Focal hepatic lesions constitute a daily challenge in the clinical setting. Accurate detection and characterization of liver lesions is paramount for appropriate treatment in a wide variety of clinical settings. Focal liver disease is a common diagnostic problem referred to radiologists for evaluation owing to its non-specific clinical presentation and marked inter-observer variation on clinical examination. Focal hepatic lesions include a large gamut of both benign and malignant lesions such as hepatic cysts, liver abscesses, hemangioma, adenoma, focal nodular hyperplasia, hepatocellular carcinoma, hepatoblastoma, metastases etc. Modern operative techniques and local therapies such as Radiofrequency (RF) ablation are effective methods to treat liver metastases or primary hepatic malignancies. Therefore, the determination of liver lesion count, and the nature of the lesion are important.
The optimal imaging modality for the detection of focal liver lesions has been robustly debated over the past two decades. Imaging modalities currently available to specifically evaluate focal liver disease include transabdominal and intraoperative ultrasound, triphasic Computed Tomography (CT), Computed Tomographic Arterial Portography (CTAP), and MRI enhanced with one or more types of contrast agent. These are often complementary and various combinations may be appropriate in different clinical settings. However, non-invasive methods can be useful in the detection and characterization of these lesions, usually achieved with contrast material-enhanced computed tomography and Magnetic Resonance (MR) imaging. Dynamic three dimensional gradient-recalled echoes MR imaging is a widely available non-invasive method of complete liver evaluation which provides dynamic contrast-enhanced thin-section images with fat saturation and a high signal-to-noise ratio. This is due to the high intrinsic soft-tissue contrast, improved biochemical and anatomic information, sensitivity to perfusion differences, multiplanar capability, and lack of ionizing radiation that MRI has surpassed all other liver imaging modalities [1]. It is the most sensitive and specific modality to show the focal liver lesions in a normal liver [1,2]. Its high intrinsic contrast allows the detection of small lesions, while the characteristics of the signal intensity on T1- and T2-weighted images allows the characterization of each lesion, with very high specificity in differentiating benign from malignant lesions.
More recently, the use of specific contrast agents has allowed an improvement in the identification of focal lesions. Moreover, the faster MRI scanning techniques presently available permit the dynamic assessment of contrast enhancement, which permits improved characterization of focal hepatic lesions, including regenerative nodules, dysplastic nodules, and hepatocellular carcinoma (HCC). Correct identification of benign lesions (e.g., hemangioma) will prevent unnecessary invasive procedures. Detection, characterization, enumeration, and localisation of primary or metastatic hepatic neoplasms is critical for planning appropriate therapy. During initial staging, after treatment, and during follow-up, the status of the liver helps to predict patient outcome with many neoplasms, even those treated with only radiation or chemotherapy. Specific interventions rely on imaging for planning or guidance including cryoablation, laser photocoagulation, radiofrequency/microwave ablation, percutaneous ethanol injection, surgical resection, and transplantation [3] In general, magnetic resonance imaging (MRI) has become the modality of choice for the characterization of focal liver disease.
Dynamic gadolinium-enhanced magnetic resonance imaging, as part of a comprehensive liver MRI protocol, has emerged as an important tool for liver lesion detection and characterization, providing accurate diagnostic information without the use of ionizing radiation.
The use of three-dimensional (3D) gradient-recalled-echo (GRE) sequences such as volumetric interpolated breath-hold examination (VIBE) has improved MR imaging by providing dynamic contrast material-enhanced thin-section images with fat saturation and a high signal-to-noise ratio [4]. Contrast-enhanced 3D GRE MR imaging demonstrates characteristic enhancement patterns that can be helpful in the diagnosis of various focal hepatic lesions. These enhancement patterns are seen during specific phases of imaging and include arterial phase enhancement, delayed phase enhancement, peripheral washout, ring enhancement, nodule-within-a-nodule enhancement, true central scar, pseudo central scar, and pseudocapsule. Magnetic resonance (MR) imaging findings of focal liver lesions depend on their histological and cytological features. Careful assessment of the enhancement properties of dynamic images obtained before and after administration of Intravenous Contrast Material (IVCM) is valuable in the characterization of the mass [5]. Familiarity with these enhancement patterns can help in the identification of specific focal lesions of the liver.
Hence, the aim of the present study was evaluation of MRI features of Focal liver lesions and their correlation with histopathology features for confirmation of diagnosis in the patients.
Materials and Methods
This was a multicenteric study conducted on In patients and Out patients of Sri Siddhartha Institute of Medical Sciences Hospital and Research Center and Rajarajeshwari Medical College Hospital and Research Center of Bengaluru from January 2020 to August 2020.
Inclusion Criteria: Both out patients and in patients of both tertiary centres with focal liver lesions diagnosed by Ultrasonography were included in the study after obtaining proper informed consent.
Exclusion Criteria: Patients with general contraindications for MRI, patients with renal failure (GFR<30%) and those patients not willing to give the written consent were excluded from the study.
A total sample of forty-two patients was selected for the present study were in the age group of 15 to 84 years with a mean age of 48 years [Table/Fig-1].
Age distribution of the patients.
| Age group | Number of patients |
|---|
| 1 to 20 years | 2 (4.8%) |
| 21 to 40 years | 10 (23.8%) |
| 41 to 60 years | 23 (54.7%) |
| >60 years | 7 (16.7%) |
Clinical features, laboratory tests findings and histopathological findings of the patients were noted for correlation. MRI was done for all the patients.
MRI technique: The studies were performed on the GE SIGNA 1.5 TESLA MR PLATFORM. A 4 channel phased array TORSO coil was used. Plain and contrast study were done with slice thickness of 7 mm. Plain study was done with using spin echo technique. T1 and T2 sequences were obtained in axial and coronal planes. IN PHASE and OUT OF PHASE imaging was done wherever required. Dynamic contrast enhanced MRI was done in axial and coronal planes with fat suppression techniques. It was performed after rapid bolus injection (0.1 mmol/kg body weight) of gadolinium dimeglumine (Gd-BOPTA, MultiHance). Three dynamics were taken including three minutes equilibrium phase.
Data Collection and Analysis
Pathological report was noted for correlation and comparison, hence confirmatory for the diagnosis and post-operative histopathological findings of the patients who were operated surgically for liver lesions were noted. The patients who were inoperable or not operated, their FNAC or Trucut biopsy findings were noted. Standard proformas were used for individual case for record of data.
Statistical Analysis
Microsoft Excel Software was used to analyse the data. Charts and tables were prepared for representation and comparison of data and sensitivity and specificity for diagnostic accuracy of MRI were calculated as per following formulas:
Results
Total 42 pateints of varying age group, with 25 males and 17 female patients with male predominance were included in this study. All patients were referred for MRI with a diagnosis of focal liver lesion on ultrasound. Most common lesions in age group of less than 40 years were benign like hemangiomas, hepatic adenomas and hydatid cyst in two patients each. Hepatocellular Carcinoma(HCC) was seen in only one patient in this age group with age of 35 years. Most common lesions in age group of more than 40 years were malignant like HCC, metastasis in eight patients each. Malignant lesions were common in males like hepatocellular carcinoma, metastasis followed by benign lesions like hemangioma and abscess. Most common lesions in females were benign like hemangiomas, hepatic adenoma and hydatid cyst.
One case of hepatoblastoma, cholangiocarcinoma and two cases of Carcinoma Gall Bladder (CA GB) infiltrating liver were seen in females. Metastasis was seen only in two patients. In the present study, no female patient had HCC.
Among 42 patients, 14 (33.3%) had benign lesions, 22 (52%) had malignant lesions, 5 (11%) had infective lesions and 1 (2%) had a pseudolesion [Table/Fig-2]. The most common benign lesion was hemangioma in six patients, most common infective lesion were abscess and hydatid cyst in two patients each and most common malignant lesion was HCC in nine patients.
Broad classification in lesions.
| Nature of lesion | Number of patients | Number of lesions |
|---|
| Benign | 14 | 25 excluding 1 patient with multiple regenerating nodules |
| Malignant | 22 | 30 |
| Infective | 5 | 4 excluding one patient with multiple tuberculomas |
| Pseudolesion | 1 | 1 |
Most common lobe involved in patients is right lobe in 27 (64%) patients followed by involvement of both lobes in 11 (26%) patients and left lobe in 4 (9%) patients.
