The AH is the most common surgery performed which is mainly equipped for benign as well as malignant indications [1]. The extent of pain as well as the length of the period of convalescence associated with hysterectomy depends on the surgical approach. The open AH is related to medium to high pain level and is considered a major surgery [2]. AH is associated with severe postoperative pain [1]. Multimodal pain management program is needed to control pain after AH which is considered as one of the major abdominal surgeries in gynaecology [2]. Pain management is a challenging task in these surgeries leading to favourable outcome in patient satisfaction.
Postoperative pain is a well-known distressing factor and can affect patient’s recovery and mobilisation. Much has been talked about the pathophysiology of pain and many newer modalities have been discovered to combat postoperative pain [3]. There are several analgesic options for abdominal surgeries like systemic analgesia, local infiltration, regional analgesia and abdominal nerve blocks [4]. A number of newly discovered peripheral blocks such as blocks of the anterior abdominal wall like ultrasound guided TAP block and QL block have become popular for postoperative analgesia [5]. These truncal blocks reduce the requirement for opioids and other analgesics. Use of ultrasound increases the effectiveness of these blocks by delineating the anatomy better and increasing the efficacy of these blocks [5].
The TAP block first described by Rafi AN is a landmark based technique within ilio-lumbar triangle of Petit and is indicated in surgical procedures involving anterior abdominal wall like laparoscopic cholecystectomy, open appendicectomy, caesarean section and other procedures [6]. The QL block is a recently developed new technique in the domain of peripheral nerve blocks involving the nerves of the anterior abdominal wall and was first described by Blanco R [7]. It provides a dermatome sensory block of the lower six thoracic and first lumbar afferents. A recent study has shown that QL block provides better somatic and visceral analgesia than TAP block [8]. The aim of the study was to compare the analgesic efficacy of QL block with that of TAP block. The primary outcome was the time of first analgesic requirement and total dose of analgesic required in 24 hours. The secondary outcome were the haemodynamic changes associated with the blocks, patient satisfaction score at the end of 24 hours and any complications that arise due to the blocks.
Materials and Methods
After obtaining approval from Institutional Ethics Committee (Ref.no: 752/UPUMS/Dean/2019-20/E.C/2019-20), this double blind randomised clinical trial was conducted from June 2017 to January 2019 in the Department of Anaesthesiology in Uttar Pradesh University of Medical Sciences, Etawah. Written and informed consent from each patient was taken after explaining the study procedure.
The study was conducted in gynaecology operation theatre in patients undergoing elective total AH.
Inclusion criteria: Patients of American Society of Anaesthesiologists (ASA) grade I and II of age group between 35-65 years with BMI between 18-30 kg/m2 were included in the study.
Exclusion criteria: Patients with coagulopathy, localised infection at the proposed site, inability to comprehend the scoring systems, known allergy to drugs used, opioid dependence, renal, hepatic or cardiorespiratory impairment or any neurological disorder were excluded from the study.
Sample Size Calculation
The sample size was calculated on the basis of a pilot study done in the three groups with a difference in mean score of 2. Using the power of study 80%, confidence interval 95% and an alpha error of 0.05, the sample size came out to be 105 divided into three groups of 35 patients each.
A random number table for 105 patients was divided into three groups and sequentially numbered opaque sealed envelopes were prepared and patients were divided according to the envelope randomly. The anaesthesiologist who administered the block was not involved in uncoding the data. The changes in haemodynamic variable as well as VAS score was recorded by another anaesthesiologist who was blinded to the technique of the block or drug used. The description of VAS score was explained to the patient prior to giving the block.
The three groups were as follows:
Group Q: Patients in group Q received QL block with 40 mL of 0.25% Bupivacaine (n=35) in which 20 mL of drug was injected on either side.
Group T: Patients in group T received TAP block with 40 mL of 0.25% Bupivacaine (n=35) in which 20 mL of drug was injected on either side.
Group C: Patients in group C received no block (n=35).
