA and F-test showed that there was no significant difference in HR (p-value 0.12), SBP and DBP (p-value 0.63 and 0.67) and MAPs (p-value 0.79) between the two groups [Table/Fig-6,7].
| Study group | Duration of block (Hours) | Mean difference | t-value | p-value |
|---|
| A | 8.5±2.7 | 3.7 | 4.60 | <0.001 |
| B | 12.2±3.4 |
Mean arterial pressure (mm of Hg).
Heart Rate (HR) Changes (Bpm).
None of the patients required conversion to general anesthesia due to block failure. There were no signs of local anaesthetic toxicity during the procedure or incidence of nerve damage during postoperative screening.
Discussion
The axillary approach to brachial plexus block was chosen for this study because of its propensity to block individual nerves preferentially with low volumes of local anaesthetics, thereby reducing systemic toxicity. Only patients undergoing surgical procedures in the hands of less than two hours duration were selected thoughtfully considering the lack of knowledge about the block duration with low volume of local anaesthetic being used. In this study, the onset of action of sensory blockade between the two groups were comparable and had no significant difference (p=0.69), inspite of a low volume of local anaesthetic being used primarily creating a clinical and statistical evidence that onset times are not affected with volume of local anaesthetics being used.
Marhofer P et al., studied the potency of low volume axillary plexus block with 1% mepivacaine and demonstrated similar onset times with low volumes of local anaesthetics in ten volunteers who received either 0.11 mL/mm2 (low volume) or 0.4 mL/mm2 (high volume) cross-sectional nerve area. The mean volume employed was 4.0±1.0 mL in the low volume group and 14.8±3.8 mL in the high volume group. The mean sensory onset time was 25.0±14.8 minutes in the low volume group and 15.8±6.8 minutes in the high volume group (p<0.01) was statistically significant, but this study was not powered to find an actual significance in shorter onset times with slightly higher volumes leaving an ambiguity in considering the significant change in the onset times of their study. Other consideration that has to be made is the very low volume of 4 mL employed in the low volume group that could be too low to cause an earlier onset time compared to the high volume group of 15 mL [16].
The mean time for onset of motor blockade also had no significant difference between the two groups in this study (p=0.40). Mogahed MM and Abd El Ghafar MS, observed similar motor onset patterns when they compared two different doses of 0.5% bupivacaine (group 1 received 30 mL vs group 2 received 20 mL) in USG guided supraclavicular brachial plexus blockade in arteriovenous shunt surgeries in chronic renal failure patients. The mean motor onset times were 22.2±2.1 minutes in Group 1 and 22.5±2.4 minutes in Group 2 (p=0.64) which was insignificant and similar to present study’s findings [17].
The duration of blockade was significantly prolonged in group B compared to group A in this study with p-value <0.001. Similar findings were encountered by Fenten MG et al., who investigated to derive a connection between the effect of dose, volume and concentration of mepivacaine on the quality of anaesthesia in USG guided axillary brachial plexus blockade using different volumes and concentrations of the same dose 300 mg (20 mL 1.5% mepivacaine 300 mg in group A and 30 mL 1.0% mepivacaine 300 mg in group B) vs. same volume of 30 mL with higher dose and concentrations of mepivacaine (30 mL of 1.5% mepivacaine 450 mg in group C). The interesting inferences of their results revealed that changes in volumes between 20 and 30 mL with same dose of local anaesthetics (300 mg) taken in group A and B did not have a significant difference in duration of blockade (sensory p>0.1), but increasing the dose to 450 mg in group C resulted in significant prolongation in the duration of blockade [18]. A slightly increased dose in group B in this study could have culminated in a significant difference in duration between the groups. A similar prolongation in duration of sensory block was also encountered by Marhofer P et al., with increase in volume of the local anaesthetic used, but the major limitation of this finding was that their study was not powered to find a difference in the volume associated to increase the block duration, leaving only a clinical evidence of block prolongation with higher volumes [16].
There were no significant changes in heamodynamics between the two groups. Two patients in group A (25 mL) and one patient in group B (30 mL) had hypoesthesia (score 1). These patients were supplemented with Inj. fentanyl 50 mcg bolus to provide adequate analgesia introperatively with no requirement for exclusion from the study leading to similar success rates in both groups. The primary reason for requirement of supplementary analgesia could only be related to procedural discrepancies. Kapral S et al., compared USG guided supraclavicular vs. axillary approach to brachial plexus in 40 patients undergoing forearm and hand surgeries. Satisfactory sensory and motor block was observed in 95% of patients in both the groups. All patients in supraclavicular group had satisfactory intraoperative blockade whereas 25% of axillary plexus group had incomplete blockade intraoperatively requiring fentanyl boluses which was in line with this study [19].
There were no intraoperative or procedure related complications during the study. Finally, the primeval consistent finding is that the volume of local anaesthetic does not influence the onset of a nerve block and using lower volumes of local anaesthetics can provide equally efficacious blockade as obtained with conventional volumes. Absolute vigilance in needle visualisation, needle tip position, and injection spread will eliminate inadvertant intravascular and intraneural injections thereby reducing complications relating to both technique and drug over dose.
Limitation(s)
The major limitation of this study was the inability to find the least volume required to provide effective anaesthesia, hence further research should be targeted in larger sample size with wider group range including more groups with graded low volumes to invent an effective least volume that would be sufficient for a considerable anaesthesia for upper limb surgeries.
Conclusion(s)
Low volumes of local anaesthetics are equally efficacious compared to conventional volumes of local anaesthetics for elective upper limb surgeries using ultrasound guided axillary brachial plexus blockade.
M: Male; F: Female; SD: Standard deviation; ASA: American society of anesthesiologists