Maxillary anterior spacing or midline diastema is the most frequently seen aesthetic concern for patients. This is attributed to the multitudes of interdependent or independent underlying aetiological factors associated with it [1]. Among the various aetiological factors for MMDs affecting children, the physiological (developmental) self-limiting diastema is the most common [2]. The mixed dentition stage is defined as an age at which both deciduous and secondary teeth have erupted in the oral cavity. Often, this period is prone to localised factors that may result in severe malocclusion problems if undetected. This phase of mixed dentition is often reported to be self-correcting with the eruption of maxillary canines [2]. Many researchers [3-5], like Broadbent BH [6], consider MMDs as an ‘ugly duckling stage’ and explain this phase as a transitional phase in the dental development. However, MMDs unrelated to the eruption of teeth has been observed owing to dental defects such as mesiodens [7,8], anodontia, hypodontia or microdontia of teeth especially upper lateral incisors, central incisor tooth discrepancies such as ankylosis, flaring or rotation [9], muscular defects like macroglossia [10], pernicious habits like thumb sucking, mouth breathing, tongue thrusting, lip biting [9,11], abnormal labial frenum attachment [9,12], dentoalveolar discrepancies [13], genetics [14], and certain midline pathologies [9].
There can be a significant disparity in the aesthetic perception from person to person and is greatly influenced by their personal experience and social environment [15-18]. Dentists are generally more sensitive to midline deviations than the general population even at 1 mm discrepancy [19,20]. A previous study described more than 1 mm as the threshold for dentists to notice midline deviation [21]. However, MMD’s up to 4 mm were not perceived by the general population [22]. In a previous study, general dentists and lay people were unable to detect even a 4 mm midline deviation [23]. For this reason, clinical evaluation of facial aesthetics may not coincide with the perceptions and expectations of patients or common people [24,25]. The fact that MMDs can be a part of the normal dental development makes it difficult for practitioners to decide whether to intervene or not at an early stage [7]. Therefore, the parental concerns and confusions regarding MMDs in their children would be unsurprisingly even higher. An effective MMDs treatment requires the accurate diagnosis and an intervention that is pertinent to that specific aetiology, including family screening, medical and dental histories, radiographic and clinical examinations, and possibly tooth-size and arch length evaluations [1,9]. Timing of the treatment is imperative to attain satisfactory results. Most of the researchers do not recommend tooth movement until the eruption of the permanent canines [26,27]. But in certain cases, where very large MMDs of >4 mm exist, treatment can be started early [28]. In the dental literature, there are no studies that have evaluated the perception and understanding of mothers regarding the various types of MMDs in children. Mothers spend most of their time upbringing their children [29,30] and they apparently are keen observers when it comes to the slightest change in appearances of their growing children [31,32]. Hence, the present study investigated the aesthetic perceptions of Saudi mothers to various MMDs in children.
Materials and Methods
This cross-sectional study involved randomly selected Saudi mothers of children attending elementary schools in Riyadh, Saudi Arabia over a period of eight months (November 2016 to June 2017). The study protocol and consent form were approved by the Research and Ethical Committee of Human Studies at the College of Dentistry Research Center (FR 0400) of King Saud University, Saudi Arabia.
The questionnaire was prepared by two senior orthodontic specialists with 15 years of professional experience. The study instrument was pretested through a pilot study conducted among 10 Saudi Mothers for reliability and content validity (α=0.90). The questionnaire consisted of four questions about demographic details one question on source of information about MMD and seven questions to assess the perception of mothers seeing the images. The participants were given 20 minutes to fill out the questionnaire. The questionnaire was distributed to the participated mother at the elementary schools and then were collected when completed within 20 minutes by two dental interns.
The sampling frame included Saudi mothers of children attending elementary schools in Riyadh, Saudi Arabia. Assuming a statistical power 90%, with 5% confidence interval and at 95% confidence level, the sample size was estimated to be 300 (EPI-INFO STAT CALC, CDC, Atlanta, USA). After 25% overestimation, a sample of 348 Saudi mothers was approached for the self-administered survey based research. A stratified cluster random sampling was used to select the required sample. The participant sample (mothers) were selected from a cluster of selected elementary schools under Saudi ministry of education. Mothers who agreed to participate were enrolled. Letters explaining the nature of the study and informed consent forms were sent to the interested participants.
