Sexually Transmitted Infections (STIs) are a heterogenous group of infections which are often transmitted sexually [1]. Various risk factors predispose to STI such as unprotected sexual contact with an infected partner or Commercial Sex Workers (CSWs), multiple sexual partners, homosexuality and anal intercourse [1,2]. STIs pose a major health, social and economic problem worldwide, predominantly in developing countries like India. Over the past few decades, a number of advanced techniques including serological and molecular diagnostic tests have been introduced to improve the diagnosis of STIs. But due to unavailability of uniform resources in majority of healthcare centres throughout the country and delay in results, the diagnosis and treatment of patients is still dependent on syndromic approach guidelines devised by National AIDS Control Organisation (NACO) [3,4]. The knowledge of epidemiology and pattern of STIs and associated high risk behaviour among population is essential for the designing, implementing, and monitoring successful targeted interventions for prevention and treatment of these infections. Although in last few decades, many studies have been conducted in different parts of India, there is paucity of information from central India.
The primary aim was to study the pattern and proportion of STIs among the patients attending STI clinic at a tertiary care hospital in central India. The authors also aimed to study the prevalence of HIV and demographic pattern such as distribution as per age, sex, residence, education and marital status and sexual behaviour pattern among the patients attending STI clinic. The knowledge of demographic pattern, proportion of STIs and associated risk factors and their regular surveillance is essential for the designing, implementing, and monitoring successful targeted interventions for prevention and treatment of STIs.
Materials and Methods
This was a cross-sectional study of data obtained retrospectively from STI clinic at a tertiary care hospital in Nagpur, referred by the outpatient Department of Dermatology and Gynaecology from January 2013 to December 2019. Approval from Institutional Ethics Committee was sought (ECR/485/Inst/MH/2013/RR-20) and case records from STI clinic were analysed retrospectively in January-June 2020. A total of 4471 cases of STI were seen during the study period of 7 years. Details of cases were recorded and included age, gender, residence, educational status, occupation, per capita income (modified BG Prasad’s socio-economic classification) [5], marital status, sexual orientation, number of partners, use of barrier contraceptive, onset and progression of symptoms, prior treatment, and history of similar complaints in partners. A thorough clinical examination of genital, anal and oral mucosa and associated lymph nodes was performed. Investigations requiring staining and microscopy such as gram-stain, KOH mount, tzanck smear and wet mount were done wherever required as per clinical presentation. Blood investigations including Venereal Disease Research Laboratory (VDRL) test and Treponema Pallidum Hemagglutination Assay (TPHA) for syphilis and antibody for HIV (ELISA and immunochromatographic rapid detection tests) were performed after pre-test counselling. The patients found positive for HIV were offered post-test counselling by an STI counselor and referred to Anti-Retroviral Therapy (ART) center of the hospital. Partner notification, examination and counseling were also done. Education regarding safe sexual practices and condom promotion were done.
Inclusion criteria: The patients were categorised as per the NACO guidelines [4] into urethral discharge, Cervico-vaginal Discharge (CVD), Genital Ulcerative Disease-Nonherpetic (GUD-NH), Genital Ulcerative Disease-Herpetic (GUD-H), lower abdominal pain (Pelvic inflammatory Disease-PID), and inguinal bubo. Along with these syndromes, other STIs that are not included in the syndromic management such as balanoposthitis, anogenital warts (condyloma acuminata) and genital molluscum contagiosum were included in the study, diagnosed on the basis of history of sexual exposure, clinical examination with help of biopsy, KOH mount, gram stain and microscopy wherever necessary.
Exclusion criteria: Cases of genital scabies were excluded from the study considering that it can spread even without sexual contact. Also, cases of HIV without any STI were not included. All the cases included in the study were sexually active as per history.
Statistical Analysis
The data was analysed statistically to study the clinico-epidemiological profile by using MS Excel and Epi Info software, and percentage, mean, standard deviation and proportions were calculated.
