COVID-19 pandemic has severely affected sports worldwide. Usual practice can’t be done due to high viral transmission, yet prolonged inactivity leads to detraining and deconditioning and threatens ending of sporting career. Depending on the present guidelines of the government, a safe and evidence based gradual resumption of training and sports is essential. The cardiorespiratory- neuromuscular system involvement among others in COVID-19 directly affects exercise-sports performance and health, and the possibility of sub-clinical transmission poses immense challenge. Like other games, swimming is also heavily affected. Although COVID-19 is transmitted by droplets, the prolonged presence of virus in the air currents, commonly-touched surfaces and in stool of those infected should be kept in mind. Importance of hand hygiene, cough and sneeze etiquette, social distancing, use of mask while not exercising hard, other good public hygiene practices, staying home if sick, frequent cleaning and disinfection of pool and frequently touched surfaces, early detection, isolation and adequate treatment for the positive cases and strictly following government guideline should be compulsory. Awareness program and continued education for athletes, parents, coaches, support staff and other management team should be done. This review is intended to understand the course of COVID-19 and to formulate guidelines for resumption of swimming in India, based on recommendations by various organisations like WHO, CDC etc. The aim being to act as a key support for safely resuming swimming yet reducing the risk of COVID-19 infection.
Introduction
COVID-19 pandemic has led to significant restrictions on all sectors of society, including sports, thereby causing devastating effects globally [1]. It has forced elite athletes of different sports to an unexpected stop not only of competitions but also of training sessions [2]. Prolonged periods of inactivity results in detraining effects on maximal oxygen consumption, muscle strength, muscle mass and endurance capacity. It reduces lubrication and nutrition of joint cartilage leading to degeneration resulting in an imbalance in the joint structures (cartilage, ligaments, synovium) [3]. Resumption of training is warranted to reverse the physiological decline with standard precautions against COVID-19. Understanding the course of disease is important to lay down guidelines for resumption of training specific to swimming athletes in India.
Literature Search
An extensive search on commonly used research databases and search engines such as PUBMED and Google Scholar was done using keywords, COVID-19, resumption of swimming, return-to-sport, pool disinfection etc. A total of 22064 articles were found using the keyword COVID-19 and 96 articles were found on resumption of sports. Out of which only 12 articles were found related to our research topic. In addition to this the recommendations by the CDC, WHO and ICMR were included in the article.
Background on COVID-19
After the first outbreak of novel beta corona virus in Wuhan City, Hubei Province, China, a public health emergency was alarmed in December 2019. It was called 2019-novel coronavirus (SARS-CoV-2). It was stated to be a worldwide epidemic with high mortality and morbidity [4-6]. The novel coronavirus (COVID-19) outbreak was declared a global pandemic by World Health Organisation (WHO) on 11 March 2020 [7]. The spectrum of disease caused by coronaviruses varies from common cold to more severe diseases including Middle East Respiratory Syndrome (MERS) and Severe Acute Respiratory Syndrome (SARS). SARS-CoV-2 is the virus responsible for COVID-19 [8]. It is an enveloped virus and lysis of the envelope results in loss of function to cause infection [9]. Mode of transmission (human-to-human) is via droplets or direct contact. Waterborne transmission has never been established in humans. However, since SARS-CoV-2 has been found in fecal samples and anal swabs of some patients, the possibility of feco-oral transmission cannot be overlooked. Primarily, people with co-morbid conditions and elderly are at high risk [10]. Although athletes are not considered under high risk, there is a possibility of occurrence in otherwise fit and previously healthy athletes.
Clinical picture is highly variable from completely symptom-free to a fatal course [10-12]. Two-14 days after exposure to the virus, symptoms tend to occur. Individuals with COVID-19 may present with symptoms like cough, shortness of breath or difficulty in breathing, fever, chills, myalgia, sore throat, anosmia, dysgeusia, anorexia and other gastrointestinal symptoms [13]. The organ manifestations and symptoms are in par with pronounced inflammatory response [11,14,15]. Impaired coagulation has also been observed with increased thrombophilia leading to pulmonary or central embolisms [16]. The lungs, cardiovascular system, the central and peripheral nervous system, skeletal muscle, as well as the liver and kidneys are affected in the acute phase. Apoptosis is seen in various organs, especially heart, intestines and lungs [12,17,18].
