Rubella virus causes an acute and contagious childhood disease known as rubella, little red, 3-day measles, or German measles [1,2]. The disease is characterised by maculopapular rash associated with a low-grade fever, lymphadenopathy, and malaise [3]. It can also cause joint pains, headache, and conjunctivitis in adults [4]. Rubella infection is considered relatively benign, and the infection is usually mild and self-limited in the absence of pregnancy. Rubella represents a major health concern globally due to its devastating effect on the developing foetus during pregnancy [5]. Almost six decades ago, the teratogenic potential of rubella virus was well established by an Australian ophthalmologist, Norman Gregg, that if a pregnant mother is infected within first five months, she might have Bad obstetric history or baby born with CRS [5].
The clinical spectrums of CRS are eye anomalies (cataracts, pigmentary retinopathy, microphthalmia, and glaucoma), sensorineural hearing loss, and cardiac defects (most commonly patent ductus arteriosus and pulmonary stenosis) [6]. Other manifestations include intrauterine growth retardation, “blueberry muffin” spots, pneumonitis, bone defects, hepatosplenomegaly, developmental delay, encephalitis, autism, diabetes mellitus, and thyroid dysfunction [6]. According to the World Health Organisation (WHO), still over 100,000 babies are born worldwide with CRS every year despite of safe and inexpensive vaccines [7]. India has the largest burden, with an estimated 40,000 cases [8-10]. WHO, South-East Asia Region, has set a target to eliminate rubella and CRS till 2023 [11]. Maintaining high population immunity to rubella, creating a network of laboratories, and developing and sustaining a case-based surveillance system are the principal strategies for elimination of measles and control of rubella and CRS [12]. India in February 2017 has introduced the rubella-containing vaccine under the Universal Immunisation Program, along with the measles vaccine [13].
Recently a health ministry surveillance program found that in India 33.3% babies screened in the last six months had CRS and birth defects [14]. Even though in 2017 the Government of India has included a rubella virus dose with measles vaccine, still much of the area is undercover and needs validated research [14]. Women living in the rural area tend to be more susceptible to infections. Various factors might be attributed to low immunity status in them like, living in a crowded community, poor hygiene practices, low educational background, lack of awareness for rubella, importance of complete coverage of immunisation and knowledge of CRS is deficient [10].
Keeping in view the above backdrop that the regional surveillance data is essential to curb the morbidity, the present study was intended to estimate the percentage of pregnant women in the vicinity of Piparia village susceptible to rubella virus infection and also to correlate it with various risk factors pertaining to sociodemographic and reproductive history.
Materials and Methods
This prospective cross-sectional study was conducted on 90 pregnant woman attending the Obstetrics and Gynaecology Out Patient Department (OPD) of Dhiraj Hospital, Piparia, Vadodara, Gujarat, India for the period of four months from September 2019-December 2019. The study was commenced after the approval from Sumandeep Vidyapeeth Institutional Ethical Committee (Approval number: SVIEC/ON/medi/SRP/19048).
Sample size calculation:
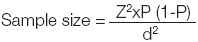
Z=1.96, P=expected proportion of low immunity for rubella in population based on previous studies-10%, d=absolute error of precision-5%, Owing to short duration of study (four months) and Kit Constrained a limited sample of 90 were considered.
Inclusion and Exclusion criteria: Pregnant women in her First/Second Trimester belonging to the rural Piparia region and of the age group 18-45 years were included in the study, while those women already vaccinated for Measles-Mumps-and Rubella (MMR) and those not willing to participate were excluded from the study.
Methodology: Informed consent was obtained from each patient and information like age, educational status, occupation, history of rubella vaccination, trimester, gravidity (primigravida/multigravida), history of still birth (foetal death at or after 20 or 28 weeks of pregnancy- CDC) twice before the live birth [15], parity, any symptoms like mild fever/rash/sore throat/headache/arthritis/jaundice etc., were noted in a pre-formed questionnaire.
