Hearing loss is one amongst commonest sensory disorder which is estimated to affect people worldwide [1]. The reported prevalence of permanent bilateral hearing loss identified by newborn hearing screening programs was 1.61/1000 infants in India [2]. The absence of external hearing stimuli can cause delayed speech, language development, development of mental status and learning difficulties too can be seen. This will result in academic failure and social problems [3]. For the children’s with impaired hearing, the first six months after birth are important. Screening of neonatal hearing has a significant role in preventive healthcare services. Therefore, measures has to be taken as soon as possible to reduce the difficulties arising from hearing deprivation. To accomplish this, it’s necessary to spot the hearing loss in neonates as soon as possible [4].
A number of neonates have been identified through early Universal Newborn Hearing Screening (UNHS) programs which have provided the evidence to achieve nearly normal language acquisition by three years of age [5]. The hearing screening procedures for newborns and infants are simple and can be performed while the infant is resting quietly [6]. The two most common screening methods used with infants are OAEs and Automated Auditory Brainstem Response (AABR) [7]. OAE test is done widely in hospital under newborn hearing screening program, which represents a big advantage for screening young children. It is an objective method which screens hearing in a range of sound frequencies important for normal speech and language development.
In newborns the presence of vernix caseosa in the outer auditory canal and retained fluid in the Middle Ear (ME) in CD may directly interfere with the result of the UNHS in the first 24 hours after birth [8]. The ME space is filled with fluid until delivery. The movement through the birth canal helps push the fluid out of the ME space. However, fluid can remain in the ME space and cause a conductive hearing loss in newborns. This can be seen in CD as the passage of neonate from birth canal is by-passed. The retained fluid in ME in such cases takes a day or two to clear. To understand the temporary conductive hearing loss during the first few days after birth, it has been suggested that this is mainly due to the presence of amniotic fluid in the ME cavity at birth and its subsequent clearance [9]. Screening of the neonatal hearing is an important tool for the detection and rehabilitation of hearing loss on time. Priner R et al., showed most of the amniotic fluid is cleared from the neonatal ME cavity by water outflow into the blood due to osmotic pressure gradients. This occurs few hours to a day after birth. It has been speculated that in CD fluid resorption is delayed from the middle ear similar to that occurring in their lungs, a condition known as Transient Tachypnea of the Newborn (TTN) [10].
The aim of this study was to investigate the influence of mode of delivery on the results of Oto-Acoustic Emission test.
Materials and Methods
This cross-sectional study was performed in Newborn hearing screening centre, Department of Otorhinolaryngology, Dhiraj Hospital, SBKS Medical Institute and Research Centre, Vadodara, Gujarat, India. The project was approved by Sumandeep Vidyapeeth Institutional Ethics Committee in January 2019 (SVIEC /ON/Medi/SRP/19001).
Inclusion criteria: A total of 500 Neonates born beyond 37 weeks of gestation in the hospital between January 2019-July 2019, without any associated risk factors and normal ear findings (based on clinical history, general and ENT examination done with help of Bull’s lamp and Otoscope) were included. The parent/guardian provided a written consent for the neonatal hearing assessment and enrolment into the study.
Exclusion criteria: After delivery infants admitted in the ICU with or without mechanical ventilation and presence of any other identified congenital health problems.
In the medical institute study, vaginally delivered neonates (spontaneous, vacuum or forceps delivery) are discharged 48 hours after birth, whereas in caesarean delivery infants are discharged on the 3rd day of birth. This study was done as a part of Neonatal screening programme by the authors with the help of Audiology Unit over the concerned population. Hearing screening tests were performed in a sound treated room by trained staff. Care was taken to keep the neonates quiet and still. Infant’s external ear canal were cleaned to reduce vernix caseosa accumulation. Canal’s diameter size probe was placed in the external auditory canal and screening tests were performed.
