Oral cancer is among the top three types of cancers in India and 90-95% of the oral cancers is Squamous cell carcinoma [1,2]. It has been envisaged by the International agency for research on cancer that India’s incidence of cancer will increase from 1 million in 2012 to more than 1.7 million in 2035 [1]. Oral cancer mostly affects males, after the fifth decade of life and is associated with mutations in genes that regulate cell growth and apoptosis leading to uncontrolled proliferation of tumor cells, which occur due to the exposure to tobacco, alcohol and betel quid [3,4]. Researchers have investigated the etiology of infectious agents in causing cancer and majority of them are on Human papilloma virus (HPV) and Candida serving as potential causes of Oral Cancer [3-5]. But the least discussed factor is the bacterial cause of oral carcinogenesis, among the bacterial origin H. pylori is considered as one of the etiological factors for oral cancers [6]. The H. pylori is already an established gastric pathogen in the world and is accountable for chronic gastritis, peptic ulcer disease, gastric adenocarcinoma, pancreatic and hepatocellular carcinoma [6], but the association between H. pylori and oral squamous cell carcinoma (OSCC) is still in the grey area of study and needs more validated research [7]. The existence of H. pylori is reported in the oral cavity, but whether the oral cavity serves as an extra gastric source for H. pylori or carries the organism only transiently is litigious [8]. Oral cancer associated with H. pylori infection evolves as a consequence of histological changes in the buccal mucosa due to chronic inflammation, which culminates initially into dysplasia and, at later stages, into cancer [9]. To establish this association, the primary objective of the study was to detect H. pylori in cohort of patients with Oral squamous cell carcinoma, Oral potential malignant disorders (premalignant lesions and conditions), and Healthy controls and secondary objective was to evaluate the contributory role of other risk factors like tobacco and alcohol in the development of oral cancer.
Materials and Methods
This prospective case-control pilot study was undertaken in the Department of Microbiology, S.B.K.S Medical Institute and Research Center, Piparia, Gujarat for the period of four months from June 2018 to September 2018. The present study was done on 35 patients, with age 30-70 years (mean age 52.1±5 years) diagnosed as either OSCC or oral potential malignant disorders based on clinical examination and confirmed by histopathology report. Fifteen age and sex matched healthy persons were employed as control.
Inclusion criteria: Patients attending the Ear Nose Throat (ENT) Outpatient Department (OPD)/Oral surgery OPD had varied symptoms like ulcerative lesion or growth on buccal mucosa/tongue/vestibule/floor of mouth/lips, pain while chewing food, burning sensation, restricted mouth opening, white patch or a red macule on cheek.
Exclusion criteria: Patients taking Non-steroidal anti-inflammatory drugs (NSAIDS) in the past four weeks or those on Proton pump inhibitors (PPI) or those patients who had endoscopic evidence of gastritis/gastric cancer/ peptic ulcer disease due to H. pylori and treated with antibiotics within the preceding six months and those not willing to participate were excluded from the study.
On the basis of results of Post Histopathological Reports, patients were categorized into three groups:
Group A comprise of all those patients having OSCC (n=11). Includes patients with Keratinizing Squamous Cell Carcinoma (n=1 patient, site: buccal mucosa), Well Differentiated Squamous Cell Carcinoma (n=4 patients, site: each from buccal mucosa and tongue), Verrucous carcinoma (n=3 patients, site: tongue and left lower lip) and Early Invasive Carcinoma (n=1 patient, site: buccal mucosa), Moderately Differentiated Squamous Cell Carcinoma (n=2 patients, site: buccal mucosa).
Group B comprises of those having Oral potentially malignant conditions (n=24). Includes patients with Lichen Planus (n=5 patients, site: 3 from buccal mucosa and 2 from the floor of mouth), Erythroplakia (n=2 patients, site: each one from buccal mucosa and vestibule), leucoplakia (n=3 patients, site: two from buccal mucosa and 1 from the floor of mouth), Oral Sub Mucus Fibrosis (n=10 patients, site: 7 from buccal mucosa, 3 from the floor of mouth) and ulceroproliferative lesions (n=4 patients, site: tongue).
Group C was the control group (n=15) with no symptoms but had habits of tobacco.
The study was commenced after the approval from Sumandeep Vidyapeeth Institutional Ethics Committee (SVIEC/ON/Medi/SRP/18026). An informed consent was obtained along with the detailed proforma regarding the demographic details of the patient, including the comprehensive lifestyle habits, symptoms and clinical findings.