Organ specific complications: Most frequently involved organ is the lungs. Pneumonia occurred in 20% of all positive cases in China with a severe (14%) or even critical course characterised by pulmonary infiltrates in more than 50% of the lung and a fall in oxygen saturation below 94%. With respect to athletic exercise capacity, slight impairment in gas exchange may limit maximum ventilation, oxygen consumption and/or disrupt respiratory economy which may lead to development of right heart load etc [10].
In the cardiovascular system, myocarditis is one of the leading causes of sudden cardiac death among athletes younger than 35, mainly due to viral infection of upper respiratory tract and gastrointestinal tract [10,19]. Fulminant myocarditis due to COVID-19 has also been established. Other manifestations include acute coronary syndrome, myocardial infarction, thromboembolic events in the periphery as well as the lungs [17,20].
Other organs are also involved. Neurological symptoms like headache, dizziness, anosmia, dysgeusia and stroke have been reported [21,22]. Some case reports also describe the onset of Guillain-Barré syndrome [23]. About 43% of the hospitalised COVID-19 patients reported by Sun P et al., complained of skeletal muscle pain. Also, evidence shows a risk of markedly prolonged convalescence with pronounced symptoms of fatigue and drop in performance post infection [24,25].
Impact of COVID-19 on Athletes
Safeguarding the health of athletes and support personnel involved in most major sporting events at international, regional and national levels is of paramount importance for major sports event organisers and sports federations, thus leading to cancellation or postponement of these events. For instance, International Olympics committee has postponed the conduct of Olympics and Paralympics, for the first time in the history of the modern games, to 2021. However, this has placed tremendous pressure over the competitive athletes to reschedule their training, while trying to stay fit at home, and risk losing professional sponsors. This has immensely jeopardized their mental health. The team environment and support personnel are critical for athletes involved in team sports. It has been seen that team training boosts performance as well as lessens the subjective pain sensation during training [26]. The sudden shift due to the restrictions imposed due to COVID-19 to individual-exercise can place significant stress on the athletes and can be frustrating, painful and lonely.
When compared with normal situation, the present pandemic situation poses further difficulties and constraints in terms of logistics in providing sport-specific exercise strategies and training solutions. On 24 March 2020, the Government of India ordered the first phase of lockdown nationwide, which reached phase 5 with various confinement strategies till date. With strict restrictions and confinement, athletes are likely to be exposed to various degrees of detraining which is partial or complete loss of training-induced adaptations both morphological and physiological as a consequence of lower training stimuli [27].
Cardiorespiratory and neuromuscular adaptations are fundamental in different sports, and substantial declines are known to occur after short-term (<4 weeks) training cessation. Short term unloading may result in alterations in mechanical properties of tendon and reduction in muscle size, strength, power and rate of force development making the athlete prone to injury [28-30].
Although the scope of this study is limited to swimmers, a sports specific reconditioning with general precautions for COVID-19 should be in order for all athletes because these athletes may not be prepared to cope with the surge in training and match demands as the pandemic situation starts to improve.
Preventive Measures Specific to Swimming on Resumption of Training
Even though the evidence of spread of COVID-19 via water used in pools is lacking, still adequate operation and disinfection of pools, water playgrounds or hot tubs should be done, which will also kill the COVID-19 virus [31].
Preventive Measures for COVID-19 at Aquatic Venues include [32]:
(a) Following proper hand hygiene and cough etiquette- It is important to encourage all swimmers and staff to wash their hands frequently with soap and appropriately cover their coughs and sneezes.
(b) Physical distancing or social distancing is one of the most efficient and easy way to reduce the spread of virus. It is important to practice physical distancing principle to maintain more than 1.5 m (six feet) separation between individuals. In addition, it is wise to maintain a minimum area of more than 2 m2 per person.