Results
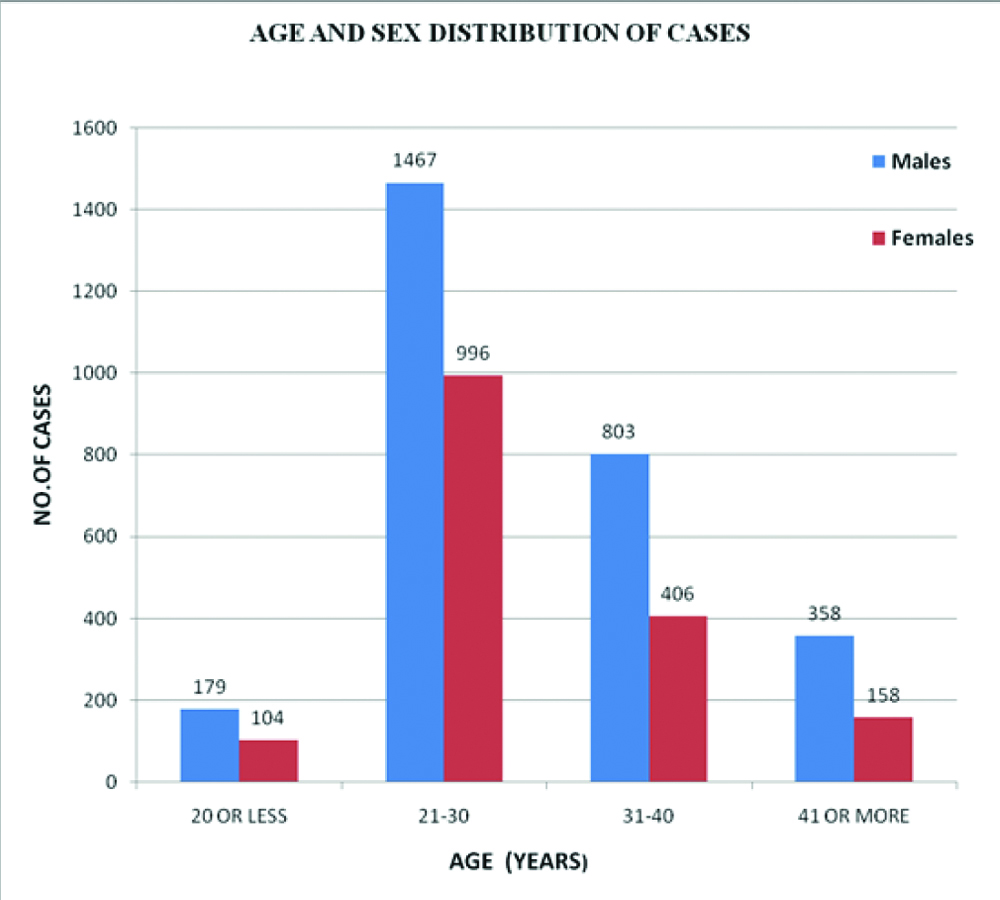
Out of the total 4471 cases, 2807 (62.8%) were males and 1664 (37.2%) were females and male-to-female ratio was 1.7:1 [Table/Fig-1]. Majority of the patients were in the early reproductive age group of 21-30 years (2463 cases, 52.3%), followed by 31-40 years (1209 cases, 28.6%), 41 years of age or more (516 cases, 12.7%), age of 20 years or less (283 cases, 6.4%). The average age of sample population was 29.6 (±7.4) years (range 15-73 years). The average age was 30 years (±7.5) in males and 29 years (±7.0) in females [Table/Fig-2]. The majority of the patients were married (3203 cases, 71.6%) and heterosexual (4361 cases, 97.5%). A total of 103 (2.3%) and 7 (0.2%) patients had homosexual and bisexual orientation, respectively [Table/Fig-3]. A history of multiple sexual partners was obtained from 1014 males and among these 98 (9.7%) cases gave history of contact with CSWs. Out of these, only 388 (38.3%) cases gave history of regular use of barrier contraceptives and the remaining 626 (61.7%) cases practiced unprotected intercourse with multiple partners [Table/Fig-3]. Out of total sample population, 3568 (79.8%) cases were residing in urban areas and 4363 (97.6%) patients were literate [Table/Fig-2]. The patients were classified into five social classes as per Modified BG Prasad’s Socio-economic Classification and majority of patients were from social class II (1614 cases, 36.1%) and class III (1108 cases, 24.8%) [5]. Delay in visiting STI clinic and hence delay in diagnosis for a period more than six months was seen in 1027 (23%) cases. The reasons observed for delay were treatment from pharmacy or general practitioner, absence of symptoms, neglect of disease, social stigma regarding the infection and lack of awareness regarding STI clinic. History of prior treatment from general practitioner or pharmacy in the form of oral or topical treatment was reported in 1145 (25.6%) cases.