Study Procedure
All patients received Tab Ranitidine 150 mg and Tab Alprazolam 0.25 mg at night and morning before surgery. The vital parameters {Heart Rate (HR), Blood Pressure (MAP), saturation and Respiratory Rate (RR)} were checked in the preoperative room. In operation theatre, peripheral vascular access was obtained with an 18-gauge (G) intravenous cannula in all patients and 10-15 mL/kg Ringer Lactate infusion was started. After taking full aseptic precautions, the surgery was performed under spinal anaesthesia with 3 mL 0.5% hyperbaric bupivacaine in L3-L4 intervertebral space with 25G Quincke’s needle in sitting position. Blood pressure, HR, and peripheral oxygen saturation (SpO2), Electrocardiogram (ECG) values were monitored by non-invasive methods in all patients throughout the intraoperative and postoperative period. If there was any fall in MAP and HR more than 20% of the baseline, then it was effectively treated with inj.Mephentermine 6 mg i.v and inj. Atropine (200 mcg) respectively.
After the completion of surgery, the sensory level before applying the respective blocks was checked by cold spray method and then the proposed blocks were administered using 18G Tuohy needle under ultrasound guidance (a SonoSite M-Turbo ultrasound machine using a curvilinear 2-5MHz sterile transducer).
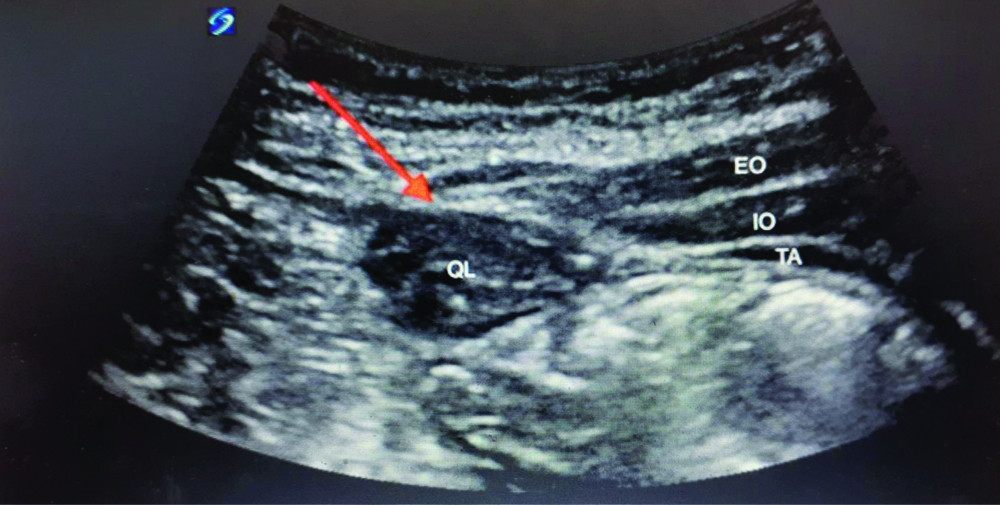
In group Q patients, a Transmuscular QL block [Table/Fig-1] was performed by first positioning the patient in lateral decubitus position. Then after all aseptic precautions, the curvilinear transducer probe was placed on posterior axillary line, between 12th rib and iliac crest. After identification of External Oblique (EO), Internal Oblique (IO) and Transversus Abdominis (TA) muscle and then tracing them backwards and caudally the QL muscle was identified by shamrock sign, which consists of the transverse process of L4 vertebra as the “stem” and psoas major, QL and erector spinae as “3 cloves of the shamrock” [9]. As soon as it was identified, then using a blunted tip 18G tuohy needle and after negative aspiration of blood the block was applied in plane of the muscle and 20 mL of 0.25% bupivacaine was administered and similar process was repeated on other side.
Ultrasound guided Quadratus lumborum block.