(c) Masks/Cloth for covering face- It is better to encourage the use of masks or cloth face coverings wherever feasible. These become an essential part when physical distancing is not possible. Care need to be taken to advise not to wear masks in the water as they can be difficult to breathe through when they’re wet. In addition, the swimmers need to be advised to avoid touching eyes, nose and mouth.
(d) Staying home- It is essential to educate the staff and swimmers on when to stay home. Certain situations are: if they have any of the symptoms suggestive of COVID-19, if they have tested positive for COVID-19, or if they were exposed to someone with COVID-19 within the last 14 days. They also need to be advised on when they can safely end their home isolation.
(e) Necessary supplies- It is pertinent that adequate supplies to support healthy hygiene need to be ensured. Necessary Supplies include no-touch soap dispenser, hand sanitizer (atleast 60% alcohol), paper towels, tissues and no-touch disposal bins.
(f) Signs and awareness messages- Posting of signs-boards about various aspects like how to stop the spread, properly washing hands, how to maintain physical distancing, promoting everyday protective measures and messages on proper use of cloth face covering in commonly visiting locations like at deck entrances and at washing areas aids in better control of spread and awareness. Broadcasting regular announcements about how to stop the spread including messages about behaviors that prevent the spread of COVID-19 should be done. Promoting awareness using methods like emails, facility websites (e.g., posting online videos), through social media platforms and messages on entrance tickets can further help in reinforcing the behaviour pattern and may improve compliance to the preventive measures.
(g) Adult athletes may follow instructions for social distancing and other protective actions. However, for younger athletes, parents or other household members should monitor them and make sure that they follow the guidelines.
Resumption of Training: Screening Guidelines for Asymptomatic Athletes
All athletes resuming to sport should be subjected to standard protocol for COVID-19 testing. Clinicians (sports physicians) should use their clinical acumen to determine if an athlete has clinical signs and symptoms of COVID-19, which warrants testing for COVID-19. Asymptomatic infection has also been reported. However, most patients with confirmed COVID-19 have been found to develop fever and/or symptoms of acute respiratory illness. Epidemiological factors like occurrence of local community transmission may guide testing are of COVID-19 in a particular region [33-35]. It should be a routine for a coach or a staff member to ask about any health issues and closely monitor the sports persons. A high level of medical suspicion is needed.
Resumption of Training: Screening Guidelines for Athletes Post COVID-19 Infection
COVID-19 requires athletes to undergo medical evaluation after an infection prior to returning to competitive sport [36]. This appears logical, especially in light of the specific pulmonary and cardiac involvement [Table/Fig-1] [10,37,38].
Decisional algorithm for resumption of sport [10,37,38].