The assessment tool in the form of a questionnaire was distributed to the participating mothers at the selected elementary school of Saudi Ministry of Education in Riyadh. Mothers who agreed to participate in the study received a self-administered questionnaire in the local language (Arabic).
An original photograph of a nine-year-old child with a smile assuring absence of MMD was obtained with the patient’s consent from the Paediatric Department of College of Dentistry, KSU [Table/Fig-1].
Normal smile line showing absence of Midline Diastema.

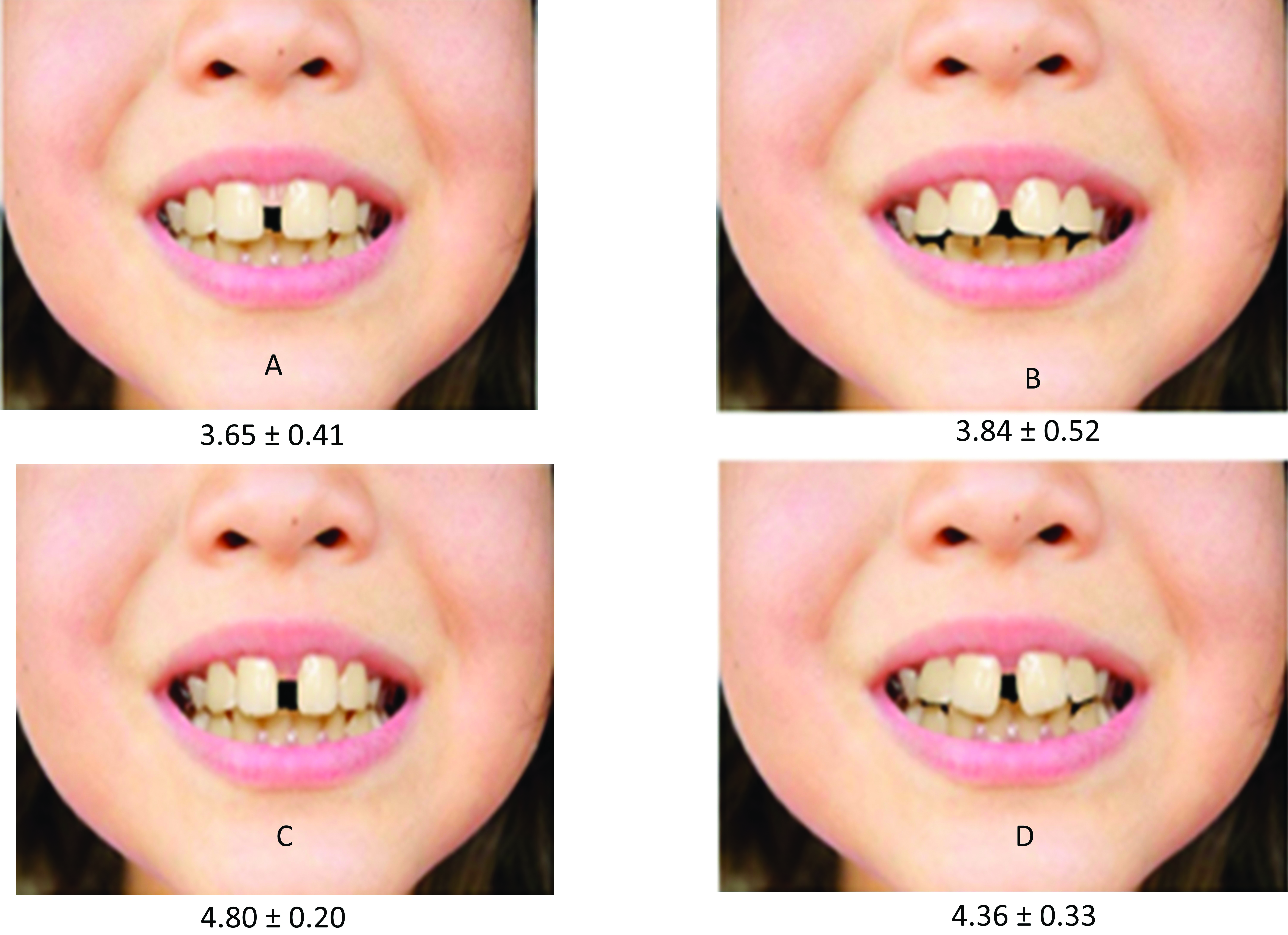
The photo was analysed and altered according to the study objectives utilising Adobe Photoshop software 7.0.1 ME software (Adobe Systems. San Jose, CA, USA). Four other photographs were generated by altering the original photograph using the same software. A midline diastema was created between the maxillary central incisors and progressively increased in 1 mm increments in accordance to previous study [23], as measured from the interproximal contact point between the central incisor crowns showing four types of MMDs which were due to: High Frenum Attachment (A), Thumb Sucking Habit (B), Central Incisor Tooth Discrepancy (C) and Ugly Duckling Stage (D) as shown in [Table/Fig-2]. These alterations were chosen based on their frequency and clinical significance to the smile [21]. A midline diastema was created incrementally between the maxillary central incisors. It was widened progressively in 0.5 mm increments. The measurements were made at the interproximal contact points between the central incisor crowns. Along with the questionnaire, the photographs of various MMDs were presented in a sheet of paper and the participants were asked to give a score 1 to 5 (very pleasant=1, pleasant=2, neutral=3, unpleasant=4, and very unpleasant=5) [33] to each MMD photograph (A-D).
