Introduction
Anaemia affects about 800 million children and women worldwide. The most common causes of anaemia are IDA and BTT. The National Family Health Survey (NFHS4) carried out in 2015-16 reported the prevalence of anaemia in children (age 6 to 59 months) being 58.6%, 53.1% in women (15 to 49 years) and 22.7% in men (15 to 49 years) [1].
The overall prevalence of beta thalassaemia is 3-4% and is amongst commonest single gene disorders in India. The frequency of the beta-thalassaemia gene is population dependent. It is prevalent in a broad belt extending from the Mediterranean basin to Southeast Asia. The estimated population of beta thalassaemia carriers in the world is 1.5%, which is around 80-90 million, with around 60,000 carriers being born every year [2].
BTT and IDA are the most common causes of MCHC anaemia. The differential diagnosis between IDA and BTT is an important concern for every physician; to avoid unnecessary iron therapy, which has deleterious effect in the cases of beta thalassaemia. Definitive methods for differential diagnosis between BTT and IDA include quantitative detection of HbA2 on chromatogram and DNA mutation studies. However, these tests are too expensive and time-consuming for initial mass screening [3]. An alternative method of screening would be carrying out the red cell indices to screen population in suggestion of electrophoresis, chromatogram or DNA mutation studies.
It is a necessity to identify the suspected BTT individuals from routinely received laboratory samples for CBC to channelise them for appropriate diagnostic work-up in otherwise heavily attended tertiary level healthcare hospitals. As this involves additional High-Performance Liquid Chromatography (HPLC) testing for confirmation of BTT, it is important that such a screening index will help to recruit the patients for further studies. This would save on the cost borne by the individuals at treatment [3].
Modern blood cell analysers are relatively popular for their rapid throughput processing time and are relatively inexpensive. These electronic red blood cell counts and their indices are easily obtained by their in process internal calculations. These indices are considered preliminary screening tools in distinguishing IDA and BTT. Such publications exists in literature and the publications details ‘reflex’ HbA2 analysis when a proper cut-off for it is chosen [4].
Approximately, 40 mathematical indices have been proposed to evaluate and discriminate the two most common aetiologies of MCHC anaemia, IDA and BTT. But none of these indices are either 100% sensitive or specific. Moreover, there are discrepancies in the various indices proposed and studies by authors worldwide. The reason for this problem is not clear; possibly the reason could amount to geographical or regional differences amounting to the genetic differences in the genotype of BTT. The small number of study populations or the age groups considered in the studies or analytical factors could also be playing role in these discrepancies.
A definitive differential diagnosis between BTT and IDA is based on the result of HbA2 electrophoresis and serum iron studies. Electronic cell counters have been used to determine red cell indices as a first indicator of BTT. The intent of using these red blood cell indices is to recognise the patients of MCHC anaemia who would be needing an appropriate follow-up and to cut their investigative costs.
With this backdrop and index that ideally answers the very query whether the case of MCHC anaemia has an underlying aetiology of IDA or BTT. The present review is novel in the context that the most popular red cell indices used worldwide for aforesaid purpose have been analysed through methods of systematic review to suggest a practicable, ideal and dependent red cell index that would often discriminate between BTT and IDA. The present analytical review was conducted to ascertain the reliability of popularly practiced red cell indices at suggesting BTT and IDA in the morphological class of MCHC anaemia.
Materials and Methods
Systematic Literature Search
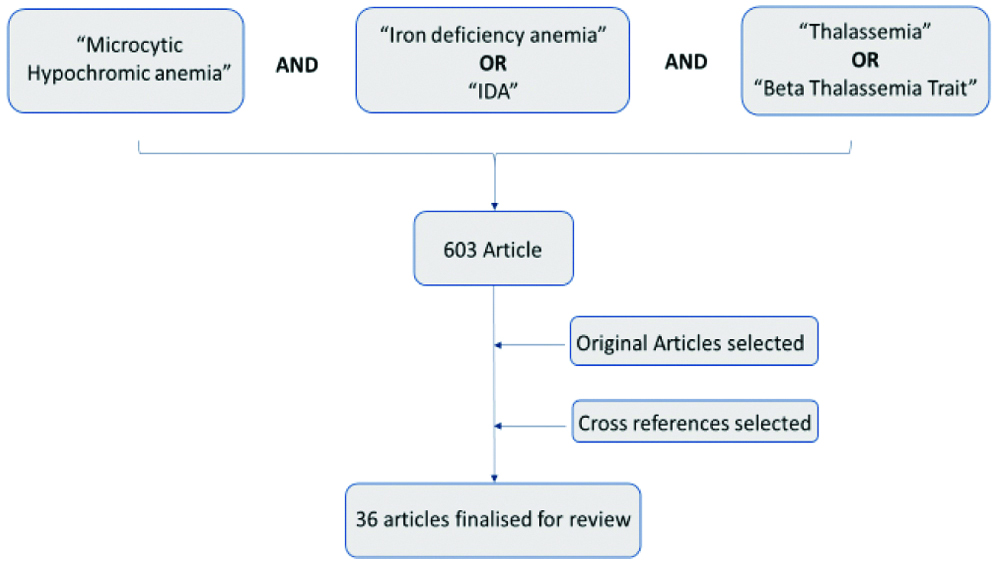
The Pubmed search was made to find the relevant literature on red blood cell indices. The combination of search words of “MCHC anaemia” AND “IDA” OR “IDA” AND “thalassaemia” OR “BTT” in the advanced search builder. Search engine revealed 603 articles as illustrated in [Table/Fig-1]. The original articles for all the discriminant indices and the cross-reference listed in the original references not covered in the initial literature search were also collected. English language articles were selected as the language restriction cap. However, the present review did not disregard the studies that proposed new indices, where their formula was compared with the existing indices for various statistical entities.
