Intertrochantric fractures have been acknowledged as one of the most commonly occurring fractures in the elderly osteoporotic population. Prolonged bed rest following a hip fracture adds to the morbidity as well as the mortality in these patients. Thus, the treatment aims at the restoration of the patients to their pre-injury status as early as possible and this entailed internal fixation to be accepted as the standard of management to gain acceptable reduction and early mobilisation [1]. The problems of instability and the complications resulting out of it after internal fixation have plagued the orthopaedic surgeons for long. Intrinsic factors like osteoporosis and comminution at the fracture site and extrinsic factors like the quality of reduction and the type of implant and insertion techniques have a significant bearing in the failure of internal fixation [2-4]. Implant failure has devastating complications and revision surgery has a high morbidity further compounded by the poor general condition of these old patients and thus, the quest to find an ideal implant which would deliver a durable fixation to these fractures has provided fuel to the ongoing research for many years.
Sliding devices like the dynamic hip screw which were once extensively used for fixation have been found to be ill-suited to fix the unstable class of these fractures [5]. They can penetrate the head or the neck of the femur and can bend, break or separate if the patient bears weight early especially in comminuted fractures [6,7]. An intramedullary nail with a dynamic femoral head-neck implant is the implant of choice to fix them [8]. Their intramedullary placement keeps them close to the mechanical axis of the femur and decreases the lever arm and the bending movement on them. They require less time for insertion with less intraoperative blood loss and allow early weight bearing with less resultant shortening on long term follow-up.
Although superior to extramedullary devices for unstable Intertrochantric fractures proximal femoral nail has its own impediments. Numerous complications like screw cut out, back out, varus collapse and rotational instability have been reported and upto 31% complication rate has been cited with their use [9]. The design of PFN has undergone many changes since its inception. The PFNA employs only a single helical blade instead of a screw system for fixation. The helical blade, which is inserted by hammering and not by reaming out the bone, is said to result in the compaction of the surrounding cancellous bone and thus imparts supplemental anchorage, especially in osteoporotic bone [10]. A stronger resistance to rotation and varus collapse has been demonstrated by a biomechanical study [11]. Contrarily, cut through into the hip joint, cut out and back out have also been shown with the helical screws [12].
Owing to the theoretical advantage of PFNA in osteoporotic bone, this prospective study was conducted to study the functional outcomes with the use of PFNA for internal fixation of intertrochantric fractures in osteoporotic subjects and to see whether these theoretical advantages translate into clinical gains in these osteoporotic elderly patients or not.
Materials and Methods
This prospective interventional study was conducted at the Uttar Pradesh University of Medical Sciences (UPUMS), Saifai, Etawah. For this study, all the patients from December 2015 to November 2018, with osteoporotic intertrochanteric fractured femur who were admitted under the investigating consultant, who met the inclusion criteria and consented to participate in the study were enrolled in the study. Patients with a minimum follow-up of 12 months postsurgery were included in the final evaluation. Ethical clearance was obtained from Institutional Ethical Committee (09/UPUMS/Dean(M)/Ethical/2015) and written informed consent was obtained from each patient. A total of 68 patients were enrolled initially. Out of them six patients were lost in the follow-up and the results of 62 patients were evaluated.
Inclusion criteria:
Age more than 50 years.
Patient able to walk prior to injury.
Minimum follow-up of 12 months.
Less than one month old injury.
Close or open (Gustilo grade) [13].
Polytrauma without any significant ipsilateral lower limb fractures.
Fractures with subtrochantric extension of <5cm.
Exclusion criteria:
Significant active infection anywhere in the body.
Unstable medical illness.
Patients on long term corticosteroids.
Significant concomitant ipsilateral lower extremity trauma.
Preoperative significant functional loss or comorbidity in ipsilateral lower extremity.
Nontraumatic disorder, pathological fractures.
Inability to comply with rehabilitation protocol and to complete the forms.