Blood Collection and Handling: Five mL of venous blood was collected aseptically from each pregnant woman for the determination of rubella antibodies. Blood was allowed to clot for an hour at room temperature, centrifuged at 3500 rpm for five minutes, and then serum was separated and stored in sterile vials at -20°C until laboratory analysis.
Microbiological Investigation: Serological evaluation for rubella IgG antibodies was performed in the Microbiology laboratory of Dhiraj Hospital. E-RVG-K14 Rubella IgG ELISA kits were procured from Nucleus Inc., RD Ratio diagnostics, Frankfurt, Germany. The procedure was performed according to the instruction given in the flyer. As per the product manual (E-RVG-K14 Rubella IgG ELISA), the results were interpreted positive for anti-rubella virus IgG if the titer was >11 IU/mL, negative if the concentration was <9 IU/mL and equivocal if the concentration ranged between 9 and 11 IU/mL.
Statistical Analysis
A Pearson Chi-square test was used to find out the significant correlations. The p-value <0.05 will be considered significant. Data analysis were conducted using SPSS version 15.0.
Results
Socio-demographic characteristics of the pregnant women [Table/Fig-1]: A total of 90 pregnant women attending the antenatal centre of Dhiraj Hospital were incorporated in the study. The mean age of the participants was 23.26±5 years (range 18-45 years). Half of the study participants were in the age group of 20-24 years (n=45, 50%), 60 females out of 90 (66.7%) were from lower middle socio-economic group. Forty-six (51.1%) of the study participants had done primary education, majority of them were house wives (92.2%), 73.3% women were in second trimester, 57.8% women had multigravida, majority (94.4%) were not aware about Rubella vaccination. Four women (4.5%) had a history of still birth. None of the women had any symptoms like fever, maculopapular rash, running nose, sore throat, malaise, arthritis, arthralgia or jaundice.
Socio-demographic characteristic of rural pregnant women enrolled in the study (n=90).
| Variables | Sub-variables | No. (%) |
|---|
| Age group (years) | 15-19 | 12 (13.3%) |
| 20-24 | 45 (50%) |
| 25-29 | 26 (28.9%) |
| 30-35 | 07 (7.8%) |
| Socioeconomic status | Lower | 23 (25.5%) |
| Lower middle | 60 (66.7%) |
| Lower upper | 07 (7.8%) |
| Educational status | No formal education | 14 (15.6%) |
| Primary | 46 (51.1%) |
| Secondary | 30 (33.3%) |
| Occupation | House wife | 83 (92.2%) |
| Daily laborer | 07 (7.8%) |
| Trimester | First | 24 (26.7%) |
| Second | 66 (73.3%) |
| Gravidity | Primigravida | 38 (42.2%) |
| Multigravida | 52 (57.8%) |
| Parity | Null | 37 (41.1%) |
| Multi | 53 (58.9%) |
| History of still birth | Yes | 04 (4.5%) |
| No | 86 (95.5%) |
Prevalence of rubella immunity (i.e., the presence of IgG antibodies) and its association with various characteristics [Table/Fig-2]: Out of 90 serum samples tested, 80 were positive, this shows that the overall seroprevalence of rubella immunity in pregnant women was 88.9%; while 11.1% women had revealed low immunity for rubella.
Association of heterogeneous risk factors with rubella immunity.