EO: External oblique; IO: Internal oblique; TA: Transversus abdominis; QL: Quadrates lumborum
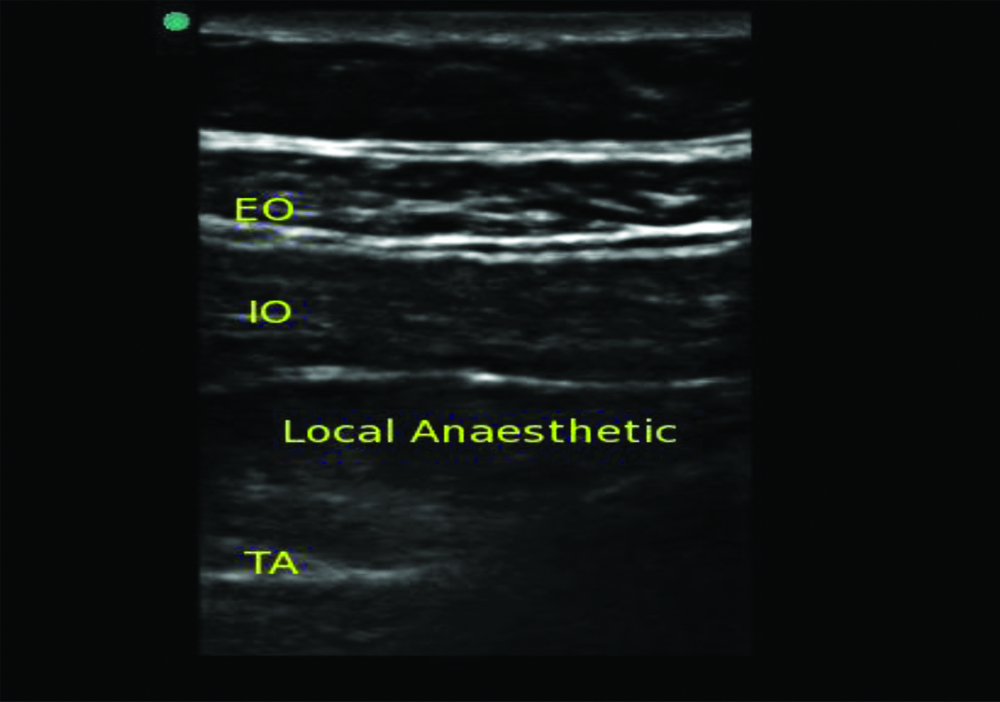
In group T patients, similarly after taking all aseptic precautions, a TAP block as depicted in [Table/Fig-2] was performed in supine position by placing linear ultrasound probe in a transverse plane between the lower costal margin and the iliac crest. Then, TA muscle was identified below EO and IO and then 20 mL of 0.25% of bupivacaine was deposited in the plane on either side with intermittent aspiration. In control group C, no block was given. Postoperative pain was assessed by an independent observer and evaluated by VAS, a scale of zero to ten, where zero is no pain and 10 is very severe pain.
Ultrasound guided transversus abdominis block.
EO: External oblique; IO: Internal oblique; TA: Transversus abdominis
In all the three groups, the time after administration of block was time zero, VAS at time zero was the baseline score after block and was recorded in all patients. If patient experienced intensity of pain which was more than three in VAS, then intramuscular injection diclofenac 75 mg was administered and if this was not sufficient, then injection tramadol (100 mg) was given intravenously and if this was also inadequate then analgesia with morphine (0.1 mg/kg) intravenously upto maximum of 5 mg was administered. Diclofenac upto maximum of 150 mg and tramadol upto maximum of 400 mg was being administered in 24 hours. Patient’s pain was evaluated at the 0, 15, 30 minutes, 1 hour, 2 hour, 6th hour, 12th hour and 24th hour upto 24 hours after block.
Patient’s satisfaction score was assessed using a seven point Likert verbal rating scale [10] after 24 hours as depicted in [Table/Fig-3].
Likert verbal rating scale.
| 1 | Extremely dissatisfied |
| 2 | Dissatisfied |
| 3 | Somewhat dissatisfied |
| 4 | Undecided |
| 5 | Somewhat satisfied |
| 6 | Satisfied |
| 7 | Extremely satisfied |
The haemodynamic parameters like HR, MAP, SpO2, RR were taken after the block and patients were monitored upto 24 hours after the block. The time of first analgesic demand (taken as first postoperative analgesic agent administration after application of block), dose of analgesic required, dose of additional analgesic (tramadol) required, total analgesic requirement in 24 hours and complications after giving block (nausea, vomiting, hypotension, and headache) were recorded.
Statistical Analysis
Quantitative data are represented as mean±Standard Deviation (SD). Categorical data is represented as number of patients. Physical characteristics, HR, MAP, onset and duration of block, time of first analgesic demand, all were compared using the unpaired t-test. Categorical data was compared using Chi-square test. Adverse effect profile was compared using Fisher’-exact test. The p-value <0.05 was considered to be significant. All the statistical calculation was done by the statistician using software SPSS version 16 (Chicago, IL, USA).