Pure subtrochantric fractures and fractures extending more than 5 cm below the lesser trochanter.
The patients were evaluated as per the history, mode of injury and anterio-posterior and lateral radiographs of the affected hip which were done on admission. They were then put on skin traction over a Bohler-Braun frame. The AO alphanumeric classification was used to classify the fractures [14]. Patients were taken up for surgery on the next elective Operation Theatre (OT) day. Adequate blood transfusion and other supportive measures were given depending on the preoperative condition of the patient and blood loss during surgery. The duration of surgery, blood loss and fluoroscopy time were recorded intraoperatively and immediate postoperative radiographs, Antero-Posterior (AP) and lateral views of the operated hip were obtained.
All patients received injectable antibiotics (cephalosporins) which were started one hour before surgery and continued postoperatively for two to three days. Oral cephalosporins were continued for next three to four days. Aminoglycosides were added intraoperatively if the procedure was prolonged. Analgesics were initially given via IV or IM route for two to three postoperative days and then orally for few days. Low molecular weight heparin as an anti-deep vein thrombosis prophylaxis was used only in some patients in this study.
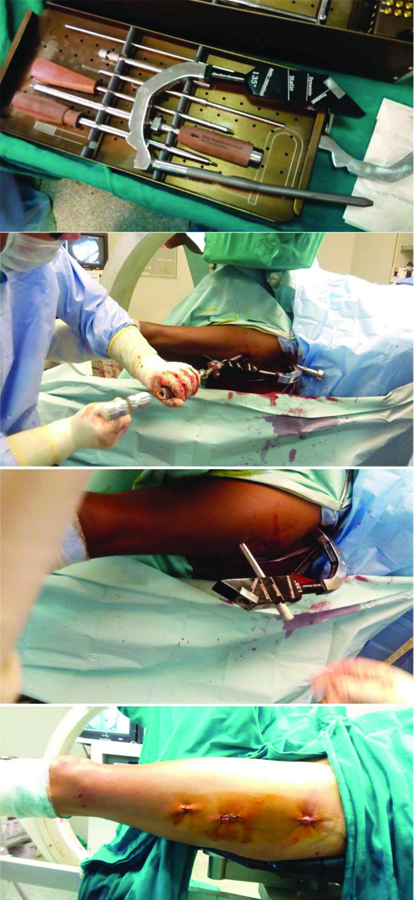
Anaesthesia was given as per the decision of the anaesthesia team. Patients were positioned on the fracture table with ipsilateral arm elevated on a sling and uninjured leg in a leg holder. Injured leg was kept in around 10-15 degrees adduction. Entry point was taken at the tip or slightly lateral to the tip of the greater trochanter in the curved extension of the medullary cavity, as the ML angle of the PFNA is 6 degrees. In the lateral view, the entry point was in line with the axis of the intramedullary canal. The medullary cavity was reamed to a diameter that was at least 1mm larger than that of selected nail. The ante version was determined by inserting a guide wire ventral to the femoral neck in the femoral head. Proximal locking was done using the hexagonal screwdriver with spherical head, connecting screw confirmed between the insertion handle and PFNA was sufficiently tightened. Aiming arm was mounted based on the Centum Collum Diaphyseal (CCD) angle. Guide wire was put through a sleeve under image intensifier. In very unstable fractures, additional guide wire was inserted to prevent any rotation. In AP and lateral views, the correct position of PFNA blade which is 10 mm below the joint level was confirmed. Intraoperative compression was done by a screwing compression instrument into the blade through protection sleeve. Compression was avoided in osteoporotic bones. Both short and long PFNA nails were locked distally and differently with options of static and dynamic locking under image [15]. All patients were given perioperative antibiotics for 24 to 48 hours and deep venous thrombosis prophylaxis. Patients were allowed to sit up in bed on the second postoperative day. Static quadriceps exercises were started on the second and third postoperative day. Sutures were removed after 10 to14 days. Patients were allowed non-weight bearing walking after the pain had subsided if the general conditions permitted. Weight bearing was determined by the stability of the fracture and adequacy of fixation and was delayed for patients with unstable or inadequate fixation [Table/Fig-1].