Two Oral Punch Biopsy samples (lesions from buccal mucosa, margins of the tongue and from the floor of the mouth) were collected from each patient and were transferred to a 2 mL of sterile normal saline and sent to the microbiology laboratory for further investigations.
Rapid urease test [10]: Biopsy was immediately placed on the Rapid urease test kit (HelicoRapt Kit was procured from Triage systems, Mumbai, India). A color change from yellow to pink was noted within 5 minutes. any change in the color after 5 minutes were considered as false positive.
Gram’s staining [11]: One oral biopsy was crushed and smears were prepared on a clean Glass slide and stained with the standard protocols. Presence of spiral shape Gram negative microorganism embedded in the tissue cells were noted.
Serology: IgG antibodies were detected in the patient’s serum by rapid test based on the principle of immunochromatography. Kits were procured for SD Bio Standard Diagnostics, Alere, India. Sample was processed according to the protocol given by manufacturer. Presence of band in the test and control region was considered to be positive.
Statistical Analysis
A data analysis was conducted using Statistical Package for Social Sciences (SPSS) version 15.0. Odd ratio was calculated to evaluate the risk factors. p-value <0.05 was taken as significant.
Results
Thirty-five subjects, 32 males (91.4%) and 03 females (8.57%) were enrolled in the study. Demographic details of the enrolled patients are shown in [Table/Fig-1] and [Table/Fig-2] which clearly indicates male predominance. Education till primary school was found in 65.71% patients. Looking into the depth of their life style habits, the study found that 88% patients were addicted to tobacco in the form of Gutkha and Mava, out of which 51.61% had an inclination of consuming it four times a day, 29% seven times a day and 16% 10 times a day. 31% patients had a practice of putting betel quid in mouth while sleeping, more than half of them had this habit since past 10 years. 48% had a habit of smoking Bidi and more than 60% are addicted in the past two decades.
Demographic details of the patients enrolled in the study (n=35).
| Variables | Number | % |
|---|
| Gender | Male | 32 | 91.43 |
| Female | 03 | 8.57 |
| Age-groups (years) | 30-40 | 09 | 25.71 |
| 41-50 | 08 | 22.86 |
| 51-60 | 10 | 28.57 |
| 61-70 | 08 | 22.8 |
| Residence | Rural | 32 | 91.43 |
| Urban | 03 | 8.57 |
| Education | Uneducated | 02 | 5.71 |
| Primary | 23 | 65.71 |
| Secondary | 06 | 17.14 |
| Higher secondary | 04 | 11.4 |
| Life-style habits | Chewing tobacco (Gutkha/mava/areca nut) | 31 | 88.57 |
| Alcohol | 05 | 14.28 |
| Smoking (Bidi/Cigarette) | 17 | 48.57 |
| Habit of betel quid in mouth while sleeping | 11 | 31.43 |
| Healthy diet | Yes- Regular diet rich in enough folates | 10 | 28.5% |
| Oral hygiene | Yes- Maintain oral hygiene | 17 | 48.5% |
Comprehensive lifestyle practices of enrolled patients.
| Variables | Number | % |
|---|
| Chewing tobacco (n=31/35) Gutka (n=19)/Mawa (n=7)/areca Nut (n=5) | Consumption (times/day) | 2-4 | 16 | 51.61 |
| 5-7 | 09 | 29.03 |
| 8-10 | 05 | 16.12 |
| >10 | 01 | 3.22 |
| Since how many (years) | 5-10 | 11 | 35.48 |
| 11-15 | 12 | 38.70 |
| 16-20 | 02 | 6.45 |
| 21-25 | 06 | 19.35 |
| Smoking tobacco (n=17/35) Bidi (n=12)/Cigarette (n=5) | Number (pk/day) | 1 | 15 | 88.23 |
| 2 | 02 | 11.76 |
| How many (years) | 5-10 | 11 | 64.71 |
| 11-15 | 03 | 17.64 |
| 16-20 | 03 | 17.64 |
| Alcohol (n=5/35) | Since how many (years) | 1-10 | 02 | 40 |
| 11-20 | 03 | 60 |
| Chewing betel quid in mouth during night and sleeping with the quid (n=11/35) | Since how many (years) | 1-10 | 06 | 54.54 |
| 11-20 | 04 | 36.36 |
| 21-30 | 01 | 9.09 |
Out of 35 enrolled, 11 patients were confirmed OSCC patients from rural area, with a prevalence rate of 31.4%. Mean age affected was 45.6 years. Male patients (81.8%) out numbered the female patients (18.2%). 72.7% (8/11) patients were not maintaining enough oral hygiene. 81.8% (9/11) patients have not incorporated enough folates (vegetables and fruits) in regular diet. 90.9% of the patients were addicted to tobacco with a range from minimum 3 to 25 years and 54.5% taking betel quid in mouth while sleeping. Out of 11 OSCC, 5 (45.5%) were positive for H. pylori infection.