Photographs showing alteration of a midline diastema. A: High Frenum Attachment (1 mm), B: Thumb Sucking Habit (2 mm), C: Central Incisor Tooth Discrepancy (3 mm), and D: Ugly Duckling Stage (4 mm).
Statistical Analysis
Data were manually entered, and statistical analysis was performed using Statistical Package for the Social Sciences software package (IBM, SPSS version 20, Chicago, IL, USA). The Chi-square test was used to identify differences in responses for different variable, with the level of significance level set at p-value <0.05.
Results
From the 348 mothers who were contacted, 300 agreed to participate in the study and submitted a completed questionnaire, with a response rate of 86.2%. The age of the mothers ranged between 23-48 years with a mean (±SD) age of 37.6±8.3 years. The socio-demographic characteristics are shown in [Table/Fig-3].
Socio-demographic characteristics of participants.
| Question No. | Variables | Total N=300 n (%) |
|---|
| 1 | Age (years) | <25 | 14 (4.7) |
| 25-35 | 91 (30.3) |
| >35-45 | 145 (48.3) |
| >45 | 50 (16.7) |
| 2 | Level of education | High school | 74 (24.7) |
| College | 192 (64.0) |
| Higher education | 34 (11.3) |
| 3 | Occupation | Unemployed | 98 (32.6) |
| Government job | 120 (40.0) |
| Private job | 82 (27.4) |
| 4 | Monthly Income (Saudi Riyal) | ≤5,000 | 54 (18.0) |
| >5,000-20,000 | 208 (69.3) |
| >20,000 | 38 (12.7) |
The majority of the mothers (192) were educated up to the college level (64%) and 120 were doing a government job (40%).
The mean scores and the responses to the 5-point Likert scale [15] in percentages were found to be statistically significant as shown in [Table/Fig-4,5].
Overall mean score and Standard Deviation (SD) of the “Most unpleasant” evaluated MMDs photographs by participants.
| S. No. | MMDs photograph | Mean score±SD | p-value |
|---|
| 1 | A | 3.65±0.41 | 0.012* |
| 2 | B | 3.84±0.52 |
| 3 | C | 4.80±0.20 |
| 4 | D | 4.36±0.33 |
*Significant differences resulting from Chi-square test.