Intraoperative clinical pictures showing the procedure.
All the patients were followed-up at two weeks for suture removal followed by at 1 month and then monthly till fracture union and 3 monthly thereafter. Radiographs of affected hip were obtained in AP and lateral planes at each follow-up visit and any changes in position of implant and extent of fracture union were noted. Fractures were judged to be healed radiographically if bridging callus was evident on 3-4 cortices as noted on two views [16].
HHS was used in this study for regular follow-up and evaluation at each and every follow-up visit. Final evaluation was done at 12 months of follow-up [17].
Statistical Analysis
The statistical analysis involved calculation of the mean and Standard Deviation of the above parameters which was done using the Microsoft excel chart sheet (version-10.0)- 2010 home edition.
Results
A total of 62 patients with age ranging from 54 to 94 (mean 78.2; SD 09.11) years were evaluated. Out of them, 33 (53.2%) patients were females and 29 (46.8%) patients were males. There were 32 (51.6%) patients with left sided intertrochanteric femur fractures and 30 (48.4%) were right sided. A total of 33 (53.2%) patients sustained injury following trivial fall on ground, 16 (25.8%) patients sustained injury due to fall from height and 13 (21%) had road traffic accident. Of 62 cases studied, 12 (19.4%) cases were A1.1, 12 (19.4%) were A1.2, 8 (12.9%) were A1.3, 16 (25.8%) were A2.1, 8 (12.9%) were A2.2 and 6 (9.6%) were A2.3 as per the AO classification of intertrochantric fractures [14]. The mean time from injury to surgery was 6.34 days, ranging from 2 to 18 days (SD 3.79).
All the 62 cases were operated under lumbar spinal anaesthesia. All of them underwent closed reduction and fixation with PFNA with the help of fluoroscopic control.
Intraoperative Parameters [Table/Fig-2]:
Results of intraoperative parameters and time to union.
| Parameter | Amount | Number of patients | Percentage (%) |
|---|
| Time takenAverage time taken | <49 min50-59 min60-69 min70-79 min>80 min61.4 (Range 45-90, SD 11.6) min | 1012171607 | 16.1%19.4%27.4%25.8%11.3% |
| Amount of blood lossAverage amount of blood loss | <79 mL80-99 mL100-119 mL120-139 mL>140 mL103.9 (Range 60-200, SD 36.4) mL | 1613111408 | 25.8%21.0%17.6%22.6%13.0% |
| Flouroscopy timeAverage fluoroscopy time | <50 sec51-60 sec61-70 sec71-80 sec81-90 sec74.0 (Range 41-98, SD 13.5) sec | 1113171407 | 17.7%21.0%27.4%22.6%11.3% |
| Mean time to union | 16.1 (Range 12-24, SD 3.3) weeks | - | - |
Time taken: The average time duration of surgery was 61.4 (SD 11.6) minutes ranging from 45 to 90 minutes.
Amount of blood loss: The intraoperative blood loss ranged from 60 to 200 mL and the mean blood loss calculated was 103.9 mL (SD 36.4).
Fluoroscopy time: The average fluoroscopy time was 74.0 seconds (SD 13.5) and it ranged from 41 to 98 seconds.
Duration of follow-up: Average duration of follow-up was of 14.3 months and it ranged from 12 to 18 months (SD 2.05).