Detection of H. pylori and its association with various attributes
H. pylori were detected by two invasive (Gram’s stain and Rapid Urease test) and one non invasive method (Serology- IgG). The Gold standard definition followed was: if any two tests are positive out of three, then it is considered as H. pylori positive with active infection. If any single test is positive then the test is considered negative and if only serology is positive, then it is considered as past infection.
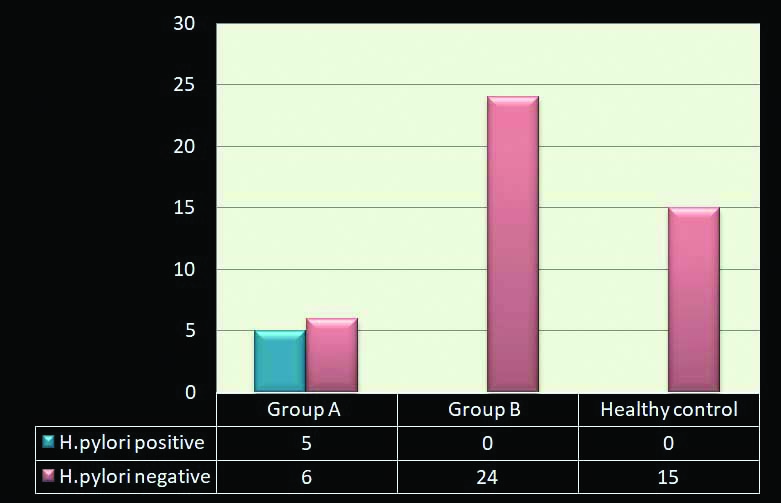
In present study, five samples positive for H. pylori out of 35 with the prevalence of 14.28%.
All the five patients were confirmed as Oral Squamous Cell Carcinoma (Group A) by histopathology. Out of five patients, two were established as Well-differentiated Keratinizing Squamous cell Carcinoma, two having Oral Verrucous carcinoma, one having Moderately Differentiated Squamous Cell Carcinoma [Table/Fig-3]. None of the patients with Potentially Malignant Disorders (Group B) and Control samples was positive for H. pylori in [Table/Fig-4]. [Table/Fig-5] assessed the role of individual risk factors in patients with Oral Squamous Cell Carcinoma. The study found that out of 11 OSCC patients, 10 were consuming tobacco since decades (OD-16.19), six patients had a habit of putting betel quid in mouth while sleeping (OD-4.56), five patients were infected with H. pylori (OD-0.83) and five were smokers (OD-0.83).
Characteristics of all enrolled patients with OSCC (n=11) in relation to gender, age, site of lesions, Habits and H. pylori status.
| Oral cancer | Gender/Age | Symptoms | Site of lesion | Habit of tobacco and smoking and Betel quid | H. pylori status by all the 3 tests |
|---|
| Keratinizing well differentiated squamous cell carcinoma | M/45 | Pain and burning while chewing food | Buccal mucosa | Yes, since 20 years | Positive |
| Well differentiated squamous cell carcinoma | M/65 | Pain and burning while chewing food | Buccal mucosa | Yes, since 10 years | Negative |
| Oral verrucous carcinoma | M/45 | Lesion on the upper lip | Lips and angle of mouth | Yes, since 20 years | Positive |
| Well differentiated squamous cell carcinoma | M/64 | Lesion on the sides of tongue | Tongue | No | Positive |
| Oral verrucous carcinoma | M/45 | Lesion on the upper lip and angle of mouth | Upper margin of lips | Yes, since 25 years | Negative |
| Well differentiated squamous cell carcinoma | M/41 | Growth on the buccal mucosa | Buccal mucosa of Right cheek | Yes, since 12 years | Negative |
| Well differentiated squamous cell carcinoma | F/35 | Growth on the left buccal mucosa | Buccal mucosa | Yes since 3 years | Negative |
| Early invasive carcinoma | M/42 | Restricted mouth opening | Buccal mucosa | Yes, since 22 years | Negative |
| Ulceroproliferative growth on the left margin | F/42 | Lesion on the sides of tongue | Left margin of tongue | Yes, since 15 years | Negative |
| Oral verrucous carcinoma | M/38 | Lesion on the sides of tongue | Tongue | Yes, since 15 years | Positive |
| Moderately differentiated squamous cell carcinoma | M/50 | Restricted mouth opening and difficulty in chewing food | Buccal mucosa | Yes, since 13 years | Positive |
M: Male; F: Female
Detection of H. pylori in Group A (OSCC, n=11), Group B (Oral potentially malignant disorders, n=24) and Healthy control (n=15).