Results
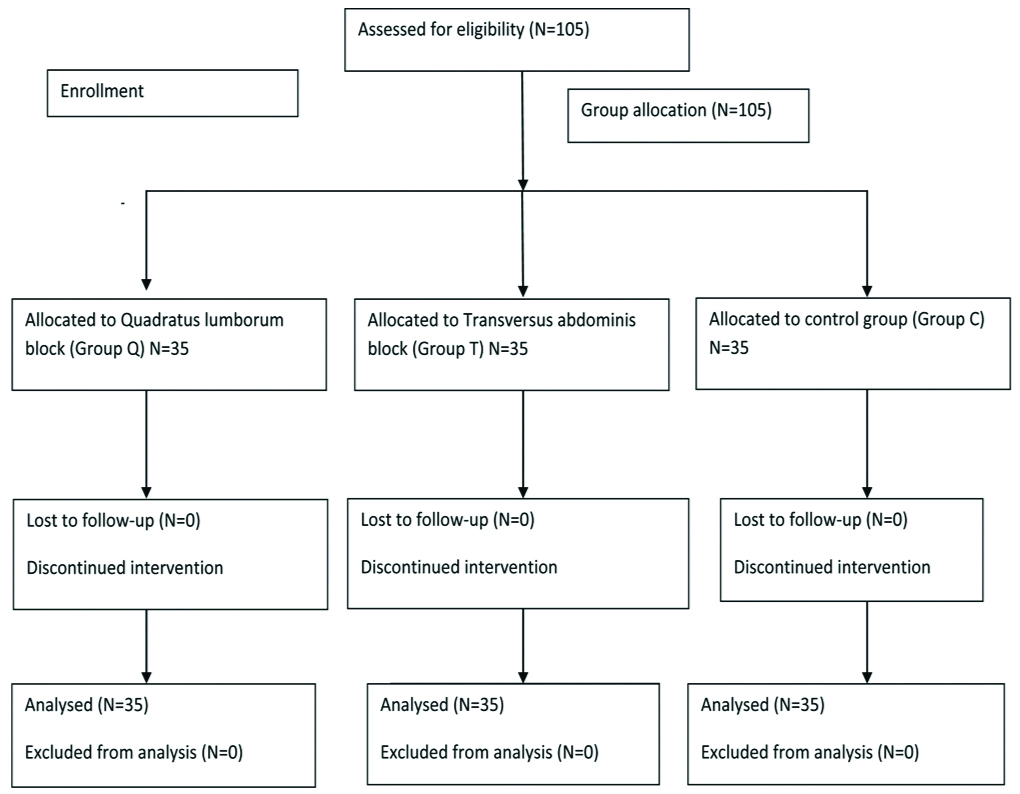
The study population comprised of 105 patients posted for total AH and was allocated into three groups of 35 patients each as shown in [Table/Fig-4].
Consort flow diagram.
Group Q: Quadratus lumborum; Group T: Transversus abdominis; Group C: Control
The three groups were similar with regard to demographic characteristics like age, BMI, duration of surgery and ASA physical grade [Table/Fig-5].
Demographic characteristics and operative data.
| Characteristics | Group Q | Group T | Group C | p-value |
|---|
| Age (Years) (Mean±SD) | 42.54±5.11 | 42.80±5.83 | 41.69±7.52 | 0.73 |
| BMI (kg/m2) (Mean±SD) | 23.64±1.98 | 23.52±1.46 | 23.23±1.21 | 0.53 |
| Duration of surgery (min) (Mean±SD) | 104.43±17.05 | 103.14±15.43 | 103.71±16.05 | 0.94 |
| ASA (I:II) | 28:7 | 27:8 | 25:10 | 0.69 |
BMI: Body mass index; SD: Standard deviation; p<0.05 Significant; ASA: American society of anesthesiologists
Haemodynamic parameters such as HR, MAP, respiratory rate and SpO2 postoperatively were comparable among all the three groups at all time periods.