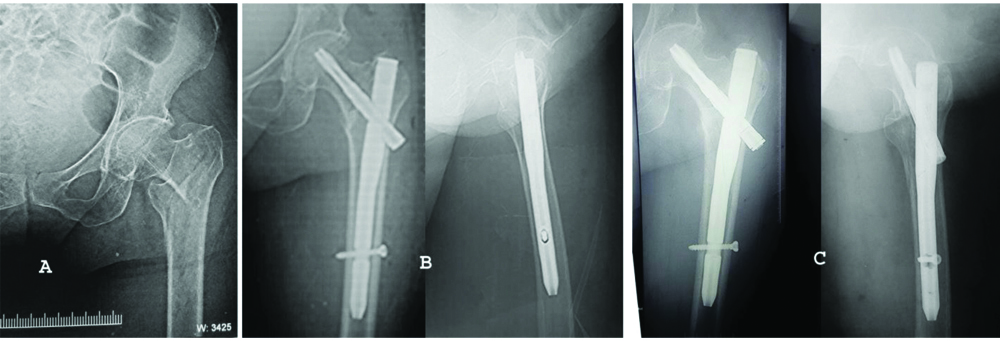
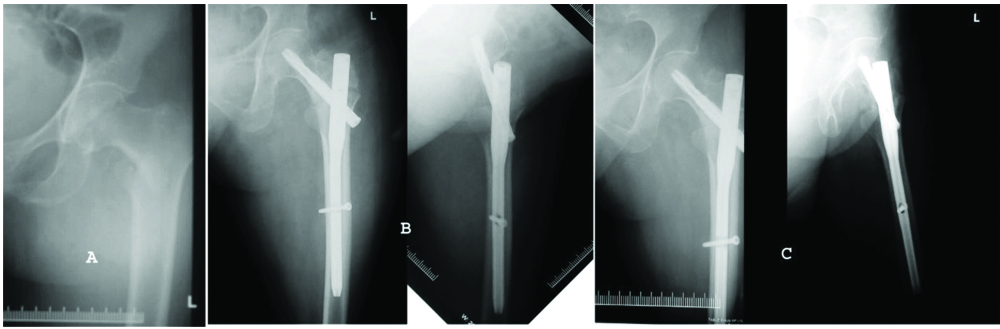
Time to union: No case of non-union was reported. The average time to union was 16.1 (SD 3.3) weeks and ranged from 12 weeks to 24 weeks [Table/Fig-2,3,4 and 5].
Functional evaluation: Final functional evaluation was done using the HHS at 12 months. Its mean value was 82.8 (SD 8.6) and ranged from 65 to 94 with 17 (27.4%) patients having excellent outcome, 29 (46.8%) having good outcome and 8 (12.9%) each had fair and poor outcome [Table/Fig-6].
Complications: All fractures united with a good implant component position and none of the patients had failure or breakage of the implant in the postoperative period. No case of deep infection was noted while superficial infection was seen in 4 cases which responded well to conservative management in all the cases. Screw cut-out or cut-through into the hip joint was also not observed in any of the case. Thirteen patients developed femoral shortening with 10 patients having it within 1 cm and 3 patients had >1 cm of femoral shortening. Varus collapse was observed in 3 patients. Other postoperative complications included, calcification at the tip of greater trochanter (n=4, 6.4%), sensitivity over Tensor Fasciae Latae (TFL) muscle (n=2, 3.2%), medial thigh pain (n=3, 4.8%) and none of these affected the functional outcome. None of the patients required a second surgery [Table/Fig-7].
Case 1: (a) Preoperative X-ray; (b) Postoperative X-ray; (c) X-ray after 12 weeks.
Case 2: (a) Preoperative X-ray; (b) Postoperative X-ray; (c) X-ray after 12 weeks.
Clinical outcome at 12 weeks follow-up.