Otometrics- Madsen capella starter kit with ER-10D OAE Probe and OTO-suite software v4.73.02 was used for the assessment. Click stimulus was offered at the rate of 21.1-27.7 per second. Total 1000-2000 clicks were given per recording in each ear. The time required for the test was about 3-5 min. (Transient Evoked OAEs) TEOAE was used for screening test. The criteria were set on basis of signal to noise ratio. SNR >OR=6dB was considered “passed” and SNR of <6dB was “referred” or “follow-up”.
The first emission test (OAE1) was performed within 24 hours after birth. Those who could not clear this test were scheduled for the second emission test (OAE2) at 48-72 hours. Those who did not pass this second test were invited for an Auditory Brainstem Response (ABR) test at three months. For each neonate included in the study, the timing and results of OAE tests were recorded. The incidence of false positives on OAE was duly noted in both groups and correlated with the timing of the OAE after analysis with appropriate statistical tests.
Statistical Analysis
Statistical analysis was performed using Statistical Package for the Social Sciences (SPSS) version 20.0. The results of effect of CD on OAE test at different time duration were noted and studied. The p-value was calculated by chi-square test and p-value <0.05 was considered statistically significant.
Results
The number of male patients were 218 (44%) and female were 282 (56%). A sample size of 500 neonates was studied, of which 194 were born by CD and 306 by normal delivery [Table/Fig-1]. In comparison to the CD group, more vaginally delivered neonates cleared the OAE-1 test at 24 hours (p=0.001). After 48 hours on repeat OAE-2, 77.78% (14 out of 18) neonates passed the test who had initially failed the OAE performed within 24 hours (p=0.778) [Table/Fig-2,3 and 4].
| Mode of delivery | Frequency | Percentage |
|---|
| Vaginal Delivery (VD) | 306 | 61.2 |
| Caesarean Delivery (CD) | 194 | 38.8 |
| Total | 500 | 100 |
Data for OAE done before 24 hours and repeated after 48 hours in failed OAE.
| Delivery | Within 24 hours | Repeat OAE in fail neonates after 48 hours |
|---|
| Pass | Fail | p-value | Pass | Fail | p-value |
|---|
| Caesarean | 152 (78.35%) | 42 (21.65%) | 0.001 | 34 (80.95%) | 8 (19.05%) | 0.778 |
| Vaginal | 288 (94.12%) | 18 (5.88%) | 14 (77.78%) | 4 (22.22%) |
| Total | 440 (88%) | 60 (12%) | 48 (80.00%) | 12 (20.00%) |
p-value<0.05 statistically significant
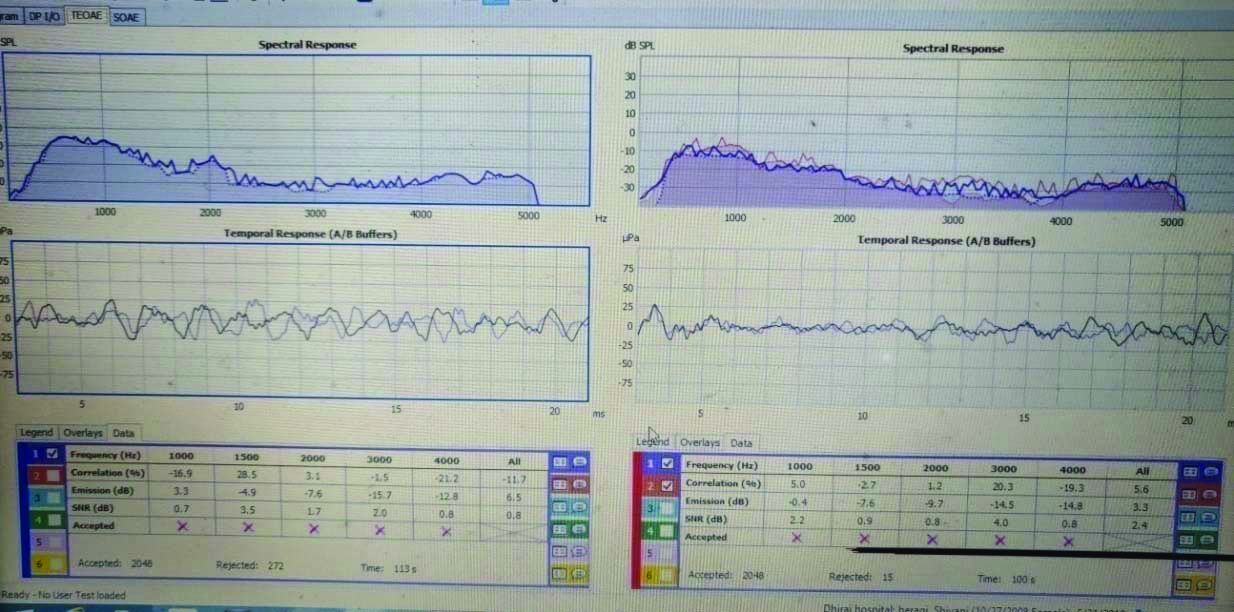
“Fail” OAE recorded after birth in a neonate of Caesarean Delivery (CD).