Distribution of cases according to age and sex.
Socio-demographic details of the sample population.
| Characteristics | Number of cases (%) |
|---|
| Total cases | 4471 |
| Males | 2807 (62.8%) |
| Females | 1664 (37.2%) |
| Average age (Years) | 29.63±7.4 |
| Males (Years) | 30.03±7.5 |
| Females (Years) | 28.96±7.0 |
| Residence |
| Urban | 3568 (79.8%) |
| Rural | 903 (20.2%) |
| Educational status |
| Illiterate | 108 (2.4%) |
| Up To Class 12 | 2357 (52.7%) |
| Graduation | 2006 (44.9%) |
| Social class (Modified BG Prasad’s Social Classification) |
| Class- I | 841 (18.8%) |
| Class- II | 1614 (36.1%) |
| Class- III | 1108 (24.8%) |
| Class- IV | 807 (18.0%) |
| Class- V | 101 (2.3%) |
Characteristics of sexual behaviour of the cases.
| Characteristics | Number of cases (Percentage) |
|---|
| Marital status |
| • Unmarried | 1236 (27.6%) |
| • Married | 3203 (71.6%) |
| • Widower/Divorced | 32 (0.7%) |
| Sexual orientation |
| • Heterosexual | 4361 (97.5%) |
| • Homosexual | 103 (2.3%) |
| • Bisexual | 7 (0.2%) |
| Nature of sexual contact |
| • Single partner | 3402/4471 (76.1%) |
| • Patients with multiple sexual partners | 1069/4471 (23.9%) |
| • Females with multiple partners | 55/1664 (3.3%) |