Evaluation of Harris hip scores (HHS) at the final follow-up of 12 months.
| Grade | Score | Number of patients | Percentage (%) |
|---|
| Excellent | 90-100 | 17 | 27.4 |
| Good | 80-89 | 29 | 46.8 |
| Fair | 70-79 | 8 | 12.9 |
| Poor | <70- | 8 | 12.9 |
| Total | ~ | 62 | 100 |
Postoperative complications.
| Complications | Number of patients | Percentage (%) |
|---|
| Varus collapse | 3 | 4.8 |
| Calcification at tip of greater trochanter | 4 | 6.4 |
| Sensitivity over TFL | 2 | 3.2 |
| Medial thigh pain | 3 | 4.8 |
| Femoral shortness >1 cm | 3 | 4.8 |
Discussion
The incidence of unstable intertrochantric fractures is on rise and this trend is likely to persist. These fractures present a formidable challenge to an average orthopaedic surgeon. Osteosynthesis with dynamic hip screws or cephalomedullary nails is favoured and arthroplasty is resorted upon in selected cases. The choice of implant for their internal fixation is still contentious. Osteoporosis further compounds the outcome of these injuries [18]. Biomechanical studies have demonstrated that osteoporosis contributes significantly in screw migration in the proximal femur and thus leading to implant failure [19]. In a quest to boost the fixation, different techniques have been proposed including cement augmentation and amelioration in implant design [20]. The plethora of implants present in the market today bespeaks the evolving hunt for an ideal implant.
The inception of a helical blade device was one such attempt to emend the fixation of these fractures and relied upon their biomechanical ascendancy in the backdrop of osteoporosis [11]. The blade does not require reaming, thereby retaining the vital bone stock in the femoral head. The cancellous bone gets compacted during the insertion of the screw, affording an enhanced purchase as well as more resistance to varus collapse and rotational stress [21]. In this study with PFNA, authors reported a good functional outcome with 100% union rates accompanied with very few complications.
Present study consisted of 62 patients, out of whom 32 were A1 type (stable) and 30 were A2 type (unstable) intertrochanteric femur fractures as classified according to AO classification [11]. Sadic S et al., conducted retrospective study on 113 patients with majority, that is 75 (66%) patients were having unstable fracture types; of these, 51 were A2 (46%) and 24 were A3 (21%) [22]. Dominant subgroups were A1.2 (26.5%) and A2.3 (25.6%). Gavaskar A et al., conducted a prospective study to assess the results of 122 elderly patients with low velocity trochantric fractures {39-stable (AO; 31-A1) and 83-unstable (AO; 31-A2) and A3} treated with PFNA from December 2008 to April 2010 [21]. Follow-up functional and radiological assessments were done.
The average duration of surgery in this study ranged from 45-90 minutes with a mean duration of 61.4 (SD 11.6) minutes. Close reduction was achieved in 47 cases while the rest required minimal opening of the fracture site to allow reduction maneuvers using Hohmann retractors and reduction clamps. Kumar GN et al., reported it to be 32 minutes (range 18-90 minutes) [23]. In their study, closed reduction of the fracture was possible in 25 cases and rest was reduced with minimal opening of the fracture site. Pu JS et al., published the mean duration of surgery to be 53 minutes for A.2 fractures and 78 minutes for A.3 fractures [24].
There is a considerable variation in the amount of intraoperative average blood loss among various studies. In this study, it was 103.9 mL, ranging from 60-200 mL while Sadic S et al., reported it to be 22.8 mL (range 5-100 mL) while for Sahin S et al., it was 225 mL (range 150-450 mL) [22,25]; Pu JS et al., reported the mean blood loss to be 80 mL in A.2 fractures and 200 mL in A.3 fractures [24].
Fluoroscopy exposure of this study was comparable to that of findings by Sadic S et al., who required a mean 63 seconds intraoperative radiation exposures (range 13-148) while an average of 74 seconds exposures (range 41-98) was required in the present study [22]. Pu JS et al., and Lv C et al., claimed that the more unstable the fracture pattern is, more is the fluoroscopy time required [24,26]. Lv C et al., observed C-arm fluoroscopy control required a mean time of 113 seconds for fixing A2 fractures and 152 seconds for fixing A3 fractures [26] while for Pu JS et al., peroperative fluoroscopy screening took a mean time of 128 seconds for A2 fractures and 159 seconds for A.3 fractures [24]. Sadic S et al., suggested that repeated reduction and manipulation increases operative and fluoroscopy time and intraoperative blood loss, especially in more unstable fracture types [Table/Fig-8] [22].