Malignant Lesions
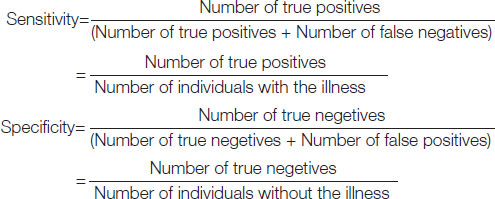
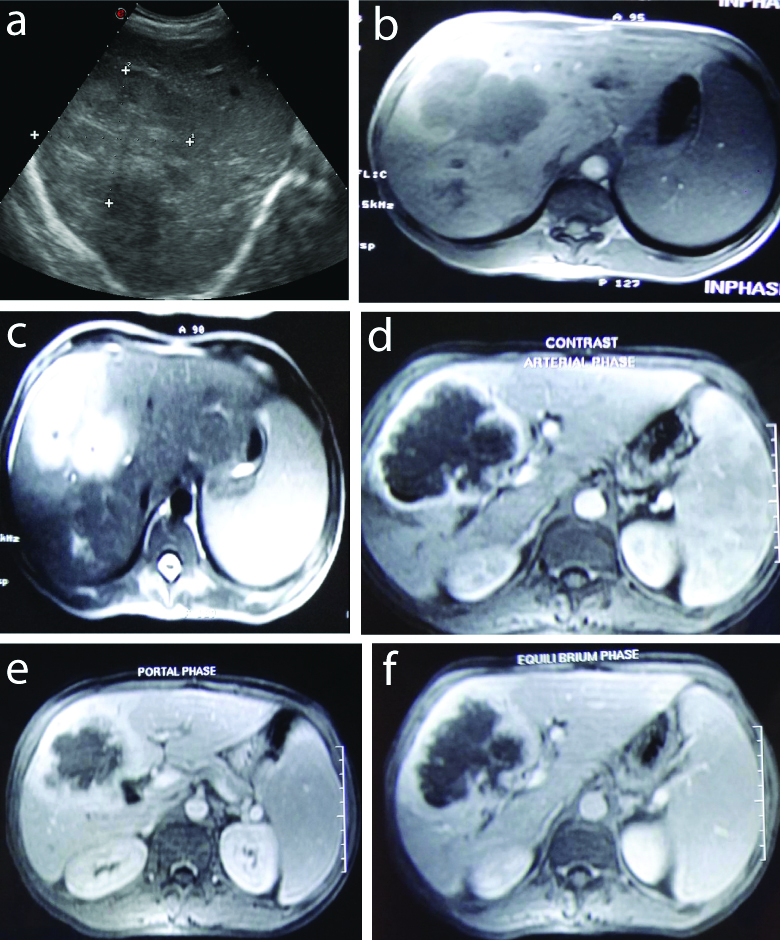
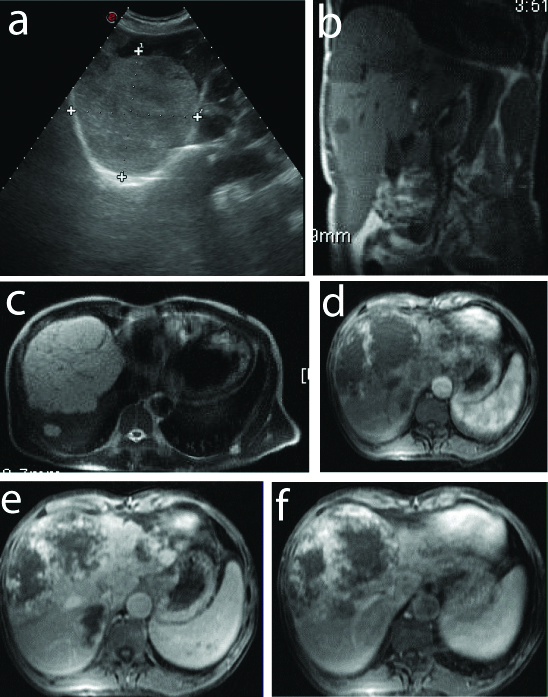
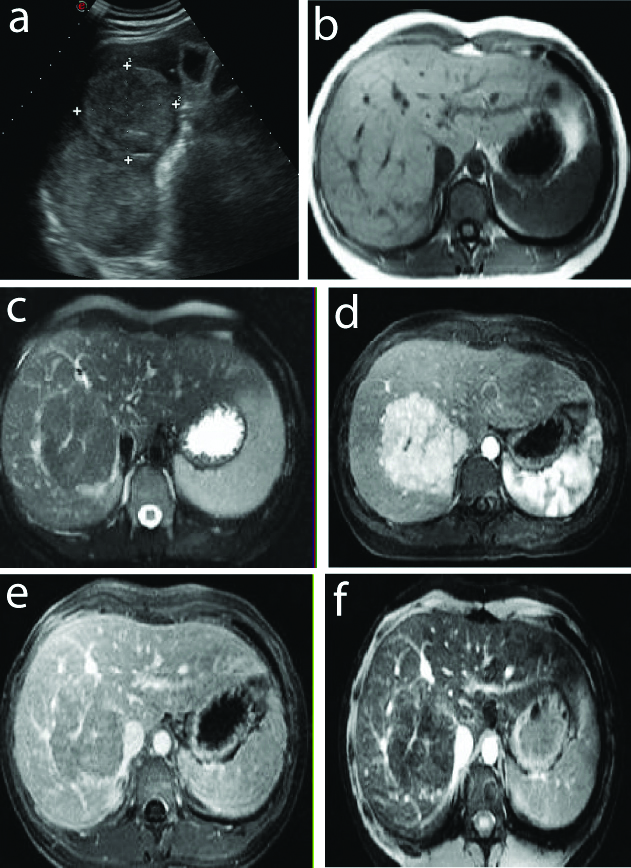
Hepatocellular carcinoma (HCC): This study involved nine patients of Hepatocellular carcinoma and all were seen in males. All the lesions were solitary in nature. Seven lesions were in right lobe, two were in left lobe, all were heterogeneously hypoechoiec on ultrasound and seven lesions (78 %) were hypointense on T1 [Table/Fig-3].
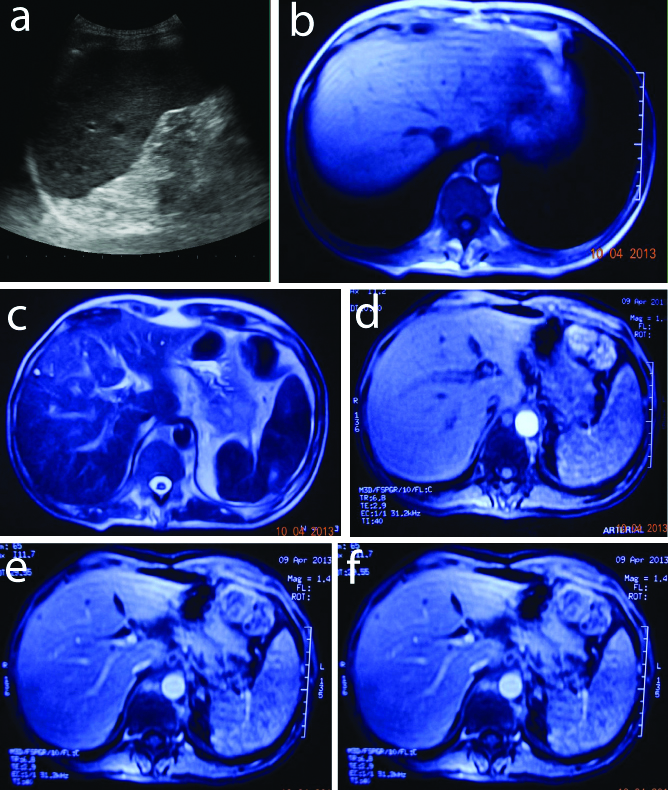
HCC with capsule in a 61-year-old male: a) USG- Hypoechoic hyperechoic rim; b) T1- Hypointense with hyperintense rim (seg IV); c) T2- Hyperintense with isoechoiec rim; d) Arterial- Mild enhancement with capsule; e) Portal- Washout with enhancing capsule; f) Equilibrium- Enhancing capsule.
Two lesions (22%) were heterogeneously hyperintense on T1 due to haemorrhage in the lesions while all the lesions were heterogeneously hyperintense on T2 weighted images.
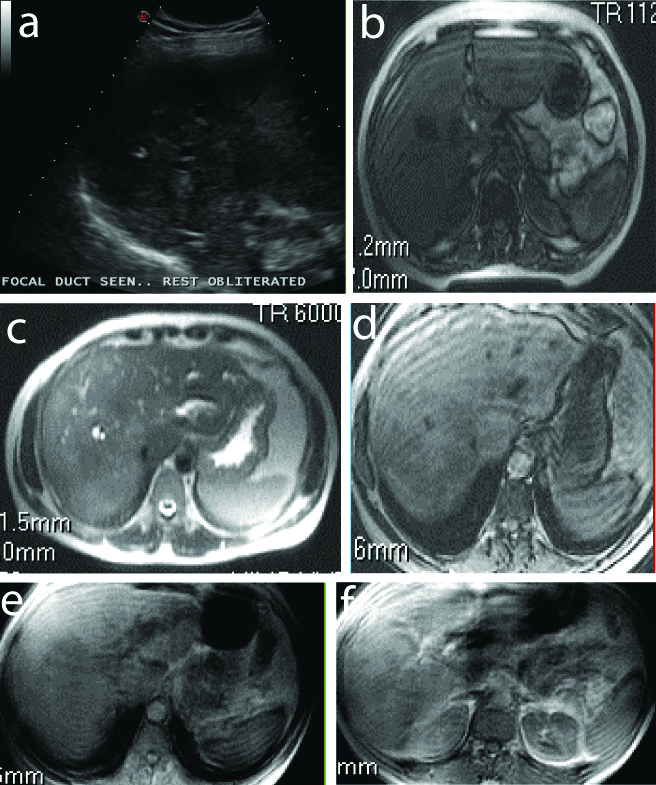
One lesion showed persistant heterogenous enhancement in all phase with enhancing septae and no washout in portal or equilibrium phase. This lesion was characterised as Metastasis on MRI which turned out to be a Hypovascular hepatocellular carcinoma [Table/Fig-4].
Hypovascular HCC in a 56-year-old male: a) USG- Cirrhotic liver Hypoechoic lesion; b) T1- Hypointense (segment V); c) T2- Heterogenously hyperintense; d) Arterial- Mild enhancement; e) Portal- Persistant enhancement; f) Equlibrium- Persistant.