| • Males with multiple partners | 1014/2807 (36.1%) |
| ■ Regular use of barrier contraceptives ■ Unprotected intercourse ■ Contact with commercial sex workers | 388/1014 (38.3%)626/1014 (61.7%)98/1014 (9.7%) |
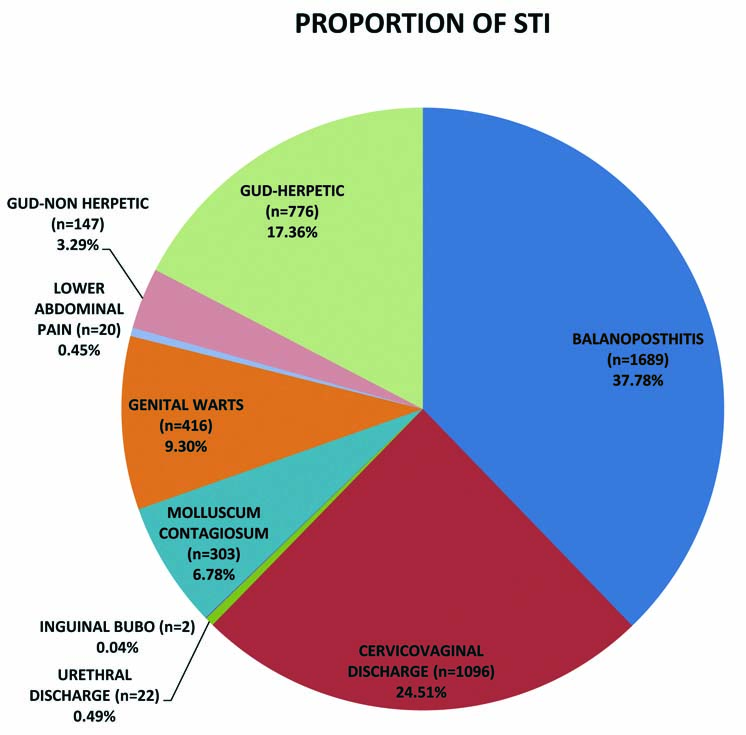
The most commonly observed STI was balanoposthitis (1689 cases, 37.8%), followed by cervico-vaginal discharge (1096 cases, 24.5%), GUD-herpetic (776 cases, 17.346%), anogenital warts (416 cases, 9.3%), molluscum contagiosum (303 cases, 6.78%), GUD-nonherpetic (147 cases, 3.28%), urethral discharge (22 cases, 0.5%), lower abdominal pain (20 cases, 0.45%) and inguinal bubo (2 cases, 0.04%). The proportion of viral STIs was 33.5% (1495 cases) including herpes genitalis, anogenital warts and genital molluscum contagiosum [Table/Fig-4].
Pie chart showing proportion of STIs in the study population categorised as per syndromic approach.
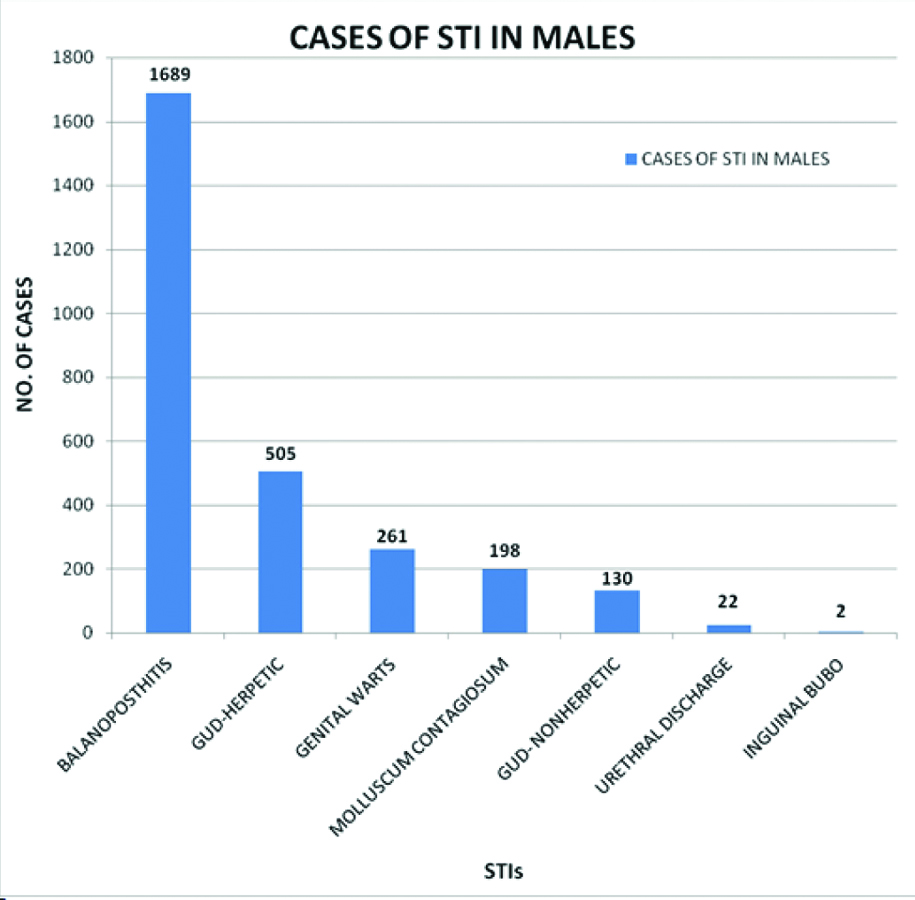
Among males, most commonly observed STI was balanoposthitis (1689 cases, 60.2%), followed by GUD-herpetic (505 cases, 18%), anogenital warts (261 cases, 9.3%), molluscum contagiosum (198 cases, 7.1%), GUD-nonherpetic (130 cases, 4.6%), urethral discharge (22 cases, 0.8%), and inguinal bubo (2 cases, 0.1%) [Table/Fig-5].
