Management of Ocular Surface Squamous Neoplasia in Association with Fungal Keratitis In an HIV Positive Individual
Prabhakar Singh1, Abhishek Gupta2, Richa Gupta3
1 Consultant, Department of Cornea and Anterior Segment, Nirwana Netralaya, Sasaram, Bihar, India.
2 Senior Resident, Department of Retina Services, IGIMS, Patna, Bihar, India.
3 Senior Resident, Department of Paediatric Services, IGIMS, Patna, Bihar, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prabhakar Singh, Nirwana Netralaya, Athkhambwa, Near Sai Baba Temple, Tarachandi Road, Sasaram, Bihar, India.
E-mail: prabhakar1aiims@gmail.com
Ocular Surface Squamous Neoplasia (OSSN) co-existent with fungal keratitis in an immunodeficient individual has rarely been talked about in literature. Risk factors for fungal keratitis are trauma with vegetative matter, topical steroid abuse, poor ocular surface, corneal anaesthesia, systemic immunosuppression, etc., and for OSSN a major risk factor is immunodeficiency. In current report, patient had multiple risk factors. This report highlights the management of HIV positive 42-year-old male with OSSN and fungal keratitis. A comprehensive evaluation helps clinician decide on treatment priority and achieve good clinical outcome.
Conjunctiva, Immunodeficiency, Interferon alpha-2b, Leukoplakic
Case Report
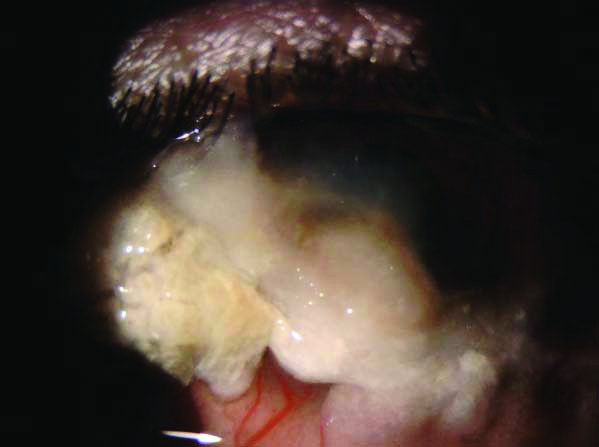
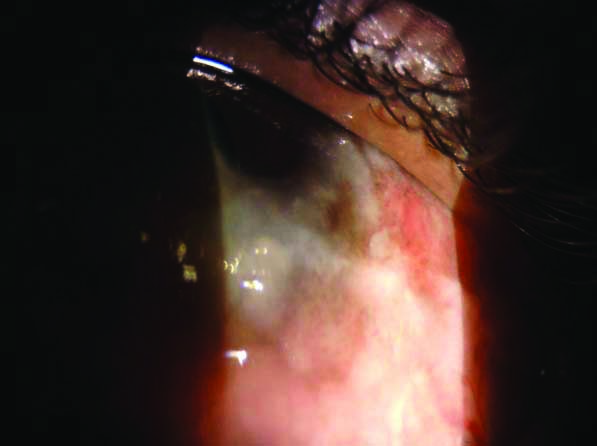
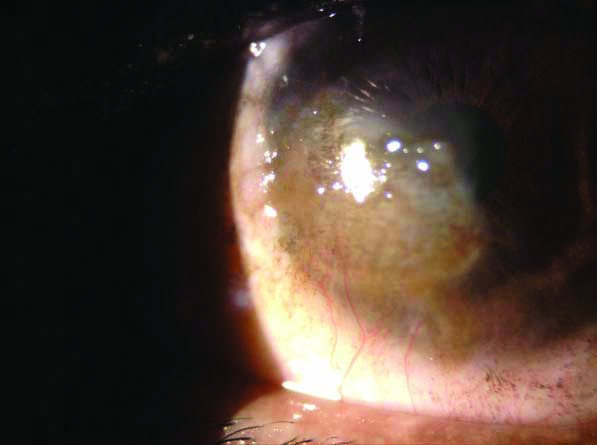
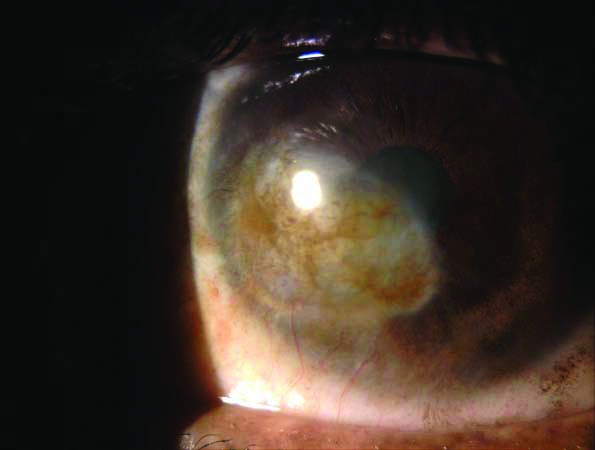
A 42-year-old male presented to the ophthalmic clinic with complaints of whitish growth over the cornea of the left eye for 4 months. It started as a painless, small lesion at the limbus that progressed over three months to encroach the cornea. Patient used topical medications (topical steroids) without proper medical advice. He sought ophthalmology consultation only when it became painful with significant decrease in visual acuity for one month. His visual acuity at presentation was 20/20 in the right eye and 20/600 in the left eye. On examination, a large, mixed, leukoplakic (overlying cornea, inferior and inferonasal limbus; H4.5*V6.5 mm) and papillomatous (Inferior and temporal bulbar conjunctiva; H4*V14 mm) mass was noted with overhanging keratin, straddling nasal and inferonasal limbus [Table/Fig-1]. Multiple dilated and tortuous feeder vessels were noted. The inferior and temporal bulbar papillomatous lesions were taking up rose-bengal stain and highlighting the extent of involvement [Table/Fig-2]. All fornices were unaffected on gross examination on slit-lamp. Pre-auricular and submandibular lymph nodes were not enlarged. Clinical features of lesions were very suggestive of OSSN. Ulcerative lesion was noted in the cornea, involving the visual axis. The infiltrates size was 4*3.5 mm (H*V) in dimension, involving more than two-third of corneal thickness, and had feathery edges. The patient was enquired about high-risk behaviour and was found to be