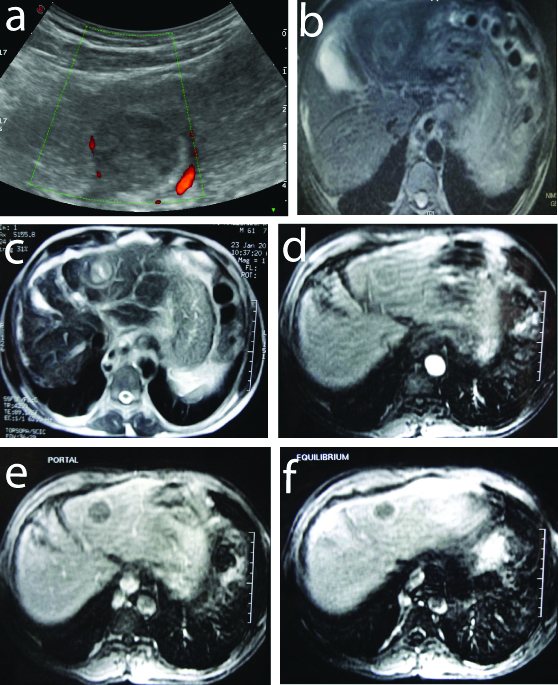
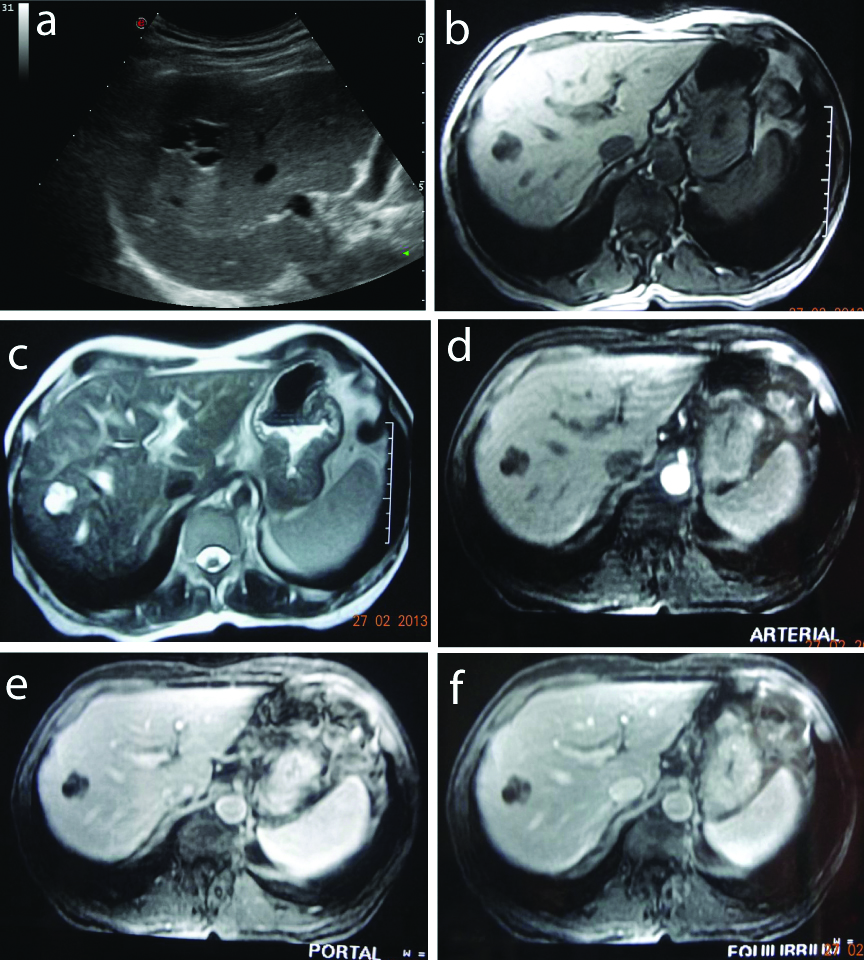
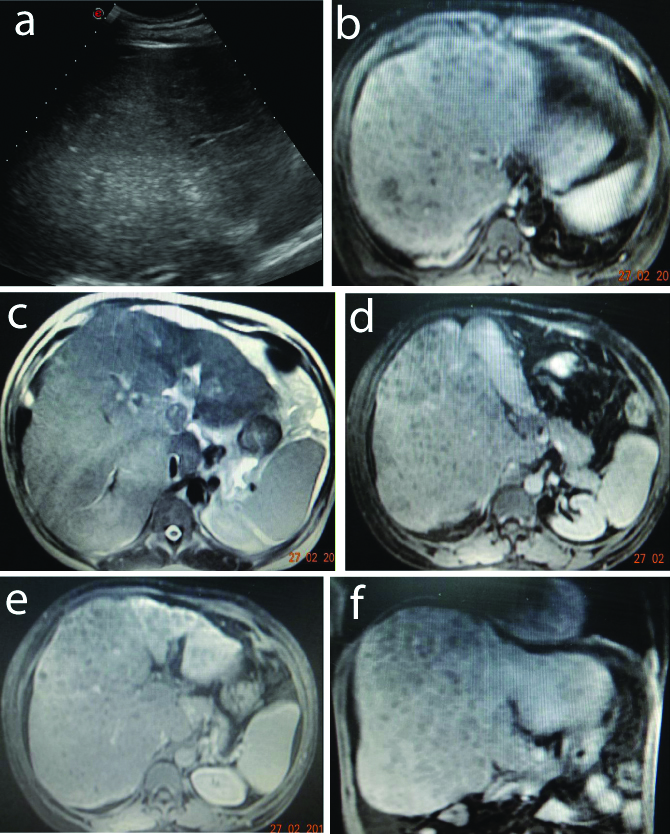
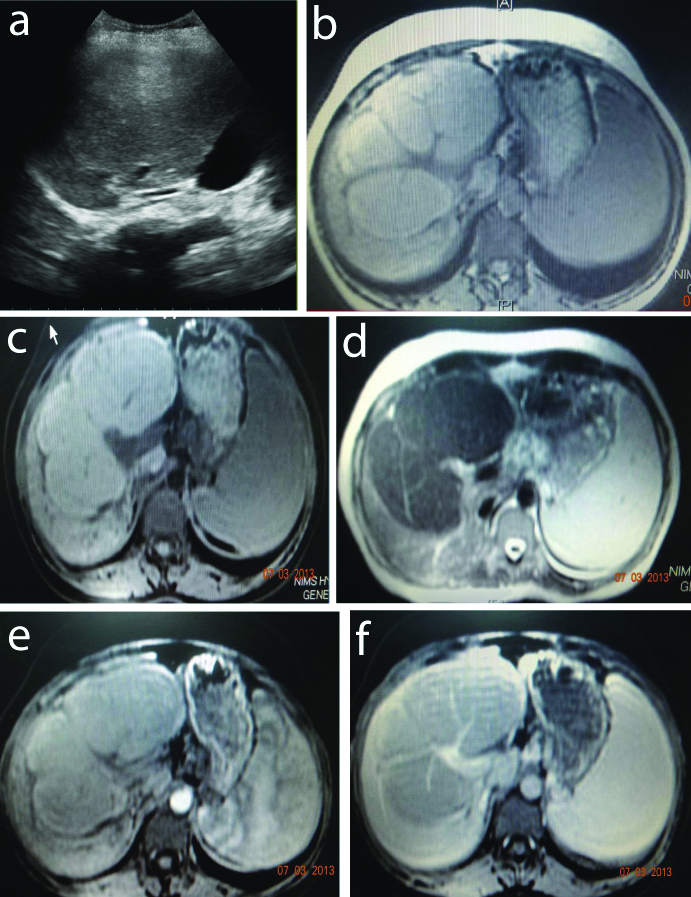
Metastasis: This study included eight patients(total 18 lesions) of metastasis, all in the age group of 40-60 years. There were known primary malignancies in the five patients as hepatocellular carcinoma, carcinoma rectum, jejunal malignancy, carcinoma pancreas [Table/Fig-5] and GastroIntestinal Stromal Tumor (GIST) involving the duodenum. All the lesions were hypoechoiec on ultrasound. Fifteen lesions out of 16 were hypointense on T1.
Metastasis from CA pancreas in a 60-year-old female: a) USG- Hypoechoic (Target lesion); b) T1- Hypointense with irregular rim (seg VI); c) T2- Hyperintense; d) Arterial- mildly enhancing mass in the head of pancreas; e) Portal- (metastasis) Peripheral irregular enhancement; Equilibrium- (metastasis) Peripheral irregular enhancement.
One lesion showed mild heterogenous enhancement with washout in portal and equilibrium phase. lesion was charesterised as Hepatocellular carcinoma which turned out to be metastasis from unknown primary [Table/Fig-6].
Metastasis from an unknown primary in a 47-year-old male): a) USG- Ill defined hypoecho; b) T1- Hypointense (segment V, VI); c) T2- Hyperintense; d) Arterial- Peripheral irregular enhancement; e) Portal- Peripheral thick enhancement; f) quilibrium- Peripheral ehancement
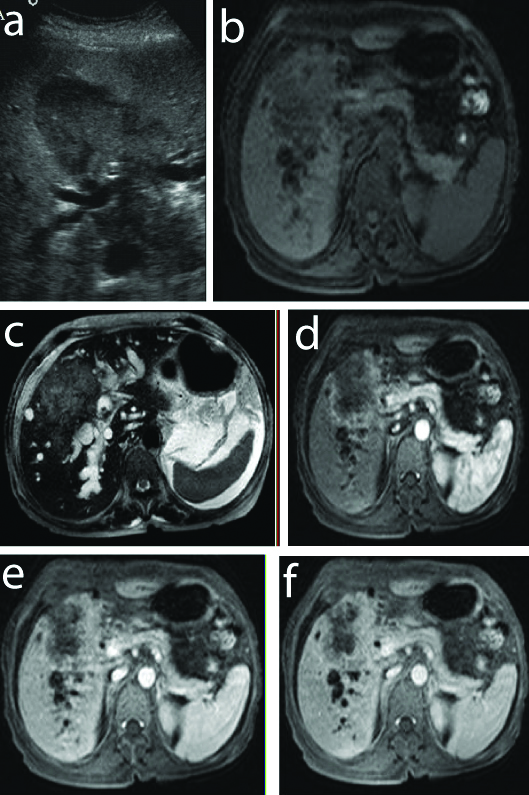
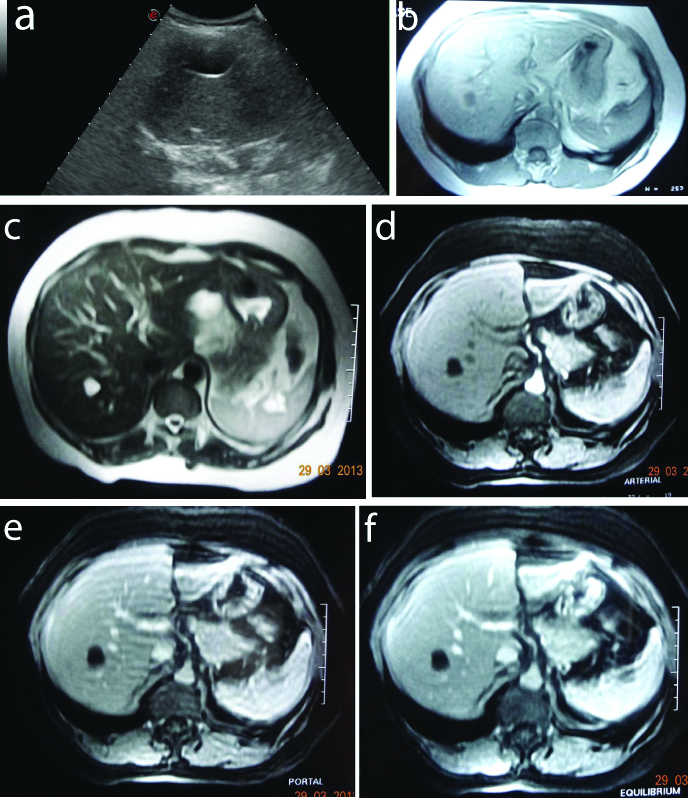
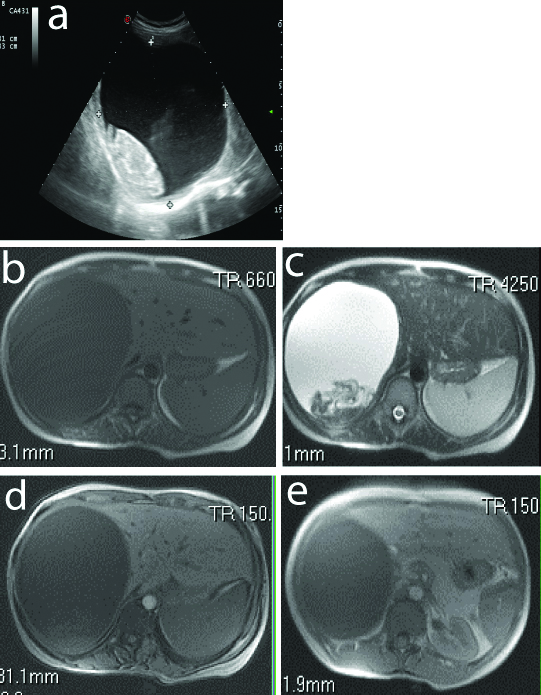
Epitheloid hemangioendothelioma: Epitheloid hemangioendo thelioma was not characterised due to similar imaging features of cholangiocarcinoma. Lesion showed T1, T2 heterogenous intensity with mild peripheral patchy enhancement and slow delayed heterogenous enhancement of lesion and presence of biliary dilatation [Table/Fig-7].