Bar diagram showing distribution of STIs among males.
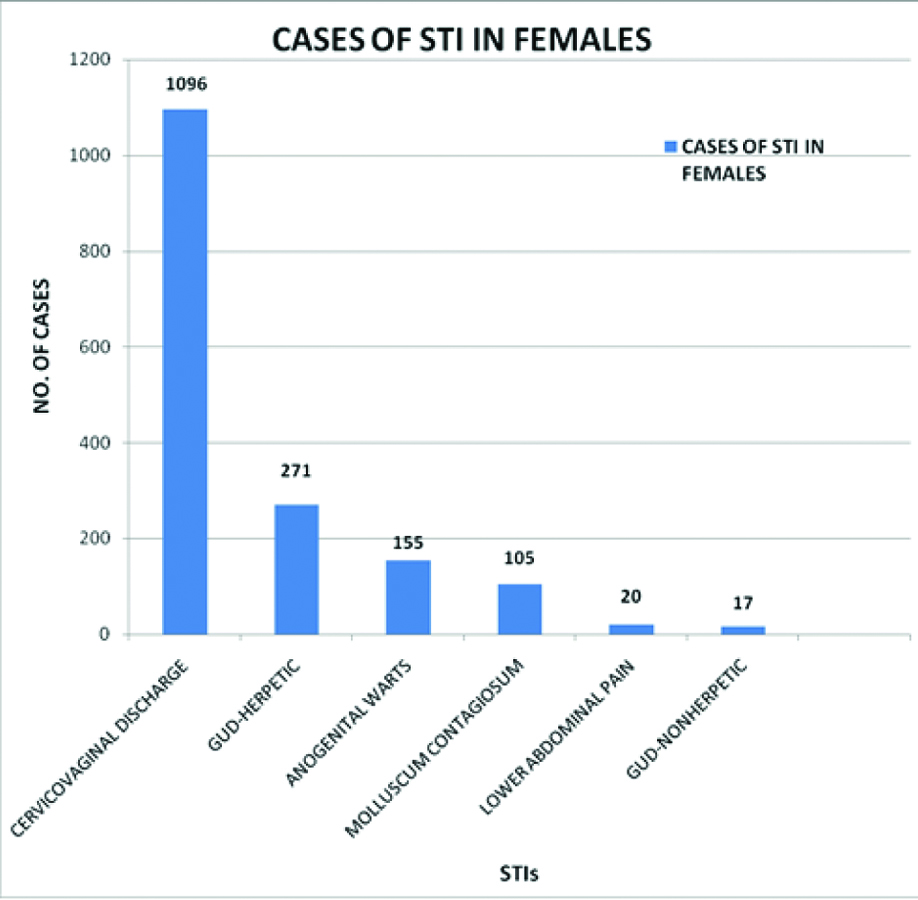
Among females, most commonly observed STI was cervico-vaginal discharge (1096 cases, 65.9%) followed by GUD-herpetic (271 cases, 16.3%), anogenital warts (155 cases, 9.3%), molluscum contagiosum (105 cases, 6.3%), lower abdominal pain (20 cases, 1.2%) and GUD-nonherpetic (17 cases, 1%) [Table/Fig-6].