Evaluation of individual risk factors leading to oral squamous cell Carcinoma (Group A) and oral potentially malignant disorders (Group B).
| Variables | Group A (N=11) | Group B (N=24) | Odd ratio | Chi Square | p-value |
|---|
| Chewing tobacco | Yes (31) | 10 | 21 | 16.19 | 0.0886 | 0.77 |
| No (04) | 01 | 03 |
| Smoking tobacco | Yes (17) | 05 | 12 | 0.83 | 0.0624 | 0.80 |
| No (18) | 06 | 12 |
| Habit of chewing betel quid and sleeping with quid | Yes (11) | 06 | 05 | 4.56 | 3.977 | 0.046 |
| No (24) | 05 | 19 |
| H. pylori infection | Yes (05) | 05 | 0 | 0.83 | - | - |
| No (30) | 06 | 24 |
p-value <0.05 is significant
Discussion
The Center for Disease Control and prevention (CDC) estimates that approximately two-thirds of the world’s population harbors H. pylori and the bacteria have coexisted with human for many thousands of years [12]. In 1994, H. pylori was recognized as carcinogen causing gastric adenocarcinoma and mucosa associated lymphoid tissue lymphoma [5]. H. pylori is also linked to the development of OSCC which is among the top 3 cancers in India after the lead of Breast and cervical cancer [3]. Conventionally oral cancer has always been associated with tobacco, Betel quid and areca nut chewing habit, it has been found that H. pylori infection leads to direct cell damage and provokes the release of proinflammatory mediators as well as it also stimulated the immune response which further causes the release of cytokines and oxygen radicles and aids in the mechanism of carcinogenesis [5].
The present study have tried to evaluate the association of H. pylori in the patients with Oral cancer and Oral potentially malignant disorders. The study found only five cases positive out of 11 for H. pylori from patients with OSCC showing male preponderance and mean age group affected was 46.5 yrs. H. pylori was detected from the lesion of buccal mucosa, tongue and from Lips and angle of mouth. All the five positive patients were addicted to Tobacco and betel quid ever since a decade. It is certainly unclear that oral H. pylori infection may interrelate with tobacco use, alcohol use, or both to augment the risk of squamous cell carcinomas.
Association of H. pylori in oral premalignant diseases and OSCC was determined and lot of studies has concluded that there is positive association between them. In a study done by Fernando N et al., [13] in patients with OSCC, 26.4% H. pylori positive cases by serology were observed and a greater additive risk for the patients exposed to both H. pylori and tobacco or alcohol were found, as H pylori infection along with tobacco habits may modify the flora of oral cavity [7]. A study done by Sharma P et al., [9] in 2015 also suggests, high prevalence of H. pylori in the oral cavity of patients with premalignant conditions and OSCC. An unusually finding was seen in a study done by Irani S et al., [5] in 2013, detected the coccoid form of H. pylori in the patients with OSCC, which might be proof for its long-standing persistence in the oral cavity and also its the role in the pathogenesis of the oral disorders and concluded as a risk factor. A study done by Dayama A et al., [7] also found a positive association between risk of oral cancer and H. pylori infection using culture and 16sRNA PCR technique. Recent study done by Meng X et al., [14] in 2015 suggests that there is negative association of H. pylori in oral cancer patients. The present study could not find any positive finding in oral potentially malignant disorders (0/24) like lichen planus, erythroplakia, leukoplakia and OSMF and healthy controls. This finding was not in accordance with the study done by Kazanowska-Dygdała M et al., [15] in which they observed the presence of H. pylori DNA in the oral cavity of patients with oral leukoplakia and oral lichen planus.
Limitation(s)
The study was a pilot study conducted for a period of four months only, so due to time constrain the sample size was limited. However, the study definitely offers an avenue for further work on bigger cohort populations to confirm and to quantify this possible association more precisely.
Conclusion(s)
H. pylori might be associated with the etiopathogenesis of OSCC. However, results of this pilot study do not establish a definite causal relationship between H. pylori and OSCC.