Epitheloid haemangioendothelioma in 30-year-old male: a) USG- Iso to hypechoic with no mass effect; b) T1-Iso to hypointense with mild biliary dilatation; c) T2- Mildly hyperintense; d) Arterial- Minimal heterogenous enhancement, e) Portal- Heterogenous enhancement; f) Equilibrium- Delayed mild central enhancement.
Cholangiocarcinoma: One lesion of cholangiocarcinoma was accurately characterised. Early peripheral Post contrast enhancement with progressive centripetal enhancement was seen [Table/Fig-8].
Intrahepatic Cholangiocarcinoma in a 62-year-old female: a) USG- Hypoechoic lesion with biliary dilatation; b) T1- Heterogenously Hypointense (seg IV, V); c) T2- Heterogenously hyperintense lesion with biliary dilatation; d) Arterial- Heterogenous enhancement, e) Portal- Heterogenous peripheral enhancement; f) Equilibrium- Delayed filling.
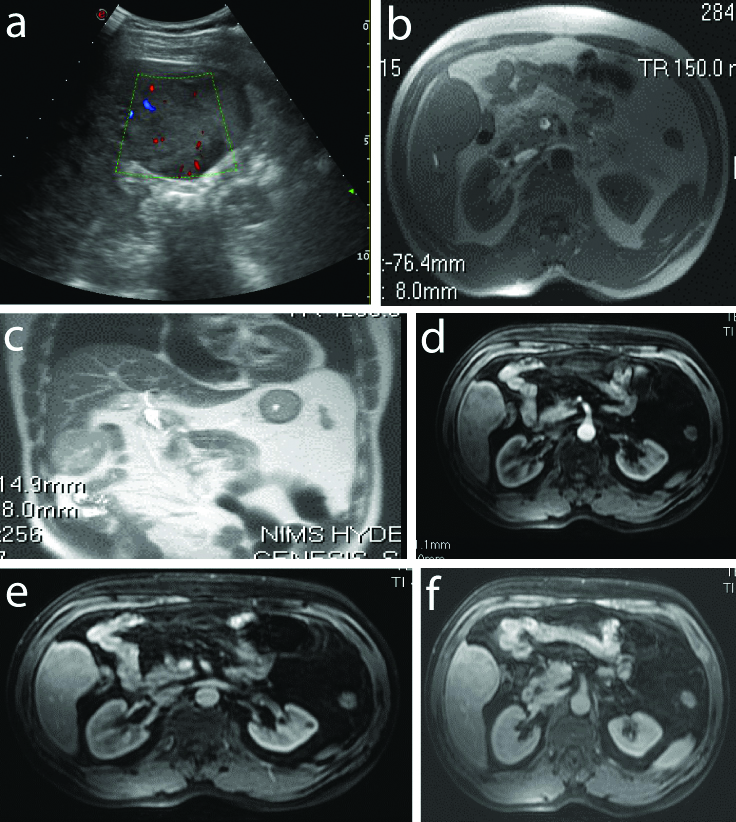
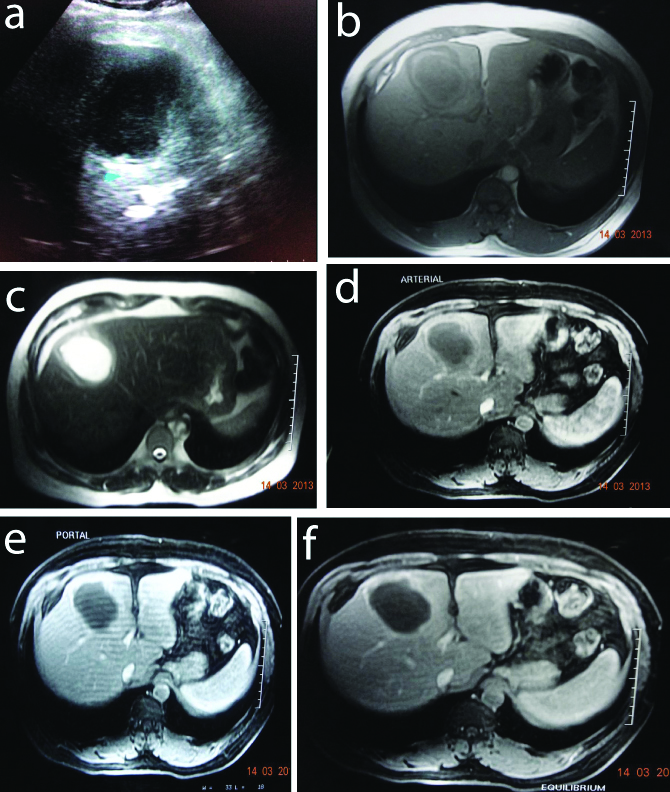
Hepatoblastoma: One lesion of Hepatoblastoma was not characterised due to the imaging features similar to Giant hemangioma. The lesion showed hetrogenous mixed intensity on T1 and T2 with patchy enhancement in arterial phase and progressive filling in portal and equilibrium phase [Table/Fig-9].
Hepatoblastoma in a 25-year-old female: a) USG- Mixed echogenic lesion; b) T1- Heterogenously Hypointense; c) T2- Heterogenously hyperintense; d) Arterial- Heterogenous peripheral enhancement; e) Portal- Increase in enhancement; f) Equilibrium- Heterogenous central filling
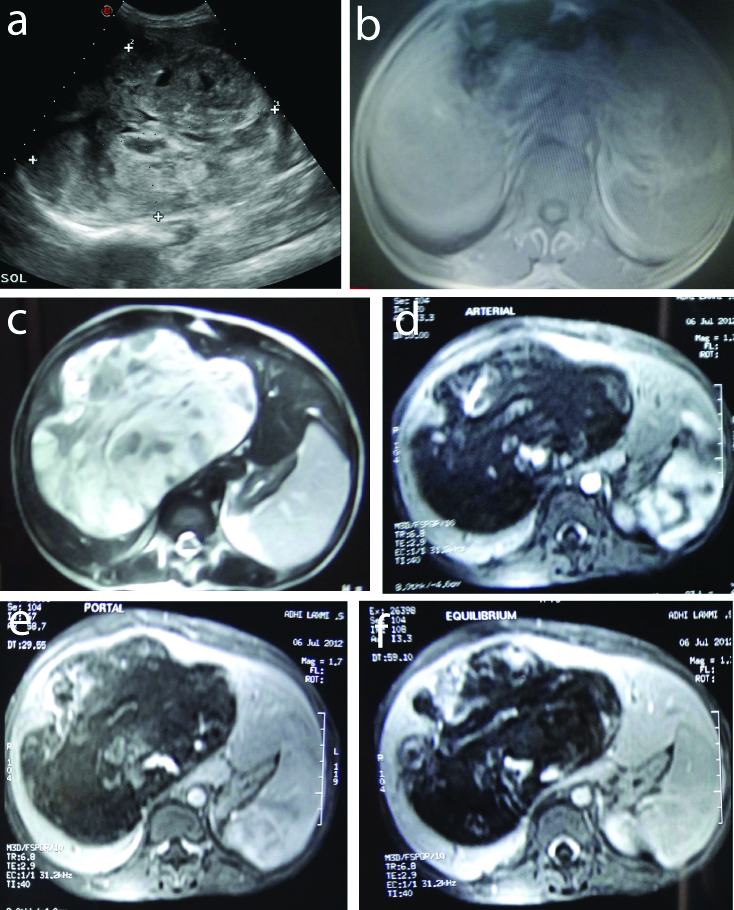
Carcinoma (CA) Gall Bladder (GB) with infiltration of liver: Two lesions of Carcinoma Gall bladder with liver infiltration were characterised by MR features of heterogenous intensity mass in GB fossa infiltrating the liver with non-visualised GB. Lesions showed progressive enhancement which differentiated from HCC.
Benign Lesions
Hemangioma: The study included six patients with hemangiomas and sixteen lesions were studied in them. Among five lesions of giant hemangioma, four lesions were heterogeneously hyperechoiec on ultrasound and one lesion was heterogeneously hypoechoic. Rest all the small hemangiomas, were hyperechoiec on ultrasound. All the lesions were Hypointense on T1 weighted images. All the lesions showed typical peripheral nodular enhancement and progressive centripetal filling [Table/Fig-10].
Giant Hemangioma in a 53-year-old female: a) USG-Hyperechoic; b) T1- (coronal image) Hypointense (segment VI, VII, VIII); c) T2- Hyperintense (bright); d) Arterial- Peripheral discrete enhancement; e) Portal- Progressive filling of center; f) Equilibrium- Centripetal filling.
Cyst: Two lesions of complex cysts [Table/Fig-11] and three lesions of simple cysts were accurately characterised [Table/Fig-12]. Characteristic feature being homogenous T2 hyperintensity and no enhancement. Complex cysts had septations within.
Complex cyst in a 70-year-old female: a) USG- Anechoic with spetations; b) T1- Hypointense with septations (seg VI); c) T2- Hyperintense with septations; d) Arterial- No enhancement; e) Portal- No enhancement; f) Equilibrium- No enhancement.
Simple Cyst in a 15-year-old female: a) USG- Anechoic; b) T1- Hypointense (segment VI); c) T2- Hyperintense; d) Arterial- No enhancement; e) Portal- No enhancement; f) Equilibrium- no enhancement.
Hepatic adenoma: The study included two patients with hepatic adenomas and both were females in the age group of 20-40 years, total of three lesions with average size of the lesions being 5.3 cms. These patients with imaging features of well-defined homogenous lesion with fat component within, showing signal drop in OUT OF PHASE images and mild enhancement on arterial phase with washout in subsequent phases were accurately characterised as hepatic adenoma [Table/Fig-13].