positive for HIV1 and HIV2 on screening. Left eye corneal scraping was done and the direct smears with Grams staining and 10% KOH showed plenty of septate, hyaline fungal filaments. Topical Natamycin (5%) was started hourly along with topical homatropine (2%). Oral ketoconazole 200 mg was started twice daily for 2 weeks after obtaining a normal liver function test. The patient was asked to return to the clinic after 1 week. The patient was counseled about the condition and referred for HAART therapy. His CD4 counts were done at district health facility and were found to be 470 cells/cu.mm. The patient was administered with HAART therapy. It took almost a month for the fungal ulcer to resolve completely. Once the corneal scar was evident patient was re-evaluated and ASOCT was done to look for extent of disease. The disease largely appeared confined to epithelial layer on ASOCT and thus the patient was started on topical interferon alfa 2b (1MIU/cc) (1cc prefilled syringe of Intalfa 3 MIU, manufactured and marketed by Intas Pharmaceuticals Ltd., India) in a dose of 1 drop 4 times a day. Initially, the patient was reviewed every week to see recurrence if any. Subsequently, the patient was followed-up every 3 weeks. Bulbar papillomatous lesions started resolving after 2 weeks of commencement of topical interferon-alpha 2b. Stippled conjunctival pigmentation was noted over the bulbar region where the OSSN had resolved. By the end of three months, all bulbar lesions were completely resolved; however, limbal and corneal lesions were persisting [Table/Fig-3]. Though significant improvement was noted for corneal lesions also. By the end of five months, all lesions had resolved completely [Table/Fig-4]. However, topical interferon-alpha 2b was continued for one more month. By now the patient has completed 1.5 years of follow-up with no recurrence.
Showing the Ocular Surface Squamous Neoplasia mass straddling nasal and inferonasal limbus (leukoplakic) with overhanging keratin and resolving –corneal infiltrate in the visual axis.
Showing papillomatous ocular surface squamous neoplasia involving temporal and inferior bulbar conjunctiva.
Showing persistent corneal lesion by the end of three months, on interferon-alpha 2b.
Showing complete resolution of lesion.
Discussion
OSSN and fungal keratitis are two different clinical entities and their association has rarely been talked about in literature. However, HIV positivity was noted in 38-41% of patients with OSSN and surprisingly 70% of them were unaware of their status [1].
Risk factors for fungal keratitis are trauma with vegetative matter, topical steroid abuse, poor ocular surface, corneal anaesthesia, systemic immunosuppression, etc., [2,3]. In the current report, the patient had multiple risk factors like, previous use of topical steroids, poor ocular surface and HIV positive status. This report highlights the management of OSSN and fungal keratitis in an HIV positive individuals.