1=Return to play only after negative COVID-19 test + normal: physical examination, blood oxygen saturation and ECG. 2=Return to play only after negative COVID-19 test + normal: blood oxygen saturation, physical examination, rest and stress ECG (no clinically relevant arrhythmia), echocardiography, spirometry and neurological tests. 3=Return to play only after negative COVID-19 test + normal: blood oxygen saturation, physical examination, rest and stress ECG (no clinically relevant arrhythmia), Cardiopulmonary Exercise Testing (CPET), blood gas analysis, echocardiography, spirometry and neurological tests. 4=Return to play only after negative COVID-19 test + normal: blood oxygen saturation, physical examination, exercise testing (CPET), blood gas analysis, rest and stress ECG (no clinically relevant arrhythmia), systolic function in echocardiography, spirometry, neurological tests, and serum markers for myocardium damage, inflammation and heart failure
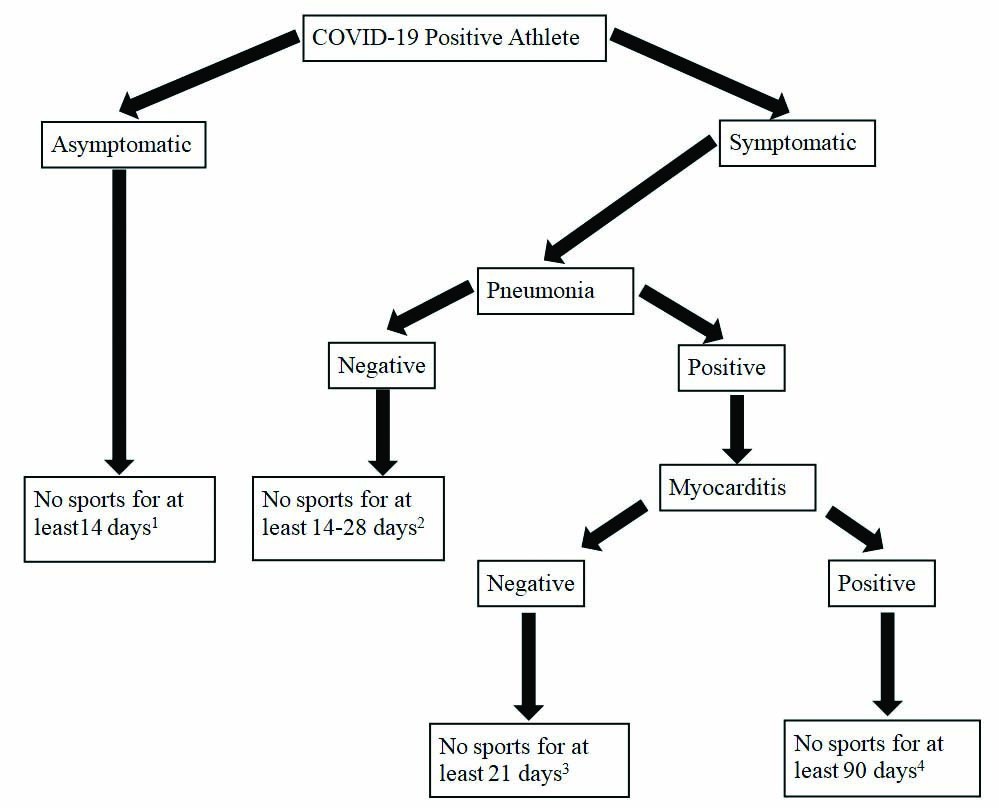
Due to a great variance in the course of COVID-19 infection, categorisation of the cases based on the clinical symptoms, pulmonary and cardiac findings [Table/Fig-2] seems logical in the decision concerning return-to-sport [10]. Depending on further symptoms, the decisional algorithm should be individually adapted.
| Cases | Categorisation |
|---|
| Suspected case | Shows Influenza Like Illness (ILI) without a conclusive COVID-19 positive result |
| Shows influenza like illness with H/O (history of) travel to country/area reporting local transmission |
| Shows influenza like illness with H/O contact with a confirmed case of COVID-19 |
| Confirmed case | Asymptomatic COVID-19 positive cases |
| Symptomatic COVID-19 positive cases with/without pneumonia |
| Severe COVID-19 positive cases with pneumonia with/without myocarditis |
A thorough history with respect to COVID-19 symptoms should be made at the time of determining sport eligibility. Both the history and the subsequent physical examination should be based on a standardised protocol. In addition to basic laboratory, additional laboratory as per the latest guidelines of international and national health/sports agencies should be determined depending on the case cluster.
Preventive Measures for Support Personnel
All general guidelines are mandatory for the support personnel.
(a) Coach and support staff:
(i) Ensure availability of facilities for hand washing, necessary supplies like alcohol-based hand gel at multiple locations within the event facility and accommodation.
(ii) Medical masks should be ready for use by the staff and medical professionals.
(iii) Ensure adequate rubber gloves to team staff and volunteers who handle laundry, towels, etc.
(b) Spectators:
(i) Physical distancing of spectators must be strictly followed if they are to be present during the training/competition.
(ii) Sports events should be conducted by maintaining the general norms of social distancing like widely spaced seats for maintaining physical distancing of at least 1.5 metre. Monitoring temperature at the entrance and providing visual reminders like stickers or wrist stamps may decrease incidental contact [39].
(iii) Tracking of the spectators during contact tracing can be made easy by pre online registration of passes and tickets for practice and competitions respectively [40]. These registrations should consist of spectator’s contact details and Identity Document (ID) proof with address on it. Manual registrations can also be done at the venue entrance.