Hepatic Adenoma in a 29-year-old female: a) USG- Mildly hyperechoic; b) T1 IN PHASE- Isointense (Seg VI); c) T1 OUT OF PHASE- Hypointense; d) T2- Iso to hyperintense; e) Arterial- Mild enhancement; f) Equilibrium- Mild washout.
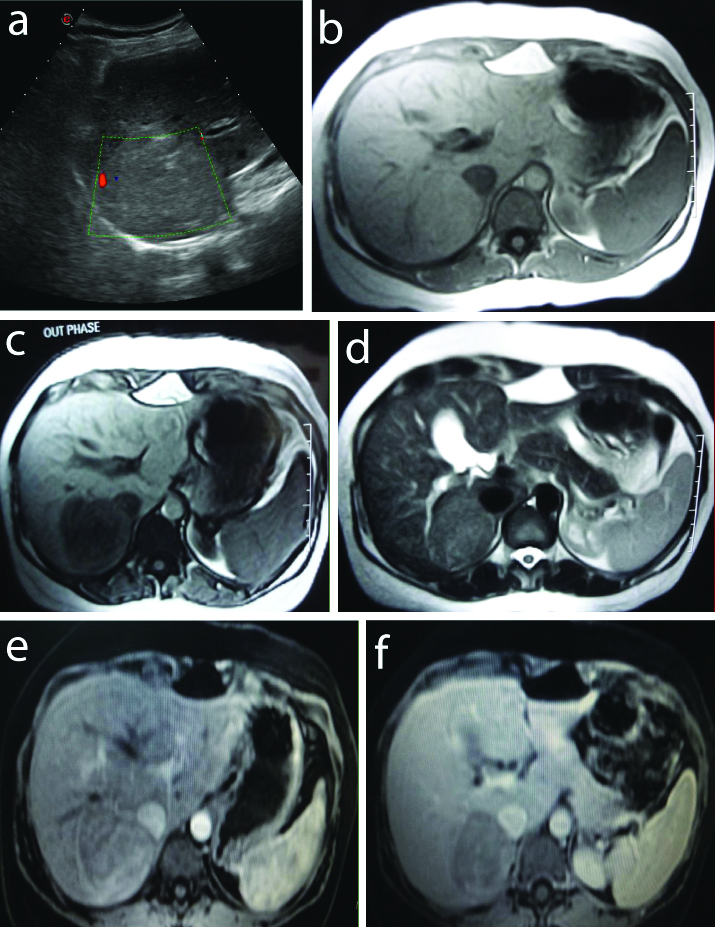
Focal nodular hyperplasia (FNH): One lesion of FNH was accurately characterised with distinct feature of homogeneity, central scar which was hyperintense on T2W images which showed delayed enhancement [Table/Fig-14].
Focal nodular hyperplasia in a 42-year-old female: a) USG- Heterogenously hyperechoiec; b) T1- Isointense (seg V, VI); c) T2- Isointense with hyperintense scar; d) Arterial- Intense enhancement with non enhancing scar; e) Portal- Mild Washout with enhancing scar; f) Equilibrium- Enahancing scar.
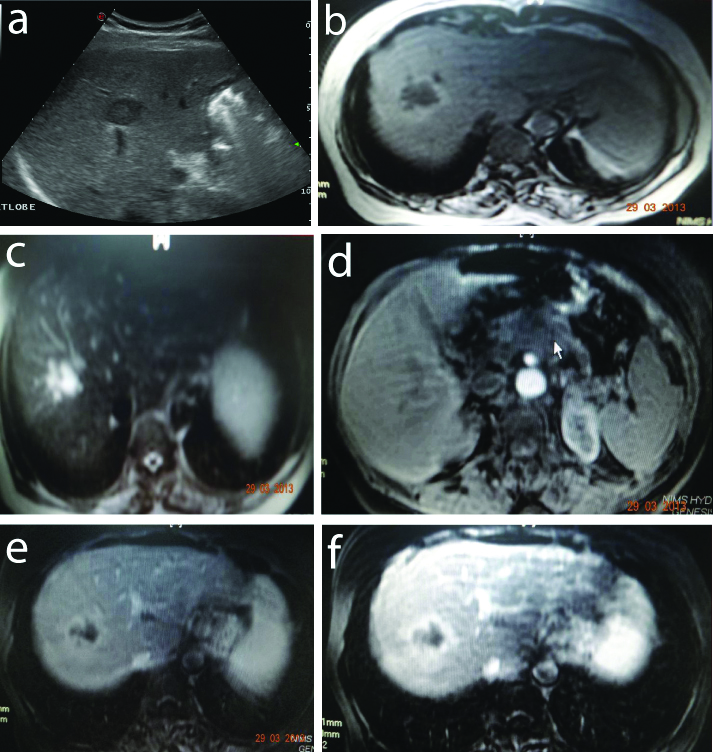
Regenerating nodules: The study included one patient with multiple regenerating nodules in background of cirrhotic liver. Patient had mildly shrunken liver with surface irregularity and nodularity with presence of ascites, presented as heterogeneously hypoechoiec on ultrasound. All of them were hypointense on T1 and T2 weighted images with no post-contrast enhancement [Table/Fig-15].
Regenerating nodules in 56-year-old male with liver cirrhosis: a) USG: Cirrhosis with multiple hypoechoic lesions; b) T1- Multiple hypointense; c) T2- Hypointense; d) T2- No enhancement; e) Portal- No enhancement; f) Equilibrium- (coronal image) no enhancement.
Hydatid cyst: Two hydatid cysts were accurately characterised. Distinct features were minimally enhancing T2 low intensity rim and one lesion with membranes within indicating rupture [Table/Fig-16].
Hydatid Cyst in a 24-year-old female: a) USG- Anechoic lesion with internal echoes, membranes and debris; b) T1- Hypointense with isointense rim; c) T2- Hyperintense with membranes within and hypointense rim; d) Arterial- No enhancement; e) Portal- minimal rim enhancement.
Abscess: Two lesions of pyogenic abscess were accurately characterised with features of hyperintensity on T2 and thick peripheral enhancement [Table/Fig-17].
Abscess in a 42-year-old male: a) USG- Hypoechoic lesion with internal echoes; b) T1- Hypointense with Iso intense wall and perilesional edema; c) T2-Hyperintense with isotense wall; d) Arterial- Thick Peripheral wall enhancement; e) Portal-Peripheral wall enhancement; f) Equilibrium- Peripheral wall enhancement.
Tuberculomas: The study included one patient with multiple tuberculomas in 49 years male involving both lobes of liver. The lesions presented with the same characterstics as other granulomas and lymphomas [Table/Fig-18].
Tuberculomas in a 44-year-old male: a) USG- Multiple hypoechoic lesions; b) T1-Multiple tiny Hypointense lesions; c) T2-Hyperintense; d) Arterial-No enhancement; e) Portal- No enhancement; f) Equilibrium- No enhancement.
Focal fatty sparing (Pseudo lesion): Focal fatty sparing was accurately characterised in one patient. Lesion had no mass effect. Loss of signal on OUT PHASE T1W images is distinct feature of fat [Table/Fig-19].
Focal fatty sparing in a 35-year-old female; a) USG- Isoechoic area; b) T1 IN PHASE- Iso to hyperintense; c) T1 OUT OF PHASE- Iso to hyperintense; d) T2- Hypointense; e) Arterial- Enhancement equal to liver; f) Equilibrium- Enhancement equal to liver.
All the findings of 42 patients of the study clinically, ultra sonographically and their correlation with MRI characterisation of the lesions have been discussed [Table/Fig-20].
Clinical, Ultrasonographic, MRI, histopathological details and their comparisons in study subjects.