OSSN is the first presenting feature in HIV/AIDS in 50-86% of patients, in Africa [4-6]. We have learned that poor ocular surface, systemic immunosuppression, chronic topical steroid abuse, corneal anaesthesia are the predisposing factors for fungal corneal ulcers. Index patient had 3 out of the 4 factors discussed above. Another plausible explanation for the development of fungal corneal ulcers could be persistent tear film distribution abnormality due to OSSN. This might have resulted in Dellen formation. Non resolution of the OSSN resulted in epithelial breakdown and ulcer formation. This ulceration is likely to be sterile to start with and must have got secondarily infected with fungus, considering its widespread prevalence and presence of other risk factors.
There is one report of concurrent OSSN and fungal keratitis in literature. In this report, the eye could not be salvaged and extended enucleation had to be done [7]. In their report, the patient had pre-existing fungal keratitis; OSSN developed during treatment for fungal keratitis. In the current report, the patient had pre-existing untreated OSSN and he developed fungal keratitis subsequently. Here, considering already compromised ocular surface with involved nasal and inferonasal limbus and extensive involvement of bulbar region also, the patient was started on topical interferon-alpha 2b rather than using other modalities like MMC or FFU. There are other modalities described in literature like topical Cidofovir, photodynamic therapy etc., [8,9].
Immunomodulators still can have role in HIV positive patients, provided their CD4 counts are reasonably within normal range.
Studies with a larger sample size should be done to address the following questions: Formulate timing between stoppage of topical anti-fungal and commencement of interferon. Can both be treated simultaneously? Is delay in treatment for OSSN compromising prognosis? and Does corneal stromal melt due to corneal ulcer facilitates intraocular spread of OSSN?
Conclusion(s)
A comprehensive evaluation is very important in cases with co-existent immunodeficiency, OSSN, and superadded fungal keratitis before going for treatment. In present case, authors treated fungal keratitis first and then OSSN. We ensured commencement of HAART therapy and this also probably contributed to better outcome.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 18, 2020
Manual Googling: Nov 10, 2020
iThenticate Software: Jan 15, 2021 (5%)
[1]. Kaliki S, Kamal S, Fatima S, Ocular surface squamous neoplasia as the initial presenting sign of human immunodeficiency virus infection in 60 Asian Indian patientsInt Ophthalmol 2017 37(5):1221-28.10.1007/s10792-016-0387-027826936 [Google Scholar] [CrossRef] [PubMed]
[2]. Harissi-Dagher M, Colby K, Fungal infections of the corneaContemp Ophthalmol 2006 5:01-08. [Google Scholar]
[3]. Rosa RH, Miller D, Alfonso EC, The changing spectrum of fungal keratitis in south FloridaOphthalmology 1994 101:1005-13.10.1016/S0161-6420(94)31225-5 [Google Scholar] [CrossRef]
[4]. Osahon AI, Ukponmwan CU, Uhunmwangho OM, Prevalence of HIV seropositivity among patients with squamous cell carcinoma of the conjunctivaAsian Pac J Trop Biomed 2011 1(2):150-53.10.1016/S2221-1691(11)60015-4 [Google Scholar] [CrossRef]
[5]. Porges Y, Groisman GM, Prevalence of HIV with conjunctival squamous cell neoplasia in an African provincial hospitalCornea 2003 22(1):01-04.10.1097/00003226-200301000-0000112502938 [Google Scholar] [CrossRef] [PubMed]
[6]. Spitzer MS, Batumba NH, Chirambo T, Bartz-Schmidt KU, Kayange P, Kalua K, Ocular surface squamous neoplasia as the first apparent manifestation of HIV infection in MalawiClin Exp Ophthalmol 2008 36(5):422-25.10.1111/j.1442-9071.2008.01794.x18939345 [Google Scholar] [CrossRef] [PubMed]
[7]. Singh S, Mittal R, Narang P, Mittal V, Ocular surface squamous neoplasia in a setting of fungal keratitis- A rare co-occurrenceInt Ophthalmol 2019 39(3):717-20.10.1007/s10792-018-0864-829423784 [Google Scholar] [CrossRef] [PubMed]
[8]. Ip MH, Coroneo MT, Treatment of previously refractory ocular surface squamous neoplasia with topical cidofovirJAMA Ophthalmol 2017 135(5):500-02.10.1001/jamaophthalmol.2017.036528358964 [Google Scholar] [CrossRef] [PubMed]
[9]. Cekic O, Bardak Y, Kapucuoglu N, Photodynamic therapy for conjunctival ocular surface squamous neoplasiaJ Ocul Pharmacol Ther 2011 27(2):205-07.10.1089/jop.2010.011321417754 [Google Scholar] [CrossRef] [PubMed]