Process illustrating the primary literature search for the study.
Red cell indices which were statistically analysed, which appeared in literature for at least on 5 instances or more. The articles selected for analysis were dealing with Mentzer index, Bessman index, Green & King index, Srivastava index and Sirdah index in order of their evolvement over past few years.
Study Selection
The titles and abstracts were screened to identify relevant studies by all authors of past two decades. The following inclusion criteria were used: (i) Studies investigating the reliability of automated red cell indices obtained to discriminate between IDA and thalassaemia trait; (ii) retrospective and prospective observational studies; (iii) studies done in human participants; (iv) study populations without any known history of chronic disease and on treatment; (v) articles published in indexed scientific journals; (vi) studies based on primary data; and (vii) studies retrieved from Pubmed published from 2001 till the date of present review. Articles included in the study were not restricted by age and sex of the subjects. The full texts were retrieved from all eligible studies.
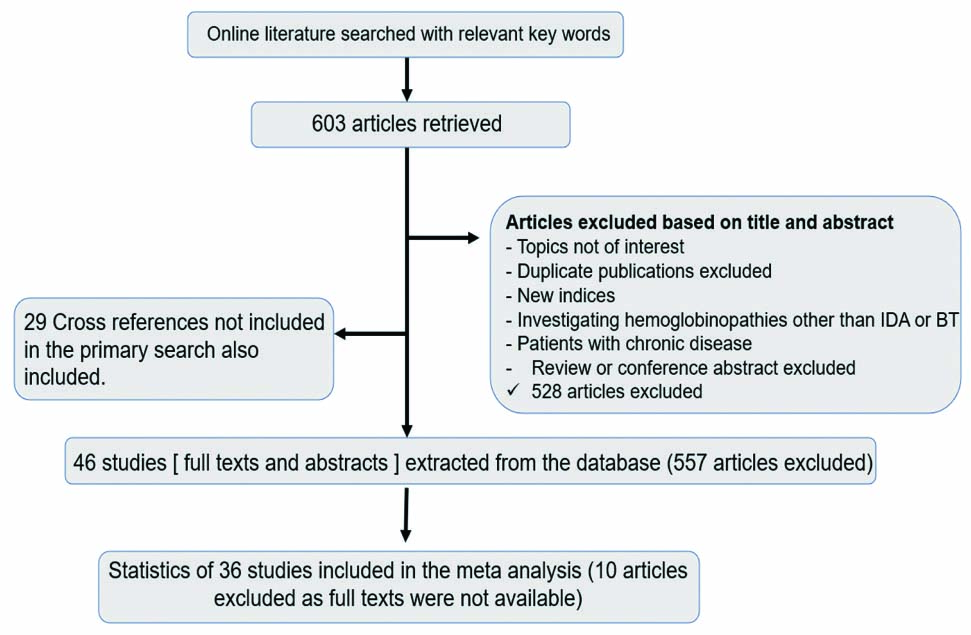
Further, exclusion criteria applied for the present study were: (i) studies introducing new formulas for distinguishing IDA from thalassaemia trait; (ii) articles studying the impact of investigative tools other than haematological indices for distinguishing MCHC anaemia; (iii) studies investigating populations with chronic disease; and (iv) Haematological indices evaluating aetiologies other than IDA and thalassaemia trait. The reference list of selected articles were scanned to identify additional relevant articles meeting the eligibility criteria for the present study. This process is illustrated in [Table/Fig-2].
Flowchart illustrating the process of systematic literature search.
Characteristics of all Included Studies
The characteristics of all 36 studies are summarised in [Table/Fig-3]. The remaining 6 articles were not available for their full texts and therefore, were not included for the purpose of review. A total of 30,835 participants were included in the systematic review with overall age ranging from 1 year to 93 years. Study sample size ranged from 45 to 3030 participants. A total of 28,638 subjects were adults. A total of 12 authors included paediatric population in their studies, which comprised of a total 2,197 participants [2,4,5,17,18,24,25,30,32,33,39,41]. Studies included were conducted in various geographical locations [2-5,10-14,17,18,22,24-47] illustrated in [Table/Fig-3]. Both retrospective and prospective original studies were included in the analysis.
Summary of 36 studies included for analysis (total population).
| Total participants | 30,835 |
| Adults | 28,638 |
| Pregnant women | 1,205 |
| Children | 2,197 |
| Countries (number of studies included)[Reference number] | India (9) [2,4,17,18,25,37,38,44,45], Turkey (5) [5,27,29,30,33], Iran (4) [3,13,34,43], Pakistan (3) [28,35,40], China (2) [24,41], Spain (2) [14,26], Palestine (1) [10], Saudi Arabia (1) [11], Thailand (1) [12], Greece (1) [22], Brazil (1) [31], Italy (1) [32], Taiwan (1) [36], Egypt (1) [39], Makkahregion (1) [42], North Africa (1) [46] and Kuwait (1) [47]. |
| Types of indices (Number of studies) | Mentzer index (36), Green and King index (31), Bessman index (24), Srivastava index (32), Ehsani index (17) and Sirdah index (13). |
Indices and their Methods of Calculation and Cut-off
For the purpose of this analysis, five indices popular in literature commonly assessed for discriminating the MCHC picture of red blood cells are included, i.e., Mentzer index (MCV/RBC), Srivastava index (MCH/RBC), Bessman index (RDW), Green and Kind index (MCV2×RDW/Hb×100), and Sirdah index (MCV-(5×Hb)-RBC-3.4). The indices and their formulae are summarised in the [Table/Fig-4] [6-10].