| S. No. | Sex | Clinical features/Investigation | Ultrasonography | T1 IN PHASE/OUT PHASE | T2 characterstics | Arterial characterstics | Portal | Equilibrium phase | Radiological diagnosis | Final diagnosis (Histopathological confirmation) |
|---|
| 1 | M | Pain abdomen | Cirrhotic liver, heterogenously hypoechoic lesion (5,6,7,8 seg.)- 14×12 cm, capsulated, Main and rt. Br. Portal vein invasion, with haemorrhage | Heterogenously hypointense | Heterogenously hyperintense | Central part showing heterogenous enhancement | Washout | Washout | HCC | HCC |
| 2 | F | Pain abdomen | Complex cyst (4A,B seg.)- 5×5 cm | Hypointense with isointense septations | Hyperintense with septations | Non enhancing | No | No | Complex cyst | Complex cyst |
| 3 | M | CLD, portal vein thrombosis, ascites | Cirrhotic liver, two hyperechoiec lesions in seg 6 and 7, 3×2, 1.5×1.5 cm | Hypointense | Hyperintense | Minimal pheripheral nodular enhancement | Centripetal filling | Centripetal filling | Hemangiomas | Hemangiomas |
| 4 | F | Pain abdomen | Hypoechoic lesion in body of pancreas with an illdefined hypoechoic lesion in segment seven of liver, 3×2.5 cm | Hypointense | Hyperintense | Peripheral enhancement | Increase in enhance | Persistant | CA pancreas with liver metastasis | Metastasis |
| 5 | M | k/c/o ca rectum, SOL in liver | Cystic lesions in segment 2,7- 3×2.5 cm, 1.5×1 cm | Hypointense | Hyperintense | Non-enhancing | No | No | Complex cyst | Complex cyst |
| 6 | M | k/c/0 alcoholic cirrhosis, Ascites, splenomegaly present | Cirhosis with multiple heterogenous echotexture lesions in all seg. in both lobes- 0.5 to 2 cm | Hypointense | Hypointense | Non-enhancing | No enhancement | No enhancement | Regenerating nodules | Regenerating nodules |
| 7 | M | CLD, portal vein thrombus | Cirrhosis with a heterogenously hypoehoiec lesion in segment 6 in right lobe- 3.5×3 cm | Hypointense | Heterogenously hyperintense | Minimal enhancement | Minimal enhancement | Washout | HCC | HCC |
| 8 | M | Pain abdomen | Hypoechoiec lesion in segment 2, 4.6×3.6 cm | Hypointense | Hyperintense with few thick septations within | minimal pheripheral and septations enhancement | Persistant | Persistant | Small bowel malignancy with liver metastasis | Metastasis |
| 9 | M | Fever, pain abdomen | Cystic lesion with internal echoes and thick wall- 6×5 cm, Capsulated | Hypointense with hyperintense rim | hyerintense with isointense rim | Mild enhancement of rim | Persistant | Persistant | Ruptured abscess | Abscess |
| 10 | M | k/c/o CLD with hep C positive, splenomegaly, Retroperitoneal nodes | Cirrhosis with mixed echoiec lesion, 5×4 cm, with Haemorrhage | Heterogenously hyperintense | Heterogenously hyperintense | Mild peripheral enhancement with enhancing septae | Persistant | Persistant | HCC | HCC |
| 11 | F | Pain abdomen | Large hypoechiec lesion in entire rt. Lobe- 14×11 cm, with Haemorrhage | Hypointense with few hyperintensities | Hyperintense with few hypointense areas within | Mild periphral discrete nodular enhancement | Peripheral puddling with centripetal filling | Peripheral puddling with centripetal filling | Giant hemangioma | Hepatoblastoma |
| 12 | M | k/c/o ca rectum, sol in liver | Hypoechoiec lesion in seg. 2 and 7- 2×1.5 cm, with Haemorrhage | Hypointense with hyperintense focus within | Hypointense with hyperintense rim | Heterogenous central enhancement | Persistant | Persistant enhancement | Metastasis | Metastasis |
| 13 | F | Pain abdomen | Heterogenously hyperechoiec lesions both lobes- 16×15 cm in lt. lobe, multiple small in rt. Lobe, compressing lt. Hepatic vein | Hypointense | Hyperintense | Mild peripheral nodular enhancement | Increase in enhancement with centripetal filling | Persistant | Giant and multiple small hemangiomas | Hemangiomas |
| 14 | M | CLD | Heterogenously hypoechoiec lesion with hyperechoiec rim and hypoechoiec halo spec of calcification (4B segment)- 4×4 cm, Capsulated | Hypointense | Heterogenously hyperintense | Mild enhancement | Peripheral enhancement with central washout | Peripheral enhancement with central washout | Cirrhosis with HCC | HCC |
| 15 | F | Pain abdomen | Large cystic lesion in rt lobe with internal echoes and hyperechoic material- 13×12 cm | Hypointense | Hyperintense with hypointense serpingenous material within | Non-enhancing | Minimal rim enhancement | Minimal rim enhancement | Hydatid cyst | Hydatid cyst |
| 16 | M | Pain abdomen | Large heterogenously hyperechoiec lesion in rt lobe, 13×13 cm, exophytic | Hypointense | Hyperintense | Peripheral discontinuous enhancement | Peripheral puddling with centripetal filling | Persistant | Giant hemangioma | Hemangioma |
| 17 | M | Pain abdomen | Heterogenously hypoechoiec lesion (seg. 5, 7, 8)-10×10 cm, large central necrotic component | Hypointense | Heterogenously hyperintense with hypointense thick septations | Thick irregular heterogenous enhancement | Mild washout | Mild washout | HCC | Metastasis |
| 18 | F | Pain abdomen | Cystic lesion in right lobe, 5×2 cm, partially exophytic | Hypointense | Hyperintense | Non-enhancing | No | No | Simple cyst | Simple cyst |
| 19 | F | Pain abdomen, vomiting | Large hypoechiec lesion in rt lobe of liver and gb fossa (seg. 5,6 and 8 of liver)- 10×9 cm | Hypointense | Heterogenously hyperintense | Mild patchy enhancement predominantly peripheral | Central necrotic area and peripheral mild enhancement. | Persistant | Ca gb infiltrating segment 5,6,8 of liver | Ca gb |
| 20 | F | Pain abdomen and distension | Large heterogenously hyperechoiec lesion in both lobes- 16×15 cm in lt. lobe, multiple similar lesions in rt. lobe | Hypointense | Hyperintense | Subtle discrete peripheral enhancement | Increased with centripetal filling | Persistant filling | Giant hemangioma with multiple small in rt lobe | Multiple hemangiomas |
| 21 | M | Pain abdomen, loss of weight | Heterogenously hypoechoiec lesion in rt. Lobe- 4×3 cm, exophytic | Hypointense | Heterogenously hyperechoiec with few cystic areas | Homogenous enhancement | Persistant | Persistant | Hypovascular HCC | Hypovascular HCC |
| 22 | F | Pain abdomen | Large cystic lesion in rt lobe (seg. 6and 7) - 8×7 cm, isointense wall, exophytic displacing rt. Kidney | Hypointense | Hyperintense | No enhancement | Minimal rim enhancement | Minimal rim enhancement | Hydatid cyst | Hydatid cyst |
| 23 | M | k/c/o CA thyroid, pain abdomen | Multiple heterogenously hyperechoiec lesions in both lobes- 12×10 in seg. 8 largest | Hypointense | Heterogenously hyperintense | Peripheral discrete nodular enhancement | Centripetal filling | Persistant | Multiple hemangiomas with a giant one | Multiple hemangiomas |
| 24 | M | k/c/o hbv related liver cirrhosis, spleno-portal thrombosis, splenomegaly | Cirrhosis with large heterogenously hypoechoiec lesion in rt. Lobe (seg. 6 and 7) - 5×5 cm | Hypointense | Iso to hyperintense | Heterogenous enhancement | Washout | Washout | HCC | HCC |
| 25 | F | Pain abdomen | Cystic lesion in right lobe, 1.1×1 cm | Hypointense | Hyperintense | Non enhancing | No | No | Simple syst | Simple cyst |
| 26 | F | Pain abdomen | ill-defined hypoechoic lesion in segment 7 of liver rt. Lobe- 3 cm | Hypointense | Hyperintense | Peripheral enhancement | Increase in enhance | Persistant | Liver metastasis | Metastasis |
| 27 | M | Pain abdomen | Multiple heterogenously hypoechoiec lesions (all segments), few giving target appearance both lobes- 6×5 cm in seg 6 | Hypointense | Heterogenously hyperintense | Mild peripheral enhancement | Progressive enhancement of periphery | Persistant | Metastasis | Metastasis |
| 28 | F | Pain abdomen | Large heterogenously hypoechoiec lesion in right lobe of liver (6, 7, 8 seg.)- 10×9 cm | Hypointense | Heterogenosly hyperintense | Peripheral nodular enhancement | Gradual centripetal filling | Centripetal filling | Giant hemangioma | Hemangioma |
| 29 | F | Pain abdomen | Heterogenously hyperechoiec lesions (6 and 7 seg.)- 6×6 cm rt. Lobe, largest, Capsulated | Isointense in IN PHASE and hypointense in OUT PHASE | Iso to hyperintense | Mild patchy enhancement | Mild washout | Persistant | Hepatic adenoma | Hepatic adenoma |
| 30 | M | k/c/o hbv related liver cirrhosis, splenomegaly and mild ascites | Cirrhosis, large ill-defined heterogenous echotexture lesion in right lobe (7 and 8 seg.)- 8×7 cm, Capsulated, IVC And Rt. Portal vein invasion | Hypointense | Heterogenously hyper intense | Heterogenous patchy enhancement | Persistant | Washout | Cirrhosis with HCC | HCC |
| 31 | M | Loss of weight, appetite | Hypoechoiec lesion in segment 4a, left lobe- 3×2 cm | Hypointense | Iso to hyperintense | Heterogenous mild enhancement | Persistant | Washout | HCC | HCC |
| 32 | M | Fever, pain abdomen | Multiple tiny hyechoiec lesions in rt. Lobe (all segments)- sub cm sized lesions | Hypointense | Hyperintense | Non-enhancing | No | No | Disseminated koch’s with multiple granulomas in liver and spleen | Disseminated koch’s |
| 33 | F | Right hypochondrium pain | Large hypoechoiec lesion in gb fossa infilterating right lobe of liver (5,6 and 7 seg.)- 6×6 cm, ihbd | Hypointense | Heterogenously hyperintense | Heterogenous enhancement in right lobe | Persistant enhancement | Persistant enhancement | Ca gb infiltrating segment 5,6,7 of liver | Ca gb |
| 34 | M | Pain abdomen, loss of apetite | Heterogenous echotexture in liver with no mass effect (4, 5, 6, 7and 8 seg.)- 11×10 cm, both lobes, diffusely narrowed and irregular contour of entire right and left proximal hepatic ductal system with dilated distal branches | Hypointense | Diffusely infiltrating heterogenously hyperintense | Minimal heterogenous patchy enhancement | Progressive increase in enhancement | Increase in enhancement | Cholangiocarcinoma | Epitheloid hemangioend-othelioma |
| 35 | F | Pain abdomen | Heterogenously hypoechoiec lesion in rt. Lobe (5 and 6 seg.)- 6×6 cm | Isointense | Iso to hyperintense | Heterogenous enhancement | Mild washout | Mild washout | Hepatic adenoma | Hepatic adenoma |
| 36 | F | Pain abdomen | Isoechoic area in liver (4,5,6, and 7 seg.)- 12×11 cm both lobes, the vessels are traversing through the lesion. No mass effect | Isointense in IN PHASE and mildly hyperintense in OUT PHASE | Hypointense | Enhancement similar to liver | Epitheloid haemangio-endothelioma | Enhancement similar to liver | Large area of focal fatty sparing | Large area of focal fatty sparing |
| 37 | M | Post op c/o HCC in segment 2,3 | Hypoechoiec lesion in both lobes- 2.1×2.5 cm, largest | Hypointense | Hyperintense | Minimal heterogenous enhancement | Persistant | Persistant | Metastasis | Metastasis |
| 38 | M | Pain abdomen, loss of apetite | Large mixed intensity lesion in epigatric and left hypochondrium with hypoechoiec lesion in left lobe of liver (4b seg)- 2.5×2.5 cm, large enhancing mixed intensity mass in left hypochondrium and epigastric region | Hypointense | Heterogenously hyperintense | Peripheral rim enhancement | Persistant peripheral rim | Persistant | Gist with metastasis | Metastasis |
| 39 | M | Headache, giddiness | Small hypoechoiec lesion with thin hyperechoic rim in rt. Lobe- 2.3×2.1 cm | Hypointense | Hyperintense | Non-enhancing | Minimal rim enhancement | Persistant | Abscess | Abscess |
| 40 | M | Alchoholic, cld | Cirrhosis with heterogenously hypoechoic lesion in right lobe - 2×1 cm | Hypointense | Heterogenously hyperintense | Enhancing | Mild washout | Mild washout | Cirrhosis with HCC | HCC |
| 41 | F | Pain abdomen and icterus | Heterogenously hypoechoiec lesion with biliary dilatation in both lobes (4 and 5 seg.)- 6 cm, segmental biliary dilatation, delayed enhanced | Hyointense | Heterogenously hyperinetense | Peripheral enhancement | Peripheral enhancement | Patchy enhancement | Cholangio carcinoma | Cholangio carcinoma |
| 42 | F | Pain abdomen | Heterogenously hypoechoiec lesion in rt. Lobe (5 and 6 seg.)- 5.5 cm | Iso intense, central linear scar | Iso, central linear hyper scar | Hyper, central hypo scar | Hyper, central hypo scar | Iso, central hyper scar | FNH | FNH |
M: Male; F: Female; rt: Right; lt: Left; Br: Branch; HCC: HepatoCellular carcinoma; Seg.-: Segment; CLD: Chronic liver disease; CA: Carcinoma; k/c/o-: Known case of; SOL: Space occupying lesion; hep C: hepatitis C; gb. fossa-: Gall bladder fossa; GB: Gall bladder; hbv: Hepatitis b virus; IVC-: Inferior vena cava; post-op.: Post operative; GIST-: GastroIntestinal stromal tumor; FNH: Focal nodular hyperplasia
Magnetic Resonance Imaging (MRI)
Specificity of MRI for HCC was 96.7 % and most characteristic feature of HCC were hyperintensity on T2W images, hypervascularity on post-contrast arterial phase with early washout and presence of capsule was most characteristic finding seen in three lesions. Specificity for metastasis was 97% and most common characteristic pattern was peripheral rim enhancement. Sensitivity for hemangiomas was 100% with most specific features of T2 brilliantly bright pattern and peripheral nodular discontinuous enhancement following intensity of vessels with progressive centripetal filling of contrast [Table/Fig-21].