Bar diagram showing distribution of STIs among females.
The number of newly diagnosed cases of HIV were 61 (1.4% of total cases), including 39 males (63.9%) and 22 females (36.1%). Among the STI clinic attendees, a total of 113 (2.5% of total) cases were patients living with HIV including 72 males (63.7%) and 41 females (36.3%). A total of 126 patients (2.8%) had significant VDRL titres (1:8 or more) along with positive TPHA, including 109 males (86.5%) and 17 females (13.5%) [Table/Fig-7].
VDRL and HIV reactivity among cases attending STI clinic.
| Test diagnosis | Total number of cases (Percentage) (N-4471) | Males (Percentage)(n-2807) | Females (Percentage) (n-1664) |
|---|
| VDRL positive | 126 (2.8%) | 109 (3.9%) | 17 (1.0%) |
| Newly diagnosed HIV cases | 61 (1.4%) | 39 (1.4%) | 22 (1.3%) |
| Patients living with HIV | 113 (2.5%) | 72 (2.6%) | 41 (2.5%) |
| Total prevalence of HIV | 174 (3.9%) | 111 (4.0%) | 63 (3.8%) |
HIV: Human immunodeficiency virus; VDRL: Venereal disease research laboratory
Discussion
STIs pose a major health, social and economic problem worldwide, predominantly in developing countries like India. As per the NACO annual report, an estimated 3 crore episodes of STI/reproductive tract infections occur every year in the country [3,6]. Cases of STI are often misdiagnosed due to lack of healthcare facilities and testing resources and often underreported due lack of awareness and social stigma. This emphasises on the need of constant surveillance regarding the prevalence and patterns of STI from all parts of the country. The study of demographic profile and current trends of different STI helps in planning and implementation of healthcare interventions towards control of HIV and STI.
In present study, the number of male patients is more than that of the females, a finding similar to other studies [7-9]. Study by Nyati A et al. showed female predominance because of higher referral from Gynaecology Department as well as cases of balanoposthitis in males were not included [3]. The majority of patients belonged to the age group of 21-30 years, in concordance with other studies [Table/Fig-8], as this is the most sexually active age group [3,7-9]. Homosexuality and bisexuality was observed in 103 cases (2.3%) and 7 (0.2%) cases respectively. A history of multiple sexual partners was obtained from 1014 males and among these 98 (9.7%) cases gave history of contact with CSWs and 626 (61.7%) cases practiced unprotected intercourse with multiple partners. History of contact with CSWs was elicited ranging from 4.6% to 23.5% cases in other studies [3,10]. Homosexual intercourse, multiple sexual partners, anal intercourse and unprotected sexual contact are high risk sexual behaviour and predisposes to acquiring and transmitting STIs and HIV.
Comparison of analysed data with other similar studies [3,7-10].