Indices with their year of introduction, formula and original cut-off values as describes by their authors.
| Index | Year | Formulae | Cut-off value |
|---|
| Mentzer | 1973 | MCV/RBC | 13 |
| Srivastava | 1973 | MCH/RBC | 3.8 |
| Bessman | 1979 | RDW | 15 |
| Green and King | 1989 | MCV×MCV×RDW/Hb×100 | 65 |
| Sirdah | 2007 | MCV-(5×Hb)-RBC-3.4 | 27 |
MCV: Mean corpuscular volume, RBC: Red blood cell, RDW: Red cell distribution width, Hb: Haemoglobin
Statistical Tools
The comparisons of these indices were calculated against the final diagnostic mode of complete iron studies, Hb electrophoresis, chromatograms and DNA sequencing in the required cases as deemed fit by the authors of respective studies. The statistical interpretation of diagnostic utilisation of cut-offs that were frequent for individual red cell index are summarised in [Table/Fig-5] along with their reference numbers against the index [6-10].
Indices and their cut-off values.
| Index | Cut-off value | IDA | BTT |
|---|
| Mentzer | 13 | >13 | <13 |
| Srivastava | 38 | >3.8 | <3.8 |
| Bessman | 15 | >15 | <15 |
| Green and King | 65 | >65 | <65 |
| Sirdah | 27 | >27 | <37 |
The statistical values were drawn using Stata version MP15, Systech Technograph Services (2018). The values of SN and SP were extracted from the reviewed studies in the present study. SN (also called the true positive rate) measures the proportion of actual positives that are correctly identified and SP (also called the true negative rate) measures the proportion of actual negatives that are correctly identified. Youden’s index, a way of summarising the performance of a diagnostic test was also noted from the studies reviewed. The formulae used for calculating SN, SP and Youden’s index as used in the review article were as followed:
Sensitivity=True Positive/True Positive+False Negative×100.
Specificity=True Negative/True Negative+False Positive×100.
Youden’s index=(sensitivity+specificity)-100
Results
The present study included 36 original studies for the analysis to determine the reliability of various indices for IDA and BTT. Combining all the studies’ participants, a total of 30,835 subjects were examined. Out of these 36 studies, 12 authors included paediatric population and the aggregated study population for this age group included in our analysis came out to be of 2,197 participants (7.12%) [2,4,5,17,18,24,25,30,32,33,39,41]. The age group in all the included articles ranged from 1 year to 93 years and a slight preponderance was noted in the female sex in the adult age groups(1.2:1) [2-5,10-14,17,18,22,24-47].
Out of the 36 studies in the present analysis, 9 studies were conducted in India [2,4,17,18,25,37,38,44,45]; 5 were carried out in Turkey [5,27,29,30,33]; 4 were studied in Iran [3,13,34,43]; 3 were conducted in Pakistan [28,35,40]; 2 each were carried out in Spain [14,26] and China [24,41] and 1 each were carried out in Palestine [10], Saudi Arabia [11], Thailand [12], Greece [22], Brazil [31], Italy [32], Taiwan [36], Egypt [39], Makkahregion [42], North Africa [46] and Kuwait [47].
Nearly all the studies used automated analysers to obtain red cell parameters to calculate the haematological indices for their accuracy and efficiency at internal calculation. Most of the them mentioned the automated analysers used in their study. Five authors used Sysmex XE-2100 [4,24,31,41,42], two used LH-750 Beckman Coulter [18,46], two used Coulter Counter (London, UK) [30,34], two used Sysmex XS-800i [25,38]; and rest of the authors used Sysmex K 1000 [3]; Siemens Adiva 2120 [5]; LH 5009 [11]; MEK-8222K, Nihon [12]; Sysmex K-800 [13]; CELL-DYN Sapphire [14]; Adiva 2120 [26]; Sysmex XT2000i [27]; Automated haematology analyser, Nihon [28]; Abbott Cell-Dyn 4000 [29]; ABX Penta DX-120 [31]; Coulter Counter Max M [33]; Hema Count Plus [35]; LH-780 [37]; Coulter Gen System 2, Beckman [39]; KX-21 Sysmex [44] and Backman HMX [47]. The older Coulter analysers showed relatively lower diagnostic performance as compared to the newer generation automated analysers.
The sample size varied vastly among the studies included in the present analysis ranging from 45 to 3030 subjects. The total number of subjects evaluated for Mentzer Index was highest amounting to 17,862; second was 16,043 for Srivastava index; 12,921 for Green and King index; 10,902 for Bessman index and lowest came down to 5,134 for Sirdah index. The overall SN and SP for the above-mentioned indices were calculated along with the Youden’s index. Mentzer index showed a SN of 76.82% and SP of 84.87%, and SN and SP for Bessman index was 69.45% and 70.6% respectively, Green and King showed a SN of 79.37% and a SP of 82.54%, Srivastava index had 70.84% SN and 77.88% SP and Sirdah index showed SN of 74.94% and SP of 84.296%. The Youden’s index for Mentzer index was 61.69%, 40.05% for Bessman index, 61.91% for Green and King index, 48.72% for Srivastava index and 59.236% for Sirdah index; summarised in [Table/Fig-6] [6-10].