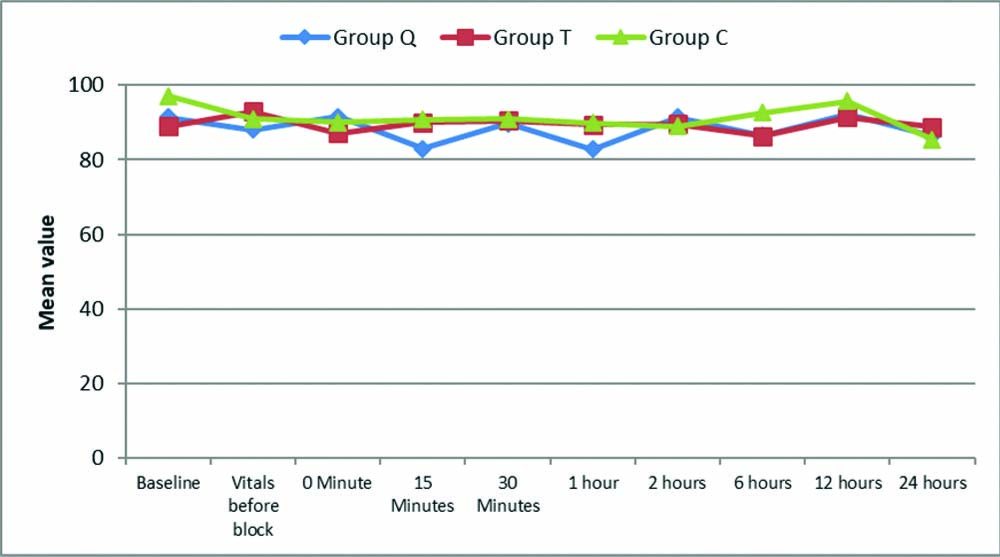
[Table/Fig-6] shows the comparison of HR (beats/minute) among the groups across the time periods. The analysis of variance showed that there was no significant (p=0.52) difference in HR among the groups at all the time periods.
Comparison of Heart Rate (HR) (beats/minute) among the groups across the time periods.
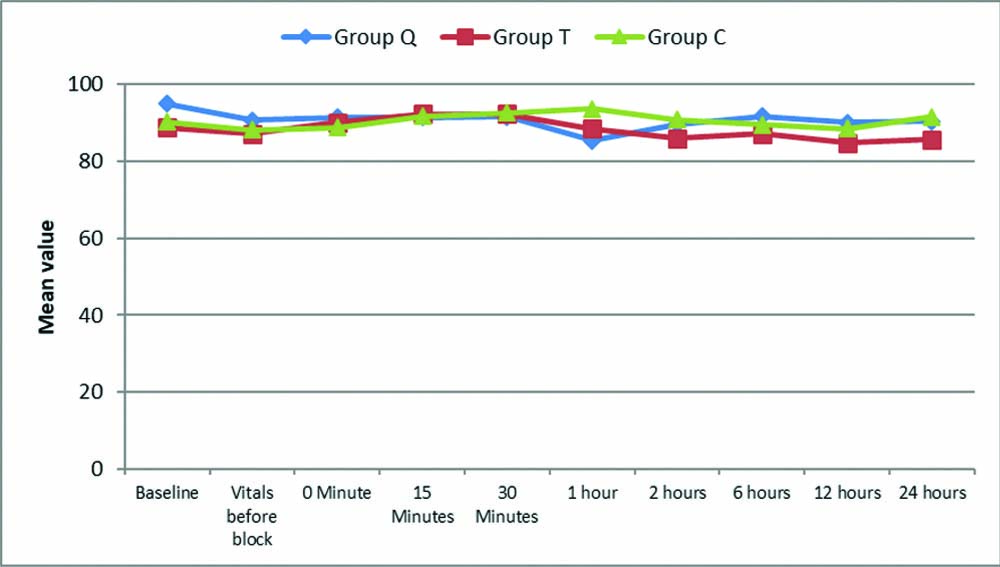
[Table/Fig-7] shows the comparison of MAP among the groups across the time periods. The analysis of variance showed that there was no significant (p=0.25) difference in MAP among the groups at all the time periods.
Comparison of Mean Arterial Pressure (MAP) among the groups across the time periods.