(c) Venue medical officer:
(i) Designated First aid and trained medical officers who are able to triage and refer suspected cases for COVID-19 testing should be made available.
(ii) The medical staff should equip themselves with Personal Protective Equipment (PPE) or face shields, along with medical masks and gloves.
(iii) Temperature check of all staff/individuals need to be performed. Any individual with temperature above 38°C should be reported timely to the chief medical officer. Close watch should also be done for any other symptoms linked with COVID-19.
Swimming Facility Recommendations [
33]
(a) Cleaning and disinfection:
(i) Care to be taken to clean and disinfect all the frequently touched surfaces daily. Shared objects need to be disinfected each time they are used. Common items are handrails, lounge chairs, tabletops, kick boards, doorknobs, door handles, surfaces of restrooms, hand washing stations and showers.
(ii) Simple routine and adequate cleaning with soap and water can lower the spread of COVID-19. This would remove germs and dirt from surfaces. Hence, should be encouraged as much as possible.
(iii) Use of disinfectants would kill germs on the surfaces. Thus, use of disinfectant can further lower the risk of spreading infection. Disinfectants recommended by WHO should be used to reduce the risk of COVID-19 transmission. Alternative disinfectants which may be used include 70% alcohol solutions, or 1/3 cup of bleach added to 1 gallon of water. Disinfection done with the help of bleach solutions may last up to 24 hours.
(iv) It is advisable to not mix cleaning chemicals together. It is generally advised to adhere to the manufacturer’s guidelines.
(v) Furnitures like chairs, stools that need to be cleaned and disinfected should be kept separately.
(vi) To avoid confusion, containers for used equipments that have not yet been cleaned and disinfected should be labeled and need to be kept separately from those of cleaned equipments.
(vii) Once cleaning and disinfection of this shared furniture, equipments, towels and clothing are performed, it is also important to protect them from further contamination before use.
(viii) In addition, it is important to ensure safe and correct use as well as storage of disinfectants appropriately.
(b) Ventilation:
(i) Ensuring proper operation of ventilation systems of indoor spaces is essential.
(ii) Opening windows and doors, using fans, or other methods would further aid in promoting cross-ventilation by increasing circulation of outdoor air as much as possible.
(c) Modified layouts:
(i) Physical distancing norm of at least six feet has to be maintained in seating and standing areas for the spectators and staff.
(d) Physical barriers and guides:
(i) Even within the swimming pools, it is important to maintain 6 feet apart between lanes. To ensure this, providing physical cues or guides like lane lines in the water or chairs and tables on the deck, visual cues and signs need to be displayed.
(e) Shared objects:
(i) Educate people to avoid sharing items that come in contact with the face (e.g., goggles and snorkels) and difficult to sanitise or disinfect.
(ii) Discouraging the sharing of items such as food, equipments and supplies also to be promoted.
(f) Pool disinfection:
(i) Centre for Disease Control and Prevention (CDC) has recommended that in swimming pools the pH should be maintained between 7.2-7.8. The free chlorine concentration of at least 1 ppm in pools (ideally 2-4 ppm) has also been recommended.
(ii) Testing of free chlorine concentration must be routinely carried out because free chlorine may be used up by sunlight or used up in the process of breaking down urine, fecal material, sweat, and dirt from swimmers’ bodies instead of killing germs.
(iii) Testing of free chlorine concentration and pH should be carried out at least two times in a day and the same needs to be done more often if the pool is being used often.
(iii) Most of the bacteria especially E.coli gets killed by free chlorine in less than a minute. Hepatitis A virus gets killed in 16 minutes it may take between 45 mins and 11 days to kill some parasites.
(iv) Free chlorine and pH are measured using the N, N Diethyl-1, 4 Phenylenediamine Sulfate testing kit.
(g) Effective preventive measures:
(i) Routine cleaning and disinfecting should be done.
(ii) Surfaces frequently touched should be cleaned and disinfected at least daily.
(iii) Daily testing of the pool water for pH and free chlorine levels.