Summarised values of Sensitivity, Specificity and Youden’s index of the five indices included in the present study.
| Index | Sensitivity | Specificity | Youden’s index |
|---|
| Mentzer | 76.82 | 84.87 | 61.69 |
| Srivastava | 70.84 | 77.88 | 48.72 |
| Bessman | 69.46 | 70.6 | 40.05 |
| Green and King | 79.37 | 82.54 | 61.91 |
| Sirdah | 74.94 | 84.296 | 59.236 |
The present review observed that Green and King index had the best Youden’s index followed closely by Mentzer index and Sirdah index. The Youden’s index of Srivastava index and Bessman index was much lower than the rest of the indices assessed.
Discussion
An IDA and BTT are the two most important causes for hypochromia and microcytosis. These two conditions are encountered rather frequently, particularly in outpatient populations in areas with traditionally high prevalence [11-16]. Prevalence of anaemia is high in India and is widely seen in all age groups, the major cause of which is IDA [17]. IDA is most important cause of MCHC anaemia in north Himalayan region [18]. The National Family Health Survey (NFHS-4) of 2015-16 reveals the prevalence of anaemia as 58.6% in children, 53.2% in nonpregnant females, 50.4% in pregnant women, and 22.7% in adult men [1]. As per Census of India 2011, there are about 35 to 45 million (3-4% of 1.21 billion population) beta thalassaemia carriers in our ethnocultural and multilingual country [19].
Since 1973, several indices have been introduced in an attempt to improve the quality of diagnosis and differentiation between these two conditions by investigators such as Mentzer WC; Green R and King R; Srivastava PC and Bevington JM [6,8,9]. These indices used red cell parameters obtained easily by routine blood count, which is widely available and inexpensive to perform [20].
These indices incorporate MCV, MCH, RBC count, RDW, and Hb in various combinations. For a certain degree of anaemia, RBC tend to be more microcytic and hypochromic in BTT than in iron deficiency states. As a result, MCV and MCH tend to be lower in BTT compared to IDA [21]. On the contrary, RBC count tends to be higher in BTT than in IDA. Thus, most indices use MCV, MCH, and RBC count to amplify these differences. Another significant difference between these two types of anaemia is the level of anisocytosis [8]. In the state of iron deficiency, the bone marrow continuously produces red cells and their iron stores progressively decreases. As a result, they tend to be more and more microcytic. The anisocytosis develops due to coexistence of normocytic cells as well as microcytic cells in the peripheral blood since life span of RBCs is 4 months. Moreover, iron deficiency leads also to poikilocytosis, which also increases the width of red cells. On the contrary, the underlying patho-genetic anomaly in BTT has no fluctuations, and as a result, the bone marrow produces a constantly uniform population of microcytic, hypochromic RBCs. Consequently, RDW, which is an index of anisocytosis, tends, theoretically, to be increased in IDA and normal in BTT [22].
To safely differentiate between BTT and IDA, a physician needs a battery of investigations including HbA2, peripheral blood smear, serum ferritin, iron, TIBC levels and transferrin saturation [22]. But the drawbacks of these tests are that many of them are expensive and require sophisticated laboratories [15]. And these facilities might not always be available to the 68.8% populations of India that resides in the rural areas [19]. These indices are used to reduce the time, cost and unnecessary laboratory procedures [3,23]. These indices helps to select appropriate individuals for a more detailed investigation [5]. Majority cases of BTT may be misdiagnosed as IDA as they might be asymptomatic or have nonspecific haematological findings [3,24]. Another issue to be considered in cases of BTT patients are mutations and migrations cases of BTT patients are mutations and migrations. Literature documents more than 200 mutations noted so far, and also according to the extent of the reduction of beta chain output, these mutations have been divided into severe, mild and silent [25]. Thalassaemia now affects residents of almost every nation in the world due to rise in migrations in the last few decades [14,26]. Due to intermixing of different ethnic populations, BTT is also being reported, increasing and co-existing with IDA [18].
According to the original published papers by the authors of theses indices, their SN in detection of BTT and IDA is approximately 100% [6-8,10]. However, later studies failed to confirm these results carried out in various countries and regions which included different ethnic groups and age criteria [3,13,18,22,27-29]. The summary is illustrated in [Table/Fig-7] [2-5,10-14,17,18,22,24-47].
Summarises different study results focused on RBC discrimination index [2-5,10-14,17,18,22,24-47].