MMDs: Maxillary midline diastemas. A: High frenum attachment, B: Thumb sucking habit, C: Central incisor tooth discrepancy, D: Ugly duckling stage
Participants’ responses to each of MMDs photos.
| S. No. | MMDs photo | Very pleasant % | Pleasant % | Neutral % | Unpleasant % | Very unpleasant % | p-value |
|---|
| 1 | A | 0 | 2 | 40 | 51 | 7 | 0.001* |
| 2 | B | 0 | 1 | 18 | 48 | 33 | 0.001* |
| 3 | C | 0 | 0 | 3 | 16 | 81 | 0.001* |
| 4 | D | 0 | 0 | 8 | 37 | 55 | 0.001* |
MMDs: Maxillary midline diastemas; A: High frenum attachment, B: Thumb sucking habit, C: Central incisor tooth discrepancy, D: Ugly duckling stage; *Significant differences resulting from Chi-square test.
The maximum mean score was 4.80±0.20 for the MMD photograph showing central incisor tooth discrepancy with around 243 mothers perceiving it to be the most unpleasant (81%). This was followed by the photograph showing ugly duckling stage and thumb sucking habit which was perceived to be most unpleasant by 165 (55%) and 99 (33%) mothers respectively. The MMD photograph showing high frenum attachment was perceived by 153 (51%) of the mothers to be unpleasant and 7% as very unpleasant. Moreover, it showed a relatively least mean score of 3.65±0.41.
When enquired about the source of information regarding MMDs, majority of the mothers (158) reported the source to be dentist (52.7%) followed by the internet or social media (25.3%) and friends (17%) as shown in [Table/Fig-6].
Source of information regarding MMDs.
| S. No. | Source of information | Total N=300N (%) | p-value |
|---|
| 1 | Dentist | 158 (52.7) | 0.001* |
| 2 | Friends | 51 (17.0) |
| 3 | Internet/social network | 76 (25.3) |
| 4 | Others | 15 (5.0) |
*Significant differences resulting from Chi-square test
Almost three-quarters, 222 of the participants (74.7%) did not know if the gap between the cut outs in it will close automatically with time. However, more than (169) half of the participants (56.33%) thought that the gap between the incisors shown in the pictures needs treatment. Nearly, two-thirds (183) of the participants (61.0%) preferred getting a treatment to close the gap between the incisors if exists with their son or daughter, as shown in [Table/Fig-7].
Participants’ responses to MMDs photos.
| S. No. | Variables | Total N=300 n (%) | p-value |
|---|
| 1 | From your point of view, in which image do you think the gap in the cutouts will close automatically with time? | A | 32 (10.7) | 0.001* |
| B | 21 (7.0) |
| C | 8 (2.6) |
| D | 15 (5.0) |
| I don’t know | 224 (74.7) |
| 2 | From your point of view, do you think that the gap between the incisors present in the pictures needs treatment? | Yes | 169 (56.33) | 0.001* |
| No | 83 (27.66) |
| I don’t know | 48 (16.0) |
| 3 | If this gap between the incisors exists with your son/daughter, would you prefer getting a treatment to close it? | Yes | 183 (61.0) | 0.001* |
| No | 87 (29.0) |
| I don’t know | 30 (10.0) |
*Significant differences resulting from Chi-square test
Discussion
This cross-sectional study was conducted to investigate the aesthetic perception of Saudi mothers regarding the various types of MMDs in children. The prevalence rates of MMD in the Saudi population between the ages 13 and 40 years were previously reported to be 23% with width ranging between 0.5-4 mm [34] and 22% among 12 to 16 year group children [35]. MMD in the Saudi population is considered an aesthetic issue and perceived to be aesthetically disturbing especially when MMD persists beyond the eruption of all permanent teeth [34].
In this study, the majority of the mothers surveyed were between 35 and 45 years of age (48.3%), had a college education (64%) and were employed in the government service (40%). The present study revealed that the mothers perceived all types of MMDs to be unpleasant and this clearly implies that certain steps need to be taken by dental professionals to raise the awareness of MMDs in children to parents and caregivers [36].
In general, physiological midline diastema occurring during mixed dentition called ugly duckling stage is found in 98% of children at the age of 6 years [7]. Spontaneous closure of such diastemas of 2 mm or less is evidenced in majority of the children. However, in diastemas measuring more than 2 mm, surgical intervention of high frenal attachment is often advocated [7]. MMDs developed due to central incisor tooth discrepancy are often corrected orthodontically and further aesthetically restored with composite or crown. Thumb sucking habit leads to formation of MMDs of more than 2 mm wherein habit breaking appliances becomes indispensable [37].