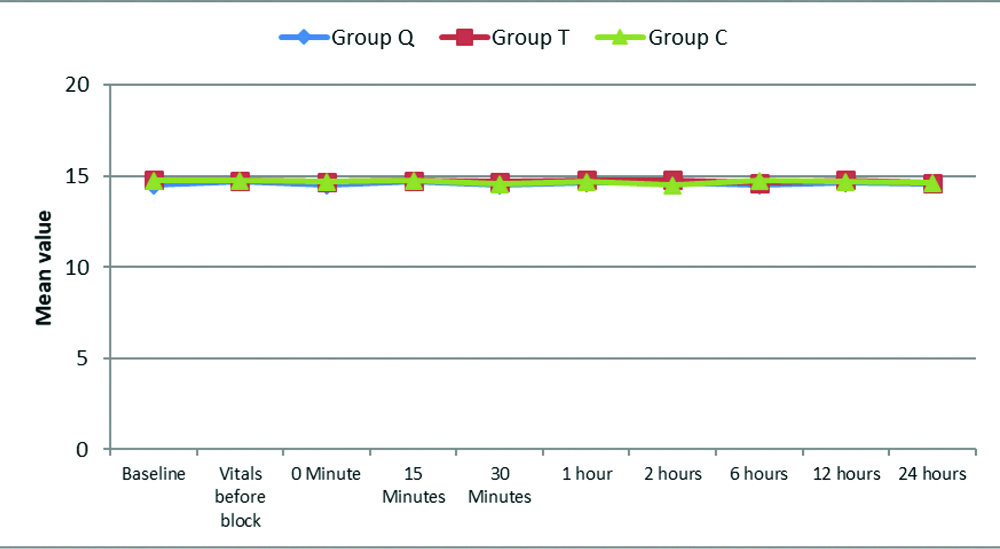
[Table/Fig-8] shows the comparison of RR among the groups across the time periods. There was no significant (p=0.76) difference in RR among the groups at all the time periods.
Comparison of respiratory rate among the groups.
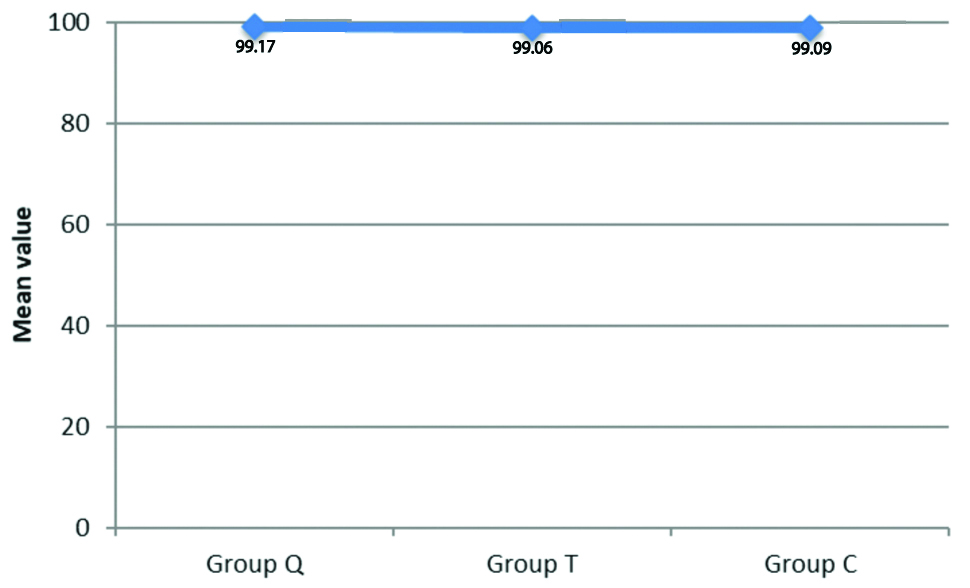
[Table/Fig-9] shows the comparison of SpO2 among the groups. The analysis of variance showed that there was no significant (p=0.67) difference in SpO2 among the groups.
Comparison of SpO2 among the groups.
VAS at the time of application of block was zero. The VAS scores were significant at all time intervals among the three groups [Table/Fig-10]. On comparison of the groups Q and T, VAS scores were significant at 2nd and 6th hour with p-value of 0.003 and 0.001, respectively.