| Studies | Country of source | Beta thalassaemia patients | Youden index | Favourindex |
|---|
| 1. Tripathi N et al., [2] | India | 185 | 67.1 | MI** (at cut-off ≤12.54) |
| 2. Miri-Moghaddam E and Sargolzaie N [3] | Iran | 100 | 68 | G & K‡ |
| 3. Sehgal K et al., [4] | India | 124 | 70.7 | MI** (at cut-off>14) |
| 4. Vehapoglu A et al., [5] | Turkey | 154 | 81 | MI** |
| 5. Sirdah M et al., [10] | Palestine | 1272 | 69 | G & K‡ |
| 6. Jameel T et al., [11] | Saudi arabia | 32 | 83 | RDWI* |
| 7. Plengsuree S et al., [12] | Thailand | 102 | 91.18 | RDW/RBC |
| 8. Batebi A et al., [13] | N/A | 273 | 88 | MI** |
| 9. Urrechaga E et al., [14] | Spain | 150 | 69 | MI** |
| 10. Sharma A et al., [17] | India | 300 | 53 | MI** |
| 11. Chandra H et al., [18] | India | 42 | 53.66 | RDW†† |
| 12. Ntaios G et al., [22] | Greece | 373 | 71 | G & K‡ |
| 13. Shen C et al., [24] | China | 127 | 81 | RDWI* |
| 14. Piplani S et al., [25] | India | 72 | 81.3 | MI** |
| 15. Urrechaga E [26] | Spain | 101 | 81.8 | G & K‡ |
| 16. Okan V et al., [27] | Turkey | 100 | 91 | S & L§ |
| 17. Ullah Z et al., [28] | Pakistan | 230 | 93 | RDWI* |
| 18. Beyan C et al., [29] | Turkey | 66 | 74 | RBC mass |
| 19. Demir A et al., [30] | Turkey | 37 | 80 | RDWI* |
| 20. Matos JF et al., [31] | Brazil | 47 | 75 | RDWI* |
| 21. Ferrara M et al., [32] | Italy | 215 | 64 | E & F† |
| 22. Nalbantoğlu B et al, [33] | Turkey | 62 | 58 | E & F† |
| 23. Ehsani MA et al., [34] | Iran | 154 | 90 | MI** |
| 24. Niazi M et al., [35] | Iran | 223 | 72 | RDWI* |
| 25. Huang TC et al., [36] | Taiwan | 453 | 91 | S & L§ |
| 26. Kumar A et al., [37] | India | 43 | 72 | RDWI* |
| 27. Gupta P et al., [38] | India | 48 | 61.85 | MI** |
| 28. Pessar SA [39] | Egypt | 58 | 54.02 | RDWI* |
| 29. Hafeez Kandhro A et al., [40] | Pakistan | 300 | 54.97 | Kerman2 |
| 30. Tong L et al., [41] | China | 46 | 84 | Joint Indicator A |
| 31. Zaghloul A et al., [42] | Makkah | 123 | 84.7 | E & F† |
| 32. Bordbar E et al., [43] | Iran | 151 | 72.3 | S & L§ |
| 33. Mukhopadhyay D et al., [44] | India | 579 | 81.4 | S & L§ |
| 34. Garg S et al., [45] | India | 255 | 93.8 | RDW†† |
| 35. Sahli CA et al., [46] | North africa | 57 | 88 | Srivastava |
| 36. AlFadhli SM et al., [47] | Kuwait | 47 | 98.2 | E & F† |
*RDWI: Red cell distribution index; †E & F: England and Fraser index; ‡G & K: Green and King index; §S & L: Shine and Lal index; **MI: Mentzer index; ††RDW: Red cell distribution width
Five indices were included for the analysis and results were relied on Youden index that takes into account of both SN and SP, and gives an appropriate measure of validity of a particular index. Green and King Index and Mentzer index showed relatively higher values of SN, SP and Youden index as depicted in [Table/Fig-6].
A vast range of variations in results were noted in the studies included which possibly could be due to a number of reasons like the type of automated analysers used by different authors. Another reason could be the diverse population by age and groupings of the patient, like Chandra H et al., divided their sample size in three groups, group I, II and III comprising of IDA, BTM and IDA+BTM, respectively [18]. Whereas, Piplani S et al., divided their population in two groups, one of BTT and second of IDA patients [25]. Some authors also stated the presence of different molecular spectrum of beta thalassaemia disorders in various countries affecting the values of RBC parameters [32,48]. Furthermore, the participant’s age in the included studies were ranging from 1 year to 93 years. Some authors focused their study on only children, while some based their studies on pregnant females [2,5,24,30,33,39,41]. The undiagnosed presence of co-existing iron deficiency in beta thalassaemia carriers could also affect the results [37].
In view of the disparities noted in the results, many authors have suggested to adjust the cut-off values for populations based on the geographical locations [3,28]. Sazawal S et al., also pointed out that an increase in RDW values may occur in children with IDA, and hence should be adjusted to allow an early detection of IDA before reduction in MCV occurs [15]. More studies are suggested in reports of the few authors in high prevalence regions for all age groups, especially in children and pregnant women to define the cut-off ranges for particulate set of population [2,36,43,44,49].
Differentiation of the two underlying aetiologies of MCHC anaemia is clinically significant, particularly in high prevalence region like India, in order to start a proper treatment protocol. The correct identification of BTT is especially important, as the management of BTT patients is not only expensive but also causes extreme distress to patient and family due to compromised quality of life and to avoid unnecessary iron medication. Carriers of BTT are often misdiagnosed as those suffering from IDA [25].
With all the available red cell indices reviewed in the present study, there lies a common disadvantage of interference of dissimilar parameters making it difficult for inter-indices comparison even though their stated SN and SP are high.
The observations within the present analysis bring the recommendation that one of these indices should be a part at picking up the patients for their treatment suffering from IDA. An attempt should be made to flag these indices on the electronic cell counters that would alert the physicians for further work-up of BTT.
Conclusion(s)
The review of studies carried out points at their inherent but distinct advantages at screening of MCHC anaemia for their underlying aetiologies of IDA and BTT. Though these indices are not entirely reliable but observed to possess potential to discriminate the above entities which further can be subjected for definitive test for diagnosis which includes iron studies, Hb electrophoresis, chromatography and DNA sequencing as the case may be. The resource limited hospitals can put these indices in the practice of laboratory medicine atleast to segregate the patients as of IDA and BTT for their appropriate management. The patients of BTT, who may unnecessarily receive iron therapy instead of chelating therapy may have deleterious effects, which may be saved by adopting one of the red cell indices as screening test. Amongst the plurality of red cell indices, Green and King index and Mentzer index can be recommended as screening indices to discriminate the patients of MCHC anaemia for IDA and BTT.