| Study | Present study | Sharma S et al., [8] | Nyati A et al., [3] | Sarkar S et al., [7] | Devi SA et al., [9] | Amin S et al., [10] |
|---|
| Place and Year of study | Nagpur (2013-19) | Jaipur (2012-14) | Kota (2012-16) | Kolkata (2011) | Puduchery (2004-06) | Aligarh (2008-13) |
| Age Range(Years) | 21-30 (52.3%) | 25-44 (57.5%) | 21-35 | 24-44(66.4%) | 21-30 (39.3%) | 16-25 (39.6%) |
| Sex | Males (62.8%) | Males (78%) | Females(62%) | Males (75.4%) | Males (66.7%) | Males (79.6%) |
| Most common STI-Overall | Balano-posthitis (37.8%) | Balano-postitis (39.6%), | Cervico-vaginal discharge (38%) | GUD-H (38.2%) | GUD-H (32.8%) | Genital scabies (53%) |
| Most common STI- Males | Balano-posthitis (60.2%) | Balano-posthitis (50.8%) | GUD-H (51.8%) | GUD-H (51.9%) | GUD-H | Genital scabies (51.8%) |
| Most common STI- Females | Cervico-vaginal discharge (65.9%) | Cervico-vaginal discharge (61%) | Cervico-vaginal discharge (61.3%) | Cervico-vaginal discharge (29.9%) | GUD-H | Genital scabies (57.9%) |
| VDRL/RPR positive | 2.8% | 2.9% | 0.6% | 1.07% | 11.6% | -- |
| Prevalence of HIV | 3.9% | 2.5% | 3.9% | 4.2% | 34.5% | 1.3% |
STI: Sexually transmitted infections; VDRL: Venereal disease research laboratory; RPR: Rapid plasma reagin; HIV: Human immunodeficiency virus; GUD-H: Genital ulcerative disease-herpetic
In present study, balanoposthitis followed by genital herpes and anogenital warts was the most common STI among males. In females, majority of reported cases had CVD followed by herpes genitalis and anogenital warts. Overall, the viral STIs (33.5%) such as GUD-H, anogenital warts and molluscum contagiosum were much more common than the bacterial STIs such as urethral discharge, syphilis, inguinal bubo and GUD-NH. There are many recent reports showing an emerging trend of viral STIs [11-17]. This change of actual decline of bacterial STIs and apparent increase of viral STIs in past few decades has been attributed to the widespread use of broad-spectrum antibiotics for other diseases resulting in partial or complete treatment of bacterial STI or alteration in the course of the disease and carrier state. The recent rise in cases of viral STIs has also been attributed to asymptomatic shedding of virus (herpesviral infection), lack of easily accessible and affordable diagnostic tests, and incurable nature of viral STIs [18].
VDRL reactivity was seen in 126 (2.8%) of the total cases which is significantly higher than previous studies by Nyati A et al., (0.9%) and Sarkar S et al., (1.07%) [3,7]. The overall prevalence of HIV in present study was found to be 3.9% including the new seropositive cases (1.4%) and person living with HIV (2.5%). This prevalence is slightly higher when compared to the data released by the NACO stating HIV prevalence is 2.46% in STI clinics [6]. Hospital-based studies conducted by Nyati A et al., and Vora et al., showed HIV prevalence of 3.6% and 4.2% respectively [3,11]. As STIs and HIV are co-factors in transmission of each other, it is necessary to study their relative prevalence and plan strategies for reduction in newly diagnosed cases of HIV.
Delay in diagnosis of more than six months was reported in 23% patients. The common reasons for this delay as per history were treatment from pharmacy or general practitioner, absence of symptoms, neglect of disease, social stigma regarding the infection and lack of awareness regarding STI clinic. History of prior treatment was reported in 25.6% of total cases. Delay in diagnosis or misdiagnosis further results in spread of infection to sexual partners during this period.
Limitation(s)
The limitation of the present study includes diagnosis of many cases was based on clinical examination and syndromic approach and that all of the cases were not confirmed with additional confirmatory tests such as histopathology, culture and microscopy.
Conclusion(s)
The prevalence of HIV is high among the cases of STI. The most important step in control of HIV is prevention and treatment of STIs. The recent trends show apparent increase in viral STIs compared to bacterial STIs. For prevention of STIs, it is important to emphasise on counseling and education, condom promotion, compliance with treatment and contact tracing of sexual partners and their treatment. Primary prevention can be achieved by providing formal sex education and secondary prevention by means of rapid diagnosis and management of STIs. Large proportion of cases in the study showed high risk sexual behaviour such as multiple sexual partners, sexual contact with CSWs, and unprotected sexual practices. This highlights the necessity of sexual health awareness programs, especially targeted towards young and vulnerable population.
HIV: Human immunodeficiency virus; VDRL: Venereal disease research laboratory
STI: Sexually transmitted infections; VDRL: Venereal disease research laboratory; RPR: Rapid plasma reagin; HIV: Human immunodeficiency virus; GUD-H: Genital ulcerative disease-herpetic