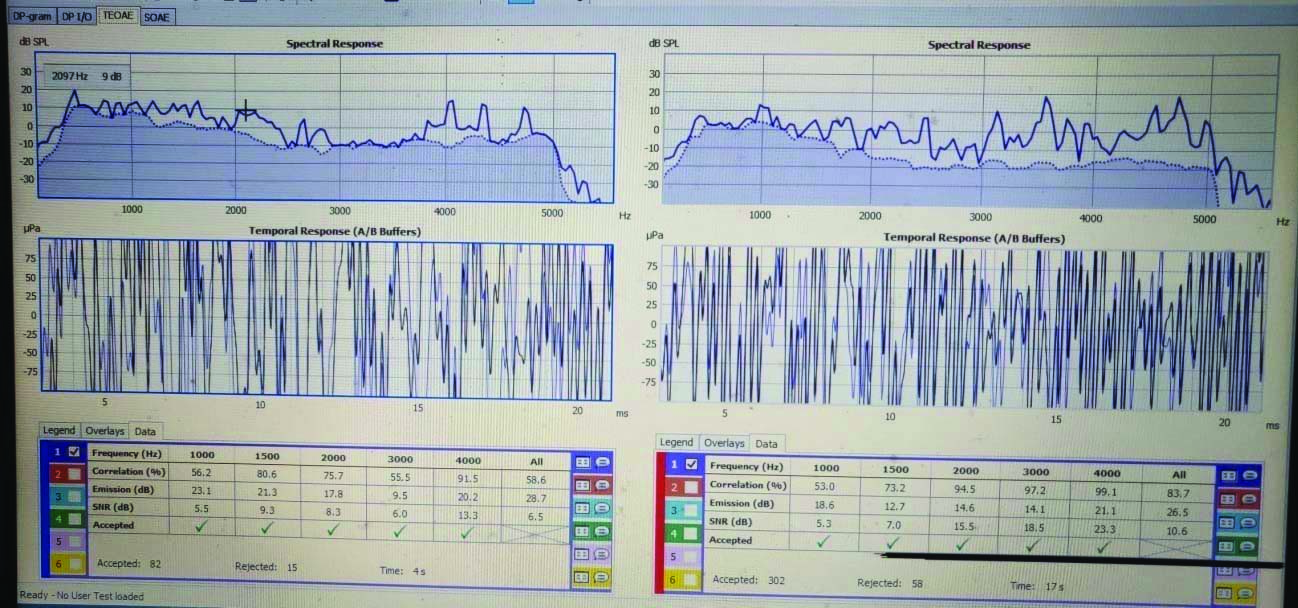
“Pass” OAE recorded after birth in a neonate of Vaginal Delivery (VD).
Failure on first OAE (at 24 hrs) was 3.5-fold higher in CD infants (21.6%) than in VD infants (5.88%). The rate of false positive in CD is higher than VD. Rate of false positive test was three times higher in CD as compared to VD that is 4.12% and 1.3%, respectively.