*RDWI: Red cell distribution index;
†E & F: England and Fraser index;
‡G & K: Green and King index;
§S & L: Shine and Lal index; **MI: Mentzer index;
††RDW: Red cell distribution width
[1]. National Family Health Survey (NFHS-4), 2015-16. Mumbai: IIPS; [accessed on September 10, 2018]. International Institute for Population Sciences. Available from: http://rchiips.org/nfhs/NFHS- 4Reports/India.pdf. [Google Scholar] [Google Scholar]
[2]. Tripathi N, Soni JP, Sharma PK, Verma M, Role of haemogram parameters and RBC indices in screening and diagnosis of beta-thalassaemia trait in microcytic, hypochromic Indian childrenInt J Hematol Disord 2015 2(2):43-46. [Google Scholar]
[3]. Miri-Moghaddam E, Sargolzaie N, Cut-off determination of discrimination indices in differential diagnosis between iron deficiency anaemia and β-thalassaemia minorInternational Journal of Hematology-Oncology and Stem Cell Research 2014 8(2):27 [Google Scholar]
[4]. Sehgal K, Mansukhani P, Dadu T, Irani M, Khodaiji S, Sehgal index: A new index and its comparison with other complete blood count-based indices for screening of beta thalassaemia trait in a tertiary care hospitalIndian J Pathol Microbiol 2015 58(3):31010.4103/0377-4929.16286226275252 [Google Scholar] [CrossRef] [PubMed]
[5]. Vehapoglu A, Ozgurhan G, Demir AD, Uzuner S, Nursoy MA, Turkmen S, Hematological indices for differential diagnosis of beta thalassaemia trait and iron deficiency anaemiaAnaemia 2014 2014:57673810.1155/2014/57673824818016 [Google Scholar] [CrossRef] [PubMed]
[6]. Mentzer WC, Differentiation of iron deficiency from thalassaemia traitLancet 1973 1(7808):88210.1016/S0140-6736(73)91446-3 [Google Scholar] [CrossRef]
[7]. Srivastava PC, Bevington JM, Iron deficiency and/or thalassaemia traitThe Lancet 1973 301(7807):83210.1016/S0140-6736(73)90637-5 [Google Scholar] [CrossRef]
[8]. Bessman JD, Feinstein DI, Quantitative anisocytosis as a discriminant between iron deficiency and thalassaemia minorBlood 1979 53(2):288-93.10.1182/blood.V53.2.288.288 [Google Scholar] [CrossRef]
[9]. Green R, King R, A new red cell discriminant incorporating volume dispersion for differentiating iron deficiency anaemia from thalassaemia minorBlood Cells 1989 15(3):481-91. [Google Scholar]
[10]. Sirdah M, Tarazi I, Al Najjar E, Al Haddad R, Evaluation of the diagnostic reliability of different RBC indices and formulas in the differentiation of the- thalassaemia minor from iron deficiency in Palestinian populationInternational Journal of Laboratory Hematology 2008 30(4):324-30.10.1111/j.1751-553X.2007.00966.x18445163 [Google Scholar] [CrossRef] [PubMed]
[11]. Jameel T, Baig M, Ahmed I, Hussain MB, Alkhamaly M, Bin D, Differentiation of beta thalassaemia trait from iron deficiency anaemia by hematological indicesPak J Med Sci 2017 33(3):665-69.10.12669/pjms.333.1209828811791 [Google Scholar] [CrossRef] [PubMed]
[12]. Plengsuree S, Punyamung M, Yanola J, Nanta S, Jaiping K, Maneewong K, Red Cell Indices and Formulas Used in Differentiation of β-Thalassaemia Trait from Iron Deficiency in Thai AdultsHemoglobin 2015 39(4):235-39.10.3109/03630269.2015.104835226076394 [Google Scholar] [CrossRef] [PubMed]
[13]. Batebi A, Pourreza A, Esmailian R, Discrimination of beta-thalassaemia minor and iron deficiency anaemia by screening test for red blood cell indicesTurkish Journal of Medical Sciences 2012 42(2):275-80. [Google Scholar]
[14]. Urrechaga E, Hoffmann JJML, Izquierdo S, Escanero JF, Differential diagnosis of microcytic anaemia: the role of microcytic and hypochromic erythrocytesInt Jnl Lab Hem 2015 37(3):334-40.10.1111/ijlh.1229025181647 [Google Scholar] [CrossRef] [PubMed]
[15]. Sazawal S, Dhingra U, Dhingra P, Dutta A, Shabir H, Menon VP, Efficiency of red cell distribution width in identification of children aged 1-3 years with iron deficiency anaemia against traditional hematological markersBMC Paediatr 2014 14(1):810.1186/1471-2431-14-824428927 [Google Scholar] [CrossRef] [PubMed]
[16]. Matos JF, Borges KB, Fernandes AP, Faria JR, Carvalho MD, RDW as differential parameter between microcytic anaemias in “pure” and concomitant formsJornal Brasileiro de Patologia e Medicina Laboratorial 2015 51(1):22-27.10.5935/1676-2444.20150005 [Google Scholar] [CrossRef]
[17]. Sharma A, Sharma M, Sharma V, Evaluation of red cell distribution width in the diagnosis of iron deficiency anaemiaInternational Journal of Research in Medical Sciences 2016 4(9):3733-36.10.18203/2320-6012.ijrms20162603 [Google Scholar] [CrossRef]