MRI has high specificity for characterisation of focal liver lesions (90.4%).
| Positive |
|---|
| True positive | 38 |
| False negative | 4 |
| Negative |
| False positive | 4 |
| True negative | 38 |
| Output: |
| Sensitivity | 90.48% |
| Specificity | 90.48% |
| Positive predictive value | 90.48% |
| Negative predictive value | 90.48% |
Discussion
A total of 42 patients referred with a diagnosis of focal liver lesion on ultrasound were included in the present study and underwent conventional MRI (T1, T2, DYNAMIC POST CONTRAST TRIPLE PHASE) and IN PHASE, OUT OF PHASE imaging (where ever applicable) on 1.5 Tesla MRI machine (Signa LXI, GE). Only 31 patients underwent FNA/Biopsy/surgery and histopathology proof was obtained. In remaining 11 patients, there was no histopathological examination done since lesions in all these patients showed typical characteristic features on MRI and hence no further diagnostic work-up was needed. One among them was a complex cyst seen in the right lobe was followed up for a period of one year. There is no change in the size and MR morphology. And hence no intervention was required.
Trastek VF et al., in their study concluded that Fine-needle aspiration (FNA) should be avoided if benign lesion like haemangioma remains a diagnostic possibility, MRI itself is sufficient to provide a conclusive diagnosis and thus obviate the need for a biopsy [6] Among 42 patients in present study, evaluation of 60 lesions in 40 patients was done while in the rest of two patients, one patient had multiple regenerating nodules studded in liver in background of cirrhosis and another patient had multiple tuberculomas in both lobes which were uncountable. Thirty eight patients (90.4%) were accurately characterised on MRI of 42 patients hence it could accurately characterise 56 lesions in 36 patients and two patients had multiple lesions studded in both lobes of liver (one patient with multiple regenerating nodules and another with multiple tuberculomas) which were also correctly diagnosed.
Four lesions in four patients, one lesion each of hepatocellular carcinoma, Metastasis, hepatoblastoma and epitheloid hemangio endothelioma, were not correctly diagnosed based on imaging and they were diagnosed based on histopathological examination.
Present study showed higher accuracy (90.4%) in characterising the focal liver lesions with gadolinium enhanced MRI. Compared to the study done by Huppertz A et al., [7] where the specificity is 79.8%. They could correctly diagnosed 103 of 129 patients in post-contrast imaging. The high specificity in present study was probably due to small sample size.
The study by Y. Yamashita et al., [8] could correctly diagnose 86% lesions among 300 focal liver lesions calculated by logistic progression analysis with morphological characters on T2 weighted images like tumour margin, internal architecture and enhancement characteristics. This study had comparable lesion characterisation rate to the present study (90.4%). Though we took into account the tumour margin, the findings like internal architecture (T2WI) and enhancement characters were similar and hence similar specificity.
The incidence of malignant liver lesions was only 22% (55 lesions) among 254 patients published by Jones et al., [9] and the incidence of HCC was 3 % (3 lesions), metastasis 54 % (12 lesions) and 31% (7 lesions) by Schmiedl U et al., [10]. The incidence of malignant lesions 48% (30) is higher in the present study, as compared to the above studies followed by 41% (26) benign lesions and 10% (5) infective lesions. The maximum number of malignant lesions are found in the age group of 40-60 years in this study who are more prone to develop malignant lesions.
Malignant Lesions
Hepatocellular carcinoma in cirrhotic liver: Cirrhosis is the most important predisposing factor for HCC, with approximately 80% of cases developing on a background of cirrhotic liver in a study [11]. In this study eight patients of cirrhosis with focal liver lesions were evaluated. Benign lesions like hemangioma can be seen and they should be considered as differential with specific imaging characters. Isointensity on T2-weighted images are typical features of well-differentiated tumours, while hypointensity on T1-weighted images and hyperintensity on T2-weighted images are usually associated with moderately or poorly differentiated tumors as studied by Lencioni R et al., [11]. There was only one HCC with slightly different characteristics on T2WI that was Iso to hyperintense. This lesion was of low grade malignancy on histopathological examination. In the present study, most characteristic MRI finding suggestive of HCC was early arterial enhancement with rapid washout in subsequent phases due to Arterio-venous shunting in the hypervascular HCC. This finding is well described in the literature [12] in 6 (85%) of 7 HCCs in cirrhosis. In a study by Jorge A et al., in 66 patients, arterial enhancement was present in all 66 patients with HCC in cirrhotic patients. By contrast, delayed hypointensity of the arterially enhancing mass was present in 89% of the patients with HCC with Sensitivity of 89% and Specificity of 96% for HCC.
Study by Marrero JA et al., [12] infers that HCC usually becomes hypointense in the portal venous and delayed phases and often shows a delayed enhancing outer rim of capsule. These features are highly specific for HCC, with a reported overall sensitivity of 89% and specificity of 96% for delayed hypointensity.
Hence, Dynamic contrast enhance MR should be performed in all patients with focal liver lesions for better characterisation.
Hepatocellular carcinoma in non-cirrhotic liver: In this study, two patients presented with HCC in non-cirrhotic liver. Both lesions (100%) were Hypointense on T1 weighted and hyperintense on T2 weighted. HCC in non-cirrhotic liver are smaller than in cirrhotic measuring less than 4 cms in contrast to the study done by Winston CB et al., [13], which reviewed MR images in 36 patients with HCC and observed that lesions in cirrhotic livers differed significantly from those in non-cirrhotic livers in terms of size. The diagnosis is probably delayed in cirrhotic liver because of the ill-defined and heterogeneous nature of the lesion on ultrasound.
In the study by Grazioli L et al., [14], the pseudocapsule (thickness 0.2-6 mm) was present in 26 of 37 nodules (70%). The dynamic study was the most suitable technique to show the pseudocapsule, which was recognised in 80.7% (21 of 26 nodules). In 5 of 26 cases, the pseudo capsule, not demonstrated by MR, was thinner than 0.4 mm. In 16 of 21 cases, in the early portal phase (30-60 seconds), the pseudo capsule had an early enhancement, which was more evident later; in 5 of 21 cases the enhancement was observed only in the late portal phase (1-2 min).
Vascular involvement like encasement and invasion into the adjacent vessel is a finding indicating malignancy. We could find vascular invasion (portal vein) in only two patients (22.3%) as most of the lesions are peripherally located and microscopic invasion could not be detected on imaging. In a recent study [15] of 322 patients undergoing curative resection of HCC, 15.5% had macroscopic venous invasion and 59% had microscopic venous invasion at histopathologic analysis. Both the studies have comparable results. The overall Sensitivity, Specificity, Positive predictive value, Negative predictive value for diagnosing HCC has increased to 88.89%, 96.77%, 88.89%, 96.77% respectively with contrast enhanced MR as compared to the plain imaging.
In a study by Elizabeth M et al., [16], retrospectively assessed the usefulness of contrast material- enhanced T1-weighted magnetic resonance (MR) imaging alone and with T2- weighted MR imaging in the diagnosis of Hepatocellular Carcinoma (HCC). At liver explantation, 57 lesions were present in 18 patients. Contrast- enhanced T1-weighted imaging depicted 13 of 19 HCCs with an overall sensitivity of 68.4% (13 of 19) and specificity of 65.7% (23 of 35).
Metastasis: In this study, eight patients with 16 metastases to liver were studied. Five patients were diagnosed cases of primary malignancy and three patients did not have evidence of extrahepatic primary malignancy at the time of MRI examination. These patients were referred for evaluation of liver mass.
According to the study by Goldberg A et al., [17] the majority of liver metastases have a higher cellular and interstitial water content of tumour tissue compared to normal liver parenchyma which renders metastases hypointense on non-enhanced T1-weighted images and hyperintense on T2W images [17]. In the present study, 15 (94%) lesions were hyperintense on T2 and one lesion was hypointense with hyperintense rim which was hemorrhagic metastasis from CA rectum.
Intense perilesional enhancement of metastases on gadolinium-enhanced MR images correlates with histopathologic hepatic parenchymal changes, which include peri-tumoral desmoplastic reaction, inflammatory cell infiltration, and vascular proliferation [18]. Two lesions (12%) showed persistant heterogeneous enhancement in all phases. One was metastasis from CA rectum and another lesion was metastasis from operated HCC.
Danet IM et al., [19] retrospectively reviewed MRI of 165 consecutive patients who had untreated liver metastases The most common pattern was peripheral ring (72% of patients) seen on the arterial dominant phase images. One metastatic lesion (6%) showed heterogeneous enhancement with washout in portal and equilibrium phase which turned out to be hypervascular metastasis from an unknown primary.
Epitheloid Hemangioendothelioma (EHE): One lesion of Epitheloid hemangioendothelioma in a 32-year-old male was studied. We had given a possibility of cholangiocarcinoma as epitheloid hemangioendothelioma is not a common focal liver lesion. Previous Studies by van Beers B et al., [20] and Bartolozzi C et al., [21] showed Epitheloid hemangioendothelioma characteristically have a dense fibrotic hypovascular central core and a peripheral hyperemic rim. Retraction of the adjacent liver capsule may occur, likely as a result of lesion-related fibrosis. This is an unusual feature in malignant lesions of the liver, and is suggestive of EHE. The center of the lesion may contain one or several concentric zones of various intensity. These areas are related to connective tissue admixed with calcifications or coagulation necrosis [22]. On post-contrast imaging, peripheral tumour enhancement is noted surrounding the central low-intensity fibrous core. A thin hypointense rim may be seen surrounding the enhanced periphery of the EHE, correlating with the avascular rim seen on pathology. Marked enhancement of the lesions is demonstrated on delayed imaging.