Discussion
Hearing loss has a catastrophic effect not only on the child’s verbal communication but also ability to learn language. Left undetected, hearing disability in infants can negatively impact verbal, educational, psychological and socioeconomic abilities. These negative effects can be eliminated or at least can get diminished through early intervention.
Neonatal Hearing Screening has been recommended since 1990’s and has been demonstrated to be effective in the diagnosis of hearing loss after birth. OAE and Brainstem Evoked Response Audiometry (BERA) are two commonly used objective tests for childhood deafness screening and diagnosis respectively. The current study focused on OAE test findings in neonatal screening and effect of mode of delivery on the findings.
Some neonates do not pass in the first screening test and the most of them show False Positives (FPs) result. Due to FP results increase family financial burden and parents stress. Finding causative factors which lead to false positive result and correcting those factor can help in reducing financial cost and anxiety. One such factor- mode of delivery has been taken into consideration in this study.
Among the 500 neonates included in this study, failure on primary OAE-1 (at 24 hrs) was 3.5-times more in CD (21.6%) than in VD (5.88%). Xiao et al., Smolkin et al., study showed that in primary screening test in CD: FPs result is higher than VD [7,11]. Smolkin H et al., also showed that OAE should be done >48 hour after delivery to decrease the failure rate [11].
Farahani et al., study results varied which showed high failure of first OAE in VD than CD infants. The failure of the first OAE of infants born by VD was more than the CD. They showed that FP rate was found 1.5-fold higher among those born by VD than in those born by CD. A steep drop was noted in FP rates in the OAE2 done in 2nd week after birth and no notable changes were associated with modes of delivery [12].
According to the present study, Mode of delivery has a significant role in the FP 1st hearing assessment. The screening test in the early hours after delivery causes high FP cases in CD as compared to VD. The study revealed that delayed screening time reduces FP in both CD and VD, whereas the study by Farhani F et al., showed a decrease in FP rate in CD whereas VD had no relation with screening time. So, generally mode of delivery has a significant role for deciding FP result during 1st hearing assessment [12].
In the early hours after delivery, FP result is most likely due to retained fluid in middle ear and debris in external ear. Study by Doyle KJ et al., said that the prevalence of occluding external auditory canal by vernix is 14.3% before 24 hours in new born which is reduced to 11.7% after 24 hours [13]. If hearing screening were done after 24 hours, only 30% of infants would contain vernix and 12% would have occluding vernix, which could lead to screening error. As vernix could be present in External Auditory Canal (EAC) in both the modes of delivery, care was taken to clear the vernix and debris from external auditory canal before testing.
Delayed absorption of fluid from the ME in new born causes reduced conductive sound transmission resulting in failure to the OAE test. To reduce the FP rate one should delay screening time as absorbed ME fluid reduces failed OAE test. Delayed absorption of middle ear fluid could be reason behind the higher failure rate of OAE screening in CD infants.
There is no consensus worldwide regarding the optimal timing for performance of first OAE test. Usually, babies born by VD and in good health conditions are discharged from hospital in 24 hours after they are born, whereas those born from caesarean sections also in good health are discharged after 48 hours. Thus, the hearing screening often has to be conducted within 24 hour from birth. In the current study, it was observed that there was a significant difference in the screening results of newborns tested within 24 hours and after 48 hours born by caesarean deliveries.
Thus, to reduce the cost of rescreening test as well as the stress caused by the referred test, at least in CD, the newborn screening may be delayed until discharge from hospital or performed after 48 hours, so that FP is reduced.
Limitation(s)
This study was carried out in a single centre and requires external validation. It requires a long term follow-up to assess permanent hearing loss. Larger sample size needs to be studied for more conclusive evidence.
Conclusion(s)
Neonates delivered by CD had significantly higher failure rates as compared to VD on first OAE, if performed within 24 hours. The authors speculate that CD is accompanied by retained fluid in ME which may impair neonatal hearing screening. The timing of first OAE should be postponed beyond 48 hours of age to minimise the neonatal false-positive hearing screen rates and efforts should be put to educate mothers about hearing screening.
p-value<0.05 statistically significant