Comparison of the results of different studies [22,24,25].
| Authors (Reference) | Duration of surgery (min) | Mean blood loss (mL) | Mean fluoroscopy time (sec) | Mean Harris hip scores |
|---|
| Our study | 61.4 | 103.4 | 74 | 82.8 |
| Sadic S et al., [22] | 73.1 | 22.8 | 63 | - |
| Pu JS et al., [24] | 53 (A2 fractures)78 (A3 fractures) | 80 (A2 fractures)200 (A3 fractures) | 128 (A2 fractures)159 (A3 fractures) | - |
| Sahin S et al., [25] | 37.8 | 225 | - | 77.8 |
The invent of PFNA has been claimed to reduce the various perioperative and postoperative complications while dealing with trochanteric fractures [27]. A 1% incidence of cutout was reported by Aguado-Maestro I et al., who claimed to have observed a reduced incidence of cut-through and cut-out with helical blades in pertrochantric fractures in their study of 200 patients and stressed that accurate placement of the helical blade is a crucial factor to prevent mechanical failure [28]. Cut out rates were found to be 3.5% by Sadic S et al., 4.7% by Sahin S et al., 4.2% by Takigami I et al., and 7.9% by Zhang H et al., [22,25,29,30]. Blade migration within the femoral head and telescoping of the blade along its long axis was seen in one patient by Sadic S et al., in their retrospective study on 113 patients [22]. Femoral head perforation has also been reported by Karapinar L et al., and Simmermacher RK et al., in 1.4% and 1.2% of their patients, respectively [31,32]. Authors did not observed any of these complications in this study.
Varus collapse was seen in 3 patients in this study (4.8%). Almost similar incidence was confronted by Yu W et al., (4.9%) in their study involving 225 cases [33] and by Zhang H et al., (5.8%) [30] while Radaideh AM et al., found it to be 12% and attributed it to inadequate reduction and/or poorly placed helical blade of the PFNA [34]. They also believed early functional exercise, high activity levels, increasing age and presence of osteoporosis to escalate the risk of implant failure.
Talking about the clinical outcomes in this study, the mean HHS at final follow-up was 82.8 (SD 8.6) points. It was comparable to that found by Sadic S et al., {79.3(SD 9.10)} points [22]. Zhang H et al., found it to be 72.4 (SD 7.2) in their study involving 139 PFNA treated cases [30]. In this series, 54 (81.1%) patients had excellent to fair results while 8 (12.9%) patients had poor results. The results were acceptable and comparable with the observations made by Sadic S et al., that had these figures to be 41 (82%) and 9 (18%), respectively [22]. Simmermacher RK et al., also observed restoration of preoperative mobility in 56% to 80% of their patients managed with PFNA [32].
Limitation(s)
This study, being done with a single group of patients, could not compare PFNA with other implants available for the treatment of the intertrochantric fractures. Moreover, being organised with a limited number of patients and in a short frame of time could not furnish insight into the long-term complications and hurdles with any revision surgery if required. Future trials that are comparative, ably outlined and appropriately powered are warranted.
Conclusion(s)
To conclude, it is inferred that PFNA can be recommended for fixation of both stable and unstable intertrochantric fractures. It may prove superior to other available implants in the setting of osteoporosis due to compaction of the cancellous bone around the helical screw. Ease in insertion, reduced operative time and blood loss, stable fixation, less complications and good functional and radiological outcome can make it an implant of choice for these fractures. Further studies with one control group, larger group size and longer follow-up are necessary to provide complete information and validate the findings of the current study.