[18]. Chandra H, Shrivastava V, Chandra S, Rawat A, Nautiyal R, Evaluation of platelet and red blood cell parameters with proposal of modified score as discriminating guide for iron deficiency anaemia and β-thalassaemia minorJournal of clinical and diagnostic research: JCDR 2016 10(5):EC3110.7860/JCDR/2016/17672.784327437228 [Google Scholar] [CrossRef] [PubMed]
[19]. Colah R, Italia K, Gorakshakar A, Burden of thalassaemia in India: The road map for controlPaediatric Hematology Oncology Journal 2017 2(4):79-84.10.1016/j.phoj.2017.10.002 [Google Scholar] [CrossRef]
[20]. Narchi H, Basak RB, Comparison of erythrocyte indices to differentiate between iron deficiency and alpha-thalassaemias in children with microcytosis and/or hypochromiaEast Mediterr Health J 2010 16(9):966-71.10.26719/2010.16.9.96621218724 [Google Scholar] [CrossRef] [PubMed]
[21]. England JM, Ward SM, Down MC, Microcytosis, Anisocytosis and the Red Cell Indices in Iron DeficiencyBr J Haematol 1976 34(4):589-97.10.1111/j.1365-2141.1976.tb03605.x990192 [Google Scholar] [CrossRef] [PubMed]
[22]. Ntaios G, Chatzinikolaou A, Saouli Z, Girtovitis F, Tsapanidou M, Kaiafa G, Discrimination indices as screening tests for β-thalassaemic traitAnn Hematol 2007 86(7):487-91.10.1007/s00277-007-0302-x17476506 [Google Scholar] [CrossRef] [PubMed]
[23]. Schoorl M, Schoorl M, van Pelt J, Bartels PC, Application of innovative hemocytometric parameters and algorithms for improvement of microcytic anaemia discriminationHematology Reports 2015 7(2):584310.4081/hr.2015.584326331001 [Google Scholar] [CrossRef] [PubMed]
[24]. Shen C, Jiang Y, Shi H, Liu J, Zhou W, Dai Q, Evaluation of Indices in Differentiation Between Iron Deficiency Anaemia and b-Thalassaemia Trait for Chinese ChildrenJ Paediatr Hematol Oncol 2010 32(6):510.1097/MPH.0b013e3181e5e26e20628316 [Google Scholar] [CrossRef] [PubMed]
[25]. Piplani S, Madan M, Mannan R, Manjari M, Singh T, Lalit M, Evaluation of various discrimination indices inAnnals of Pathology and Laboratory Medicine 2016 03(06):9 [Google Scholar]
[26]. Urrechaga E, Discriminant value of% microcytic/% hypochromic ratio in the differential diagnosis of microcytic anaemiaClinical Chemistry and Laboratory Medicine (CCLM) 2008 46(12):1752-58.10.1515/CCLM.2008.35519055451 [Google Scholar] [CrossRef] [PubMed]
[27]. Okan V, Cigiloglu A, Cifci S, Yilmaz M, Pehlivan M, Red cell indices and functions differentiating patients with the β-thalassaemia trait from those with iron deficiency anaemiaJ Int Med Res 2009 37(1):25-30.10.1177/14732300090370010319215670 [Google Scholar] [CrossRef] [PubMed]
[28]. Ullah Z, Khattak AA, Ali SA, Hussain J, Noor B, Bano R, Evaluation of five discriminating indexes to distinguish Beta-Thalassaemia Trait from Iron Deficiency AnaemiaJ Pak Med Assoc 2016 66(12):5 [Google Scholar]
[29]. Beyan C, Kaptan K, Ifran A, Predictive value of discrimination indices in differential diagnosis of iron deficiency anaemia and beta-thalassaemia traitEur J Haematol 2007 78(6):524-26.10.1111/j.1600-0609.2007.00853.x17419742 [Google Scholar] [CrossRef] [PubMed]
[30]. Demir A, Yarali N, Fisgin T, Duru F, Kara A, Most reliable indices in differentiation between thalassaemia trait and iron deficiency anaemiaPaediatr Int 2002 44(6):612-16.10.1046/j.1442-200X.2002.01636.x12421257 [Google Scholar] [CrossRef] [PubMed]
[31]. Matos JF, Dusse LMS, Borges KBG, de Castro RLV, Coura-Vital W, Carvalho M, Das G, A new index to discriminate between iron deficiency anaemia and thalassaemia traitRevista Brasileira de Hematologia e Hemoterapia 2016 38(3):214-19.10.1016/j.bjhh.2016.05.01127521859 [Google Scholar] [CrossRef] [PubMed]
[32]. Ferrara M, Capozzi L, Russo R, Bertocco F, Ferrara D, Reliability of red blood cell indices and formulas to discriminate between β thalassaemia trait and iron deficiency in childrenHematology 2010 15(2):112-15.10.1179/102453310X1258334701009820423571 [Google Scholar] [CrossRef] [PubMed]
[33]. Nalbantoğlu B, Güzel S, Büyükyalçın V, Donma MM, Güzel EÇ, Nalbantoğlu A, Indices used in differentiation of thalassaemia trait from iron deficiency anaemia in paediatric population: Are they reliable?Paediatric Hematology and Oncology 2012 29(5):472-78.10.3109/08880018.2012.70523022866672 [Google Scholar] [CrossRef] [PubMed]