VAS scores among the groups across the time periods.
| Time periods | Group Q (n=35) | Group T (n=35) | Group C (n=35) | p-value1 | p-value2 |
|---|
| Q vs T | Q vs C | T vs C |
|---|
| Baseline | 0.00±0.00 | 0.00±0.00 | 0.00±0.00 | - | - | - | - |
| Vitals before block | 0.00±0.00 | 0.00±0.00 | 0.00±0.00 | - | - | - | - |
| 0 Min | 0.00±0.00 | 0.00±0.00 | 0.00±0.00 | - | - | - | - |
| 15 Min | 0.00±0.00 | 0.00±0.00 | 0.00±0.00 | - | - | - | - |
| 30 Min | 0.00±0.00 | 0.00±0.00 | 1.06±0.83 | - | - | - | - |
| 1 hour | 0.00±0.00 | 0.03±0.16 | 3.63±1.06 | - | - | - | 0.001* |
| 2 hours | 0.34±0.53 | 1.03±1.01 | 3.86±0.94 | 0.001* | 0.003* | 0.001* | 0.001* |
| 6 hours | 2.46±1.19 | 3.89±0.79 | 4.63±0.49 | 0.001* | 0.001* | 0.001* | 0.02* |
| 12 hours | 3.97±0.66 | 3.71±0.66 | 4.46±0.61 | 0.001* | 0.22 | 0.006 | 0.001* |
| 24 hours | 3.66±1.30 | 3.91±0.78 | 4.61±0.71 | 0.02* | 0.51 | 0.01* | 0.02* |
1ANOVA test, 2Post-hoc tests, *Significant
The demand for first analgesic was significantly early in Group C with mean value of 1.37±0.74 hours and it was 4.63±0.97 hours in Group T and 7.77±1.51 hours in Group Q [Table/Fig-11]. The demand for diclofenac was same in all the three groups but the demand for tramadol was greater in group T and control group. The number of patients requesting tramadol as additional analgesic was higher in group T and much higher in control group.
Time of first analgesic requirement among the groups (in hours).
| Groups | Time of first analgesic used (Mean±SD) |
|---|
| Group Q | 7.77±1.51 |
| Group T | 4.63±0.97 |
| Group C | 1.37±0.74 |
| p-value1 | 0.0001* |
| p-value2 |
| Q vs T | 0.0001* |
| Q vs C | 0.0001* |
| T vs C | 0.0001* |
1ANOVA test, 2Post-hoc tests, *Significant; SD: Standard deviation
The number of patients requesting tramadol as additional analgesic was higher in group T and much higher in control group. In this study in the group Q, only five patients out of 35 required tramadol i.v in a dose of 100 mg as additional analgesic. In group T, 34 patients required i.v tramadol in a dose of 100 mg while in the control group all the 35 patients required tramadol i.v in a dose of 200 mg.
There was significant (p=0.0001) difference in patient satisfaction between group Q and C and group T and C but no significant difference in patient satisfaction was observed between group Q and T (p=0.97) [Table/Fig-12]. There was no significant (p>0.05) difference in complications among the three groups with a p-value of 0.51 [Table/Fig-13].
Patient satisfaction among the groups.
| Groups | Patient satisfaction (Mean±SD) |
|---|
| Group Q | 5.94±0.23 |
| Group T | 5.91±0.28 |
| Group C | 3.94±0.90 |
| p-value1 | 0.0001* |
| p-value2 |
| Q vs T | 0.97 |
| Q vs C | 0.0001* |
| T vs C | 0.0001* |
1ANOVA test, 2Post-hoc tests, *Significant; SD: Standard deviation
Complications among the groups.
| Complications | Group Q (n=35) | Group T (n=35) | Group C (n=35) | p-value1 |
|---|
| No. | % | No. | % | No. | % |
|---|
| Vomiting | 3 | 8.6 | 3 | 8.6 | 1 | 2.9 | 0.51 |
| Shivering | 0 | 0.0 | 1 | 2.9 | 0 | 0.0 |
| Nil | 32 | 91.4 | 31 | 88.6 | 34 | 97.1 |
1Chi-square test
Discussion
In this study, the significant finding was that QL block had reduced VAS scores when compared to TAP block at 2nd and 6th hour postoperatively. The time for first analgesic demand was prolonged in group Q than group T with mean duration of 7.77±1.51 hours in group Q and 4.63±0.97 hours in group T (p=0.0001). The total analgesic requirement was lower in group Q and the number of patients requesting additional analgesic in the form of tramadol was also lower in group Q in comparison to group T. Patients in group Q and T were more satisfied than patients of control group, but both groups Q and T were comparable in terms of patient satisfaction.