In the present study, MMD showing central incisor tooth discrepancy was perceived by the mothers’ to be the most unpleasant (81%) with the maximum mean score of 4.80 (0.20). However, MMDs are considered to be a sign of beauty in the country of Nigeria [28]. Negative aesthetic alterations in anterior teeth are easily visible when compared to the posterior teeth and this has a huge impact on the observer and can lead to dissatisfaction with oral aesthetics [38]. The study conducted among Saudi dentists and lay people regarding altered smile aesthetics in adults revealed that even a small amount of space between the maxillary central incisors was rated as unattractive [36]. Likewise, it has been reported that asymmetric alterations make teeth appear unattractive to both dental professionals and lay people [21].
In par, a similar research reported that study participants rated MMDs of 2 mm as attractive [28]. In addition, a study comparing prevalence and perception of MMDs among African and Caucasian population exclaimed that MMD of more than 4 mm was only considered as unpleasant [28].
Opinions and responses of lay people are useful in routine practice to prioritise problems and to identify preferences in health care services [33]. The fact that cultural and ethnic characteristics, treatment expectations, and access to dental services may have impacted the responses provided by the mothers cannot be denied [30,31]. It has been reported that younger children are unaware of their dental appearance and their perception of dental attractiveness increases with age [39]. Although, it is imperative to involve parents in the decision-making process on whether or not the child should undergo treatment, overemphasising parent’s opinion should be dealt with caution as they may tend to amplify the impact of dental appearance on the child [40]. This outlines the need to provide appropriate advice and guidance to parents, along with their children when discussing the importance of finding the cause of MMD and the provision of dental services [12].
Two critical information needs to be put across to the public regarding MMDs. Firstly, spontaneous correction of a childhood MMD is most likely when its width is not more than 2 mm and the period of waiting till the eruption of the permanent canines [9]. Secondly, the importance of a thorough dental check up to rule out pathological causes like supernumerary teeth and midline soft tissue anomalies (high frenum attachment), which can be surgically removed, followed by orthodontic space closure [34]. In addition, it is better to align the teeth before frenectomy. Oral habits such as thumb sucking and tongue thrusting should be corrected before closure of the space [41]. The results of this study may help in making strategic plans to enhance the awareness of mothers about MMDs in children and its repercussions. For instance, oral education strategies in the form of distribution of flyers/posters emphasising the two above-mentioned key information to parents in general, with algorithm for decision making process may be initiated during regular check-ups for children [42].
Limitation(s)
Certain limitations of this study merits mention in order to improve on future studies. Firstly, being a questionnaire-based survey, there may be some elements of under-reporting bias and non-respondent bias in the study. Another limitation of this study is the homogenised sample. The inclusion of only mothers has limited the extrapolation of results to the general population. However, future studies considering different populations with varying ethnic and cultural characteristics should be conducted to confirm the findings presented herein.
Conclusion(s)
Based on the present study findings, Saudi mothers perceived MMDs with spacing between the central incisors to be most aesthetically unpleasant thus requiring management followed by MMDs developed during ugly duckling stage and those due to thumb sucking habit. MMDs due to high frenal attachment when found as unpleasant as suggested by the current study warrant early intervention.
Declaration: This research project was supported by a grant from the “Research Center of the Center for Female Scientific and Medical Colleges”, Deanship of Scientific Research, King Saud University.
*Significant differences resulting from Chi-square test.
MMDs: Maxillary midline diastemas. A: High frenum attachment, B: Thumb sucking habit, C: Central incisor tooth discrepancy, D: Ugly duckling stage
MMDs: Maxillary midline diastemas; A: High frenum attachment, B: Thumb sucking habit, C: Central incisor tooth discrepancy, D: Ugly duckling stage; *Significant differences resulting from Chi-square test.
*Significant differences resulting from Chi-square test
*Significant differences resulting from Chi-square test