[34]. Ehsani MA, Shahgholi E, Rahiminejad MS, Seighali F, Rashidi A, A new index for discrimination between iron deficiency anaemia and beta-thalassaemia minor: Results in 284 patientsPakistan Journal of Biological Sciences 2009 12(5):473-75.10.3923/pjbs.2009.473.47519579993 [Google Scholar] [CrossRef] [PubMed]
[35]. Niazi M, Tahir M, Raziq F e, Hameed A, Usefulness of redcell indices in differentiating microcytic hypochromic anaemiasGomal Journal of Medical Sciences [Internet] 2010 Dec 31 [cited 2020 Aug 12] 8(2)Available from: http://www.gjms.com.pk/ojs24/index.php/gjms/article/view/242 [Google Scholar]
[36]. Huang TC, Wu YY, Chen YG, Lai SW, Wu SC, Ye RH, Discrimination index of microcytic anaemia in young soldiers: A single institutional analysis. Kim J, editorPLoS ONE 2015 10(2):e011406110.1371/journal.pone.011406125679510 [Google Scholar] [CrossRef] [PubMed]
[37]. Kumar A, Saha D, Kini J, Murali N, Chakraborti S, Adiga D, The role of discriminant functions in screening beta thalassaemia trait and iron deficiency anaemia among laboratory samplesJ Lab Physicians 2017 9(03):195-201.10.4103/0974-2727.20825628706390 [Google Scholar] [CrossRef] [PubMed]
[38]. Gupta P, Nag BP, Mathur A, Evaluation of red cell indices and discriminant functions in the detection of beta thalassaemia traitIAIM 2019 6(3):50-59. [Google Scholar]
[39]. Pessar SA, Evaluation of twenty four discriminant indices for differentiating beta-thalassaemia trait from iron deficiency anaemia in EgyptiansIranian Journal of Paediatric Hematology & Oncology 2019 9(3):135-46. [Google Scholar]
[40]. Hafeez Kandhro A, Shoombuatong W, Prachayasittikul V, Nuchnoi P, New bioinformatics-based discrimination formulas for differentiation of thalassaemia traits from iron deficiency anaemiaLaboratory Medicine 2017 48(3):230-37.10.1093/labmed/lmx02928934514 [Google Scholar] [CrossRef] [PubMed]
[41]. Tong L, Kauer J, Wachsmann-Hogiu S, Chu K, Dou H, Smith ZJ, A new red cell index and portable RBC analyser for screening of iron deficiency and Thalassaemia minor in a Chinese populationSci Rep 2017 7(1):1051010.1038/s41598-017-11144-w28874768 [Google Scholar] [CrossRef] [PubMed]
[42]. Zaghloul A, Al-bukhari TAMA, Bajuaifer N, Shalaby M, AL-Pakistani HA, Halawani SH, Introduction of new formulas and evaluation of the previous red blood cell indices and formulas in the differentiation between beta thalassaemia trait and iron deficiency anaemia in the Makkah regionHematology 2016 21(6):351-58.10.1080/10245332.2015.113375326907523 [Google Scholar] [CrossRef] [PubMed]
[43]. Bordbar E, Taghipour M, Zucconi BE, Reliability of different RBC indices and formulas in discriminating between β-thalassaemia minor and other microcytic hypochromic casesMediterr J Hematol Infect Dis 2015 7(1):e201502210.4084/mjhid.2015.02225745549 [Google Scholar] [CrossRef] [PubMed]
[44]. Mukhopadhyay D, Saha K, Sengupta M, Mitra S, Datta C, Mitra PK, Role of discrimination indices in screening of beta-thalassaemia trait in West Bengal, India: An institutional experience on 10,407 subjectsSaudi Journal for Health Sciences 2015 4(3):151 [Google Scholar]
[45]. Garg S, Srivastava A, Singh S, Jaiswal R, Singh YK, Role of hematological indices in the screening of β-Thalassaemia minor (Trait) and iron deficiency anaemiaAmerican Research Journal of Hematology 2016 1(1):01-05. [Google Scholar]
[46]. Sahli CA, Bibi A, Ouali F, Fredj SH, Dakhlaoui B, Othmani R, Red cell indices: Differentiation between β-thalassaemia trait and iron deficiency anaemia and application to sickle-cell disease and sickle-cell thalassaemiaClinical Chemistry and Laboratory Medicine (CCLM) 2013 51(11):2115-24.10.1515/cclm-2013-035423800659 [Google Scholar] [CrossRef] [PubMed]
[47]. AlFadhli SM, Al-Awadhi AM, AlKhaldi D, Validity assessment of nine discriminant functions used for the differentiation between iron deficiency anaemia and thalassaemia minorJournal of Tropical Paediatrics 2006 53(2):93-97.10.1093/tropej/fml07017166936 [Google Scholar] [CrossRef] [PubMed]
[48]. Brancaleoni V, Pierro ED, Motta I, Cappellini MD, Laboratory diagnosis of thalassaemiaInternational Journal of Laboratory Hematology 2016 38(S1):32-40.10.1111/ijlh.1252727183541 [Google Scholar] [CrossRef] [PubMed]
[49]. Susanti AI, Sahiratmadja E, Winarno G, Sugianli AK, Susanto H, Panigoro R, Low hemoglobin among pregnant women in midwives practice of primary health care, Jatinangor, Indonesia: Iron deficiency anaemia or β-thalassaemia trait?Anaemia 2017 2017:693564810.1155/2017/693564828634546 [Google Scholar] [CrossRef] [PubMed]