The results in this study were similar to the study done by Kumar GD et al., which compared QL block and TAP block in 70 patients using ropivacaine [11]. Pain assessment was done using Numeric pain intensity scale and it was found that QL block reduced pain scores and total analgesic requirement than TAP block. The time for first analgesic demand was also later in QL group. Another study done by Yousef NK, in 2018 showed similar results where TAP block was compared with QL block in total AH patients under general anaesthesia [12]. Here also, total analgesic requirement was reduced in QL group when compared to TAP group and duration of analgesia was prolonged in QL group (15.1±2.12 h vs. 8.33±4 h, p=0.001).
Verma K et al., in 2018 conducted a study in 60 patients comparing QL block versus TAP block for post caesarean analgesia and concluded that time for rescue analgesic requirement was higher in QL group than TAP group (mean±SD: 68.77±1.74 h vs. 13.3±1.21 h) (p<0.001) [13]. In a study done by Kumar GD et al., comparing QL block and TAP block in patients undergoing laparoscopic bariatric surgeries concluded that VAS scores were lower in QL group and higher in TAP group (p<0.02) and also time for first analgesic demand was more in QL group (p<0.001) and total analgesic consumption was also lower in QL group (p<0.001) [11]. The results are similar to the present study. Baidya DK et al., conducted a study on QL block as an effective method of perioperative analgesia in children undergoing pyeloplasty and concluded it as an effective technique of perioperative analgesia [14]. Murouchi T et al., conducted a study on 11 patients scheduled for laparoscopic ovarian surgery under general anaesthesia [15]. The patients received bilateral single injection QLB (20 mL of 0.375% Ropivacaine per side). It was concluded that QL block resulted in a widespread and long lasting analgesic effect upto at least 24 hours after laparoscopic ovarian surgery. In another study conducted by Blanco R et al., comparing QL block and TAP block in patients undergoing elective caesarean section for postoperative pain relief, patients in the QL block used less morphine than the TAP block group (p<0.05) at 6, 12, 24 and 48 hours after cesarean delivery [8].
The mechanism of prolonged analgesic effect of QL block is still unclear. While there are many theories, the most prominent one state that there is a paravertebral spread of local anaesthetic in case of QL block leading to visceral pain relief [8]. Another theory states that the QL block provides extensive analgesia from T7 to L1 dermatomes probably due to the spread of local anaesthetic into the paravertebral space or in the thoracolumbar plane that contains mechanoreceptors and multiple sympathetic fibres, thus contributing to extensive somatic and visceral analgesia [16]. In case of TAP block, it is postulated that it blocks the thoracolumbar nerves T10 to L1 and provides adequate somatic analgesia with little or no visceral blockade [5]. In 2011, Carney J et al., showed that contrast spreads from the L1-T5 segment of the paravertebral space [17].
In this study, patient satisfaction was assessed using a seven point Likert verbal rating scale after 24 hours. There was no difference in patient satisfaction between groups Q and group T (p=0.97). The patients of both groups Q and T block were more satisfied than the control group with the blocks for postoperative analgesia. With regard to adverse effects like nausea, vomiting and shivering all the three groups were comparable (p=0.51).
Limitation(s)
Ultrasound Sonography Test (USG) guided needle placement is an operator dependent technique and other technical problems encountered during the study were the need of assistance to position the patients in lateral decubitus on both sides in order to perform bilateral injections in the group QL group. Moreover, ultrasound visualisation was also difficult sometimes for the same reason. Other limitations in present study included that we evaluated only single-injection technique for both QL and TAP blocks.
Conclusion(s)
From the observations and analysis of the present study, it can be concluded that analgesic efficacy of QL block is better than TAP block as it prolonged the duration of first analgesic demand and reduced total analgesic consumption in 24 hours. Hence, QL block is a better postoperative analgesic technique than TAP block in patients undergoing total AH.
BMI: Body mass index; SD: Standard deviation; p<0.05 Significant; ASA: American society of anesthesiologists
1ANOVA test, 2Post-hoc tests, *Significant
1ANOVA test, 2Post-hoc tests, *Significant; SD: Standard deviation
1ANOVA test, 2Post-hoc tests, *Significant; SD: Standard deviation
1Chi-square test