Cholangio carcinoma: In this study, one lesion of cholangio carcinoma was studied in 62-year-old female. It had presented with pain, anorexia, weight loss, jaundice and lump. The lesion was hypoechoic on ultrasound. It was diagnosed accurately on MRI as lesion showed typical delayed enhancement in equilibrium phase with additional features of proximal biliary dilatation.
Similar enhancing characters are also described by Yoji Maetani et al., [23] in a study of 50 patients and showed that on contrast, lesions showed patchy peripheral enhancement in arterial or portal venous phase followed by progressive centripetal enhancement in delayed phases.
Hepatoblastoma: One lesion of hepatoblastoma was studied in 25-year-old female. However hepatoblastomas are commonly seen in age group of less than five years. Lesion was involving entire right lobe and was T1 hypointense with hyperintense areas suggestive of hemorrhage within. Lesion was heterogeneously hyperintense on T2 weighted images with areas of haemorrhage and necrosis. It showed peripheral discrete nodular enhancement in arterial enhancement. Portal and equilibrium phase showed increased heterogenous patchy enhancement. With these imaging features and age of patient, the lesion was characterised as giant hemangioma. Patient was operated and histopathology proven to be hepatoblastoma.
Study done by Dachman AH et al., [24] showed on MRI that the hepatoblastoma appears as a heterogeneous isointense or hypointense mass on T1-weighted un-enhanced images with variable haemorrhage and intermediate intensity seen on T2-weighted images. During the arterial phase of dynamic Gd-enhanced imaging, the lesion becomes heterogeneously hyperintense, except for the fibrotic and necrotic areas. On portal venous and equilibrium phases, the tumour rapidly appears isointense and subsequently hypointense.
Carcinoma gall bladder with infiltration of liver: We had two patients of CA Gall bladder infiltrating right lobe of liver. One was measuring 10 cms and another being 6 cms in the largest dimension. Both lesions were hypoechoic on ultrasound infiltrating liver with non-visualised gall bladder. Both lesions were heterogeneously hyperintense on T2 weighted images with mild heterogeneous enhancement in arterial phase with delayed increase in enhancement in portal and equilibrium phase clearly differentiating them from HCC. There were also enlarged lymph nodes noted at porta. With these features, both lesions were accurately characterised on MRI as gall bladder was not separately visualised. Histopathology proved both lesions to be carcinoma gall bladder infiltrating liver.
Benign Lesions
Hemangiomas: In this study six patients (16 lesions) with hemangioma were studied. Five (31.2%) of them were giant hemangiomas (more than 6 cm) with average size of 13 cm while rest 11 (68.7%) were small hemangiomas with average size of 2.5 cm. One patient had hemangioma in background of cirrhotic liver. On T1W images, all (100%) hemangiomas were hypointense. However larger hemangiomas were 13 (81%) were hyperintense on T2W imaging.
On T2-weighted images hemangiomas demonstrate a markedly bright signal as hemangiomas are comprised of blood-filled spaces or vascular channels lined with a single layer of endothelium separated by fibrous septa. There may be areas of thrombosis or fibrosis. Very slow blood flow is characteristic in the lesions [25].
In a study done by Semelka et al., [26], most of the medium (1.5-5 cm), and large hemangiomas (>5 cm) had initial peripheral nodular enhancement, whereas uniform enhancement was observed in 35 of 81 small lesion.
In the present study, all (16 lesions) hemangiomas were correctly diagnosed on MRI because of typical characteristics and contrast enhancement features seen. The sensitivity and specificity of characterisation of hemangiomas is 80% and 99% respectively by Quillin SP et al., [27] They evaluate proven focal liver lesions in 128 patients with hemangiomas which showed slightly low sensitivity compared to the present study. Khalid. M. Elsayes et al., study concluded the inability to definitively characterise 29% of hemangiomas on MR images, due to either the small size of the lesion or an atypical enhancement pattern [28].
Simple and complex cysts: This study had two patients with three complex cysts and two patients with 2 simple cysts. The differentiating features between simple and complex cyst were internal thin septations with few tiny nodules which was seen in complex cysts. There was no post-contrast enhancement in both lesions. Findings were similar to study done by Koenraad J et al., [29]. In their study on MR characteristics of cystic liver lesions, they inferred that the findings like septae, calcification or internal nodules were important in the characterisation of liver cysts as complicated.
In a study by Quillin SP et al., [27] included analyses of total of 311 proven focal hepatic masses in 128 patients, they found 45 hepatic cysts and none showed contrast enhancement with sensitivity of 100%. The findings are similar in four patients of the present study with no enhancement in any of the simple or complex cysts. However, this study has small sample size.
Hepatic adenoma: Total three lesions of hepatic adenomas were studied in two patients and both were females in the age group of 27-28 yrs. One patient had IN PHASE AND OUT OF PHASE imaging was performed in both patients.
Accurate diagnosis was made in both patients correlating with the history. All the lesions were proved to be hepatic adenomas on histopathology.
In the study by Grazioli L et al., [30] showed similar findings of hepatic adenoma. Their study showed, On T1-weighted images, frequently the lesion is heterogeneous in appearance due to areas of increased signal intensity related to fat, glycogen or recent hemorrhage, and low signal intensity areas corresponding to necrosis or old hemorrhage. About one-third of adenomas have a peripheral rim, corresponding to a fibrous capsule; frequently the rim is of low signal intensity on both images.
Focal nodular hyperplasia: This study had one lesion of Focal nodular hyperplasia in a 33-year-old female. The lesion was typically well-defined with clear-cut margins, uncapsulated, yet hypoechoic on ultrasound. Lesion showed arterial enhancement and washout in portal phase with enhancing scar in equilibrium phase. It was proved on histopathology.
Similar findings were reported by Mortele KJ et al., [31] in 48 patients with FNH, On T1- and T2-weighted images, lesions appeared predominantly hypointense (69.5%) and hyperintense (72.7%), respectively.
Regenerating nodules: This study had one patient with multiple regenerating nodules in background of cirrhotic liver which were involving both lobes heterogeneously hypoechoic on ultrasound. All the lesions were hypointense on T1 and T2 weighted images with no post-contrast enhancement. With the typical imaging findings, patient had no further work-up done. Lencioni R et al., [11]. study showed similar characters in regenerating nodules. Lesion signal intensity on baseline T1-weighted and T2-weighted images may help differentiate HCCs from regenerating nodules in cirrhosis [32].
Hydatid cysts: Two lesions of hydatid cysts of the liver were evaluated. In both the patients, lesions were well-defined with smooth margins. They were hypointense on T1W images and hyperintense on T2WI with low intensity peripheral rim. Peripheral rim was more apparent in T2W images. Minimal enhancing peripheral low intensity rim was seen in both (100%) and is characteristic finding of hydatid cyst. Both the patients were operated and proved to have hydatid cysts on histopathology.
Similarly Wojtasek DA et al., [32] studied the MR characteristics of hepatic hydatids and found out that the low signal intensity rim described on T2WI was not found in all cases and that MR was superior to other modalities in delineating the internal contents of the hydatid cyst. This finding was seen in both lesions of the present study. Kodama Y et al., [33] studied MR characteristics of 50 liver hydatid cysts. In both the lesions in the present study, we did not find daughter cysts, probably because one lesion was ruptured and also due to small sample size.
Abscesses: Two lesions of liver abscesses were studied. Both lesions showed thick wall (100 %). Both the lesions (100%) were hypointense on T1W and hyperintense on T2W images. One lesion (50%) showed peri-lesional edema. Post-contrast, both lesions showed peripheral enhancement in all the phases. They were proved to be abscess on FNAC with causative organism being staphylococcus and klebsiella respectively.
Findings were similar to the study done by Mendez RJ et al., [34]. Which showed MR imaging increased the peripheral rim enhancement. Peri-lesional edema is seen on T2-weighted MR images in 50% of abscesses, although it may also be seen in 20%-30% of patients with primary or secondary hepatic malignancies [34]. Therefore, the presence of peri-lesional edema can be used to differentiate a hepatic abscess from a benign cystic hepatic lesion [34]. This was seen in one lesion of the present study.
Tuberculomas: One patient had multiple 0.5-1 cm sized well-defined lesions which were hypoechoic on ultrasound. On T1W, all these lesions were hypointense.
On FNAC, they proved to be tuberculomas. The differentials to be considered for such lesions are lymphoma and other granulomas. The original description of hepatic tuberculosis by Alvarez SZ et al., [35] classified the disease as 1) Miliary, as a part of generalised disease and 2) local, with focal involvement of liver where extrahepatic disease is not obvious. In the present study, multiple tuberculomas in liver were part of disseminated tuberculosis with similar lesions noted in spleen.
Focal fatty sparing: One patient with a large focal fat sparing was studied in the middle aged female patient. On ultrasound, there was isoechoic area in both lobes with no mass effect. On CT, there was a large high attenuation defect in segment IV,V,VI,VII. In MRI, chemical shift imaging was performed, lesion presented as isointense on IN PHASE T1W images and hyperintense on OUT PHASE T1W images compared to the rest of liver. On T2, lesion was Iso to hypointense and the vascular structures were normally traversing through the lesion. This was pathognomonic of focal fat sparring. Hence patient didn’t undergo any intervention.
The findings were similar to study done by Wynnson W. Tom et al., [36]. They observed that MR is the best way to adequately characterize fat by opposed-phase imaging. This technique is based on the different precession velocities of fat and water observed after excitation in the transverse plane and the condition to be observed is that water and fat coexist in the same tissue voxel.
Limitation(s)
Firstly, small sample size was the limitation of the study. Secondly, selection bias might be there as all subjects of the study were selected on basis of Ultasound examination. Thirdly, Magnetic Resonance Imaging involves breath holding with long procedure time which creates issues to many patients even after being a good diagnostic modality.
Conclusion(s)
MRI is superior as compared to other modalities like ultrasound and CT in having high spatial resolution with multiple sequences like T1, T2 and fat suppression techniques like IN PHASE, OUT OF PHASE helps in demonstrating lesion characters like architecture, margin, haemorrhage, fat component and vascular invasion of the lesions. MRI is a modality of choice for focal liver lesions in patients with contraindications for Computed Tomography like pregnant patients, paediatric patients and contraindication for iodinated contrast like patient with renal dysfunction. MRI is valuable for the characterization of focal liver lesions detected on Ultrasonography. Basic MRI sequences along with chemical shift imaging sequences and dynamic contrast imaging has significant role in characterising the focal liver lesions.