| Variables | No. of antenatal women enrolled | Anti-Rubella IgG positive women (n=80, 88.9%) | Anti-Rubella IgG negative women (n=10, 11.1%) | p-value |
|---|
| Age group (years) | 15-19 | 12 | 11 (91.6) | 01 (8.4%) | 0.766 |
| 20-24 | 45 | 38 (84.4) | 07 (15.6%) |
| 25-29 | 26 | 24 (92.3) | 02 (7.7%) |
| 30-35 | 7 | 7 (100) | - |
| Socio-economic status | Lower | 23 | 22 (95.7%) | 01 (4.3%) | 0.411 |
| Lower middle | 60 | 51 (85%) | 09 (15%) |
| Lower upper | 07 | 07 (100%) | - |
| Educational status | No formal education | 14 | 10 (71.45) | 4 (28.55%) | 0.006 |
| Primary | 46 | 42 (91.3) | 4 (8.7%) |
| Secondary | 30 | 28 (93.3%) | 2 (6.7) |
| Occupation | House wife | 83 | 74 (89.1%) | 09 (10.9%) | 0.780 |
| Daily wager | 07 | 06 (85.8%) | 01 (14.2%) |
| History of Rubella vaccination | Yes | 01 | 01 (100%) | 00 | 0.722 |
| No | 89 | 79 (88.9%) | 10 (11.1%) |
| Trimester | First | 24 | 20 (83.3%) | 04 (16.7%) | 0.311 |
| Second | 66 | 60 (90.9%) | 06 (9.1%) |
| Gravidity | Primigravida | 38 | 33 (86.8%) | 05 (13.1%) | 0.597 |
| Multigravida | 52 | 47 (90.3%) | 05 (9.6%) |
| Parity | Null | 37 | 32 (86.4%) | 05 (13.5%) | 0.544 |
| Multi | 53 | 48 (90.5%) | 05 (9.4%) |
| History of still birth | Yes | 04 | -- | 04 (100%) | 0.057 |
| No | 86 | 80 | 06 |
p-value less than 0.05 considered significant
Immunity was notably higher (100%) in women of 30-35 years of age, followed by 25-29 years (92.3%) of age. Nevertheless, there was no statistically significant difference (p-value-0.766). According to their socioeconomic status, higher immunity was found in the lower upper class women and was strangely found least in the women belonged to lower-middle class.
In the lower middle group of women with low immunity, 50% women were multigravida and they all had a history of still birth twice before the live birth.
Level of education also significantly correlated to the immune status of pregnant women as 93.3% of those women with higher education were immune to rubella compared to the ones with no formal education (p-value=0.006). None of the women were aware about past history of rubella vaccination status.
The level of Rubella immunity was higher in the women in second trimester (90.9%) in comparison to the women in first trimester (83.3%, p-value-0.311). Among the multigravida, higher prevalence of 90.3% was obtained, while in primigravida, prevalence was 86.8%.
Characteristics of the women with low immunity for Rubella (N=10): Ninety percent (90%, 9/10) of those women with low immunity belonged to lower middle group and 70% (7/10) of them were of the age group 20-24 years and they all were uneducated and unaware about the consequences of disease and importance of vaccination. Around 90% (9/10) women with low immunity were housewife, 60% (6/10) were in the second trimester and all of them had a history of still birth (p-value-0.05) (other reasons of still birth like any birth defects, pre-eclampsia, congenital infections, diabetes, obesity, thyroid etc., were excluded).
Discussion
In the past, prior to the introduction of immunisation program, the endemicity of rubella in India was well documented [16,17]. After the implementation of vaccination, the disease shifted from children to young adults [16,17]. However, a substantial number of women of childbearing age (10-28%) were apparently showing low immunity (by natural infection or immunisation), and thus were at a risk of acquiring infection during the pregnancy which can infect the foetus leading to a CRS [17]. Seroprevalence survey of rubella immunity in pregnant women plays a pivotal role not only in defining the disease epidemiology but also can obliquely clue at the risk of acquiring CRS [18]. In the present study, conducted among pregnant women, 88.9% had a protective level of IgG antibodies while the rest 11.1% were susceptible and can acquire infection during pregnancy. Higher levels of protective immunity suggest that they have acquired natural infection during their life prior to pregnancy, as none of them had received vaccination against rubella.
The rural populations are always inclined to live in a closed community with overcrowding, and owing to the asymptomatic nature of rubella which might be the key factors contributing to high seroprevalence in this study [19].
There is considerable variation in the prevalence of rubella IgG among women of child bearing age in different geographical regions [Table/Fig-3] [10,12,17,20-25]. In this study, age-wise seropositivity to rubella was found to increase with increasing age; it was 100% in women of 30-35 years of age, followed by 92.3% in 25-29-year-old and 84.4% in 20-24 years. of age. These results were well corroborated with the study done in Nigeria [19] and Trichy [10]. As a matter of fact, with increasing age and parity a woman’s risk of acquiring the infection should expectedly augments due to the more recurrent exposure of the younger age to rubella virus, which activate the development of immunity to the virus [25]. Although women of both the rural and urban community are exposed to rubella at younger age but in rural community, chances of exposure are less as they live in area with low population density [20], that might be the reason of developing low immunity.
Data of Rubella immunity status in the pregnant women from different geographical regions [10,12,17,20-25].
| S. No. | Author (Year of publication) | Place | Setting | Participants | Rubella immunity |
|---|
| 1. | Singla N et al., [20] (2004) | Amritsar | Hospital based and health personal based | 233 | 67.2% |
| 2. | Padmaja M et al., [24] (2010) | Kerala | Hospital based setting | 485 | 65.7% |
| 3. | Gupta A et al., [12] (2015) | Lucknow | Hospital based setting | 152 | 88.2% |
| 4. | Kolawole OM and Anjorin EO [25] (2014) | Nigeria | Hospital based setting | 200 | 87.5% |
| 5. | Priyanka D et al., [10] (2016) | Tamil Nadu | Hospital based setting | 100 | 90% |
| 6. | Thayyil J et al., [17] (2016) | Kozhikode | Community based | 70 | 90% |
| 7. | Tamirat B et al., [21] (2017) | South Ethiopia | Hospital based setting | 422 | 86.3% |
| 8. | Wondimeneh Y et al., [22] (2018) | Ethiopia | Hospital based setting | 600 | 89% |
| 9. | Present study (2021) | Gujarat | Hospital based setting | 90 | 88.9% |
Higher level of immunity (93.3%) was found in the women with education till secondary high school compare to the women with no formal education (p-value-0.006). These results were consistent with the studies done by Priyanka D et al., and Tamirat B et al., [10,21]. This clearly proves that education has always been acknowledged as an additional advantage in various facets of life and also helps in making informed decision and sourcing for useful information regarding health concerns and also reflects their improved level of hygiene.
Prevalence based on gestational age showed, 90.9% in second trimester and 83.3% in first trimester were immune to rubella and hence their babies were not at risk of developing CRS [24].
The seroprevalence of rubella immunity in multigravida was higher than that acquired in primigravida, which was in consistence with the findings that with each pregnancy outcome, there is an increase in the number of rubella immune women [26]. The lower prevalence obtained in primigravid makes them more susceptible to rubella and this suggests that their babies are at risk of CRS, thus agrees with the earlier study that the incidence of congenital rubella is higher in first born babies [27].
Low level of immunity was found in 100% women with bad obstetric history, which shows statistical significance, indicating that rubella infection might be the cause of still birth (p-value-0.05) in all of them. It was rightly quoted by The Director General of the Indian Council of Medical Research (ICMR) [14], that still much awareness is needed regarding rubella and specified that it is high time India should focus on the syndrome.
Limitation(s)
Sample size was small to comment on the actual level of immunity in pregnant women.
Study period was of four months, so follow-up of patients could not be done with low immunity.
Due to time constraint, screening of rubella immunity could not done in women of child bearing age and adolescent girls. As rubella is a vaccine preventable disease, so vaccine can be given to those with low immunity.
Conclusion(s)
The present study showed that a significant proportion of pregnant females are still susceptible to rubella virus infection in India, so antenatal screening for rubella should be mandatory. Adhering to the stringent protocol of rubella vaccination in adolescent girls and women of child bearing age with sero-surviellance can reduce the risk of CRS in India especially in rural places.
p-value less than 0.05 considered significant