(iv) Maintaining a regular cleansing regime
(v) Following good public hygiene guidelines like take a shower before entering the pool and to not spit into the pool.
Continued Education and Awareness Program on COVID-19
An ongoing education program on the preventive measures of COVID-19 for the coaches, athletes and support staff is vital. This allows for the reinforcement of importance of hand hygiene, cough etiquette, physical distancing, wearing masks and staying home if sick. This helps in continued risk reduction of the pandemic. The coach can be a role model by wearing a face cloth/mask and encouraging athletes, parents, officials and sports staff to do the same during practices and games. The coach can provide hand sanitiser (70% alcohol) to these athletes before and after practice/game and emphasise on hand washing with soap. He/she can educate athletes about covering coughs and sneezes with their bent elbows and keep reminding them of physical distancing. The coach should keep himself/herself updated on COVID-19 through online programs. The facility management should keep educating the cleaning staff about all preventive measure while cleaning and disinfecting. A medical professional should be designated who conducts a weekly awareness program on the preventive measures of COVID-19.
Conclusion(s)
The broad aim of this study was to understand the natural history of COVID-19 and to formulate guidelines for resumption of sports specific to swimming in India. This study is one of the major attempts to have shed focus on the resumption of sport guidelines for Indian swimming athletes. In our study, we have adhered to the recommendations given by the CDC, WHO to formulate resumption of swimming guidelines. The evidence-based knowledge about the course of COVID-19 and guidelines for resumption of swimming reported here can be a key support for the coaches, athletes, support staff, aquatic facility managers/owners and medical professionals to reduce the risk of COVID-19 while safely resuming swimming.
[1]. Hughes D, Saw R, Perera NKP, Mooney M, Wallett A, Cooke J, The Australian Institute of Sport framework for rebooting sport in a COVID-19 environmentJ Sci Med Sport 2020 23(7):639-63.10.1016/j.jsams.2020.05.00432451268 [Google Scholar] [CrossRef] [PubMed]
[2]. Paoli A, Musumeci G, Elite athletes and COVID-19 lockdown: Future health concerns for an entire sectorJ Funct Morphol Kinesiol 2020 5(2):3010.3390/jfmk502003033467246 [Google Scholar] [CrossRef] [PubMed]
[3]. Mujika I, Padilla S, Detraining: loss of training-induced physiological and performance ad-aptations. Part IISports Med 2000 30(3):145-54.10.2165/00007256-200030030-0000110999420 [Google Scholar] [CrossRef] [PubMed]
[4]. Halabchi F, Ahmadinejad Z, Selk-Ghaffari M, COVID-19 epidemic: Exercise or not to exercise; That is the question!Asian J Sports Med 2020 11(1):e10263010.5812/asjsm.102630 [Google Scholar] [CrossRef]
[5]. Pradhan P, Pandey AK, Mishra A, Gupta P, Tripathi PK, Menon MB, Uncanny similarity of unique inserts in the 2019-nCoV spike protein to HIV-1 gp120 and GagBioRxiv 2020 :01-14.10.1101/2020.01.30.927871 [Google Scholar] [CrossRef]
[6]. Guan W, Ni Z, Hu Y, Liang W, Ou C, He J, Clinical characteristics of 2019 novel coronavirus infection in ChinaMedRxiv 2020 10.1056/NEJMoa200203232109013 [Google Scholar] [CrossRef] [PubMed]
[7]. Cucinotta D, Vanelli M, WHO declares COVID-19 a pandemicActa Bio-Medica Atenei Parm 2020 91(1):157-60. [Google Scholar]
[8]. La Rosa G, Bonadonna L, Lucentini L, Kenmoe S, Suffredini E, Coronavirus in water environments: Occurrence, persistence and concentration methods-A scoping reviewWater Res 2020 2020:11589910.1016/j.watres.2020.11589932361598 [Google Scholar] [CrossRef] [PubMed]
[9]. Wigginton KR, Ye Y, Ellenberg RM, Emerging investigators series: The source and fate of pandemic viruses in the urban water cycleEnviron Sci Water Res Technol 2015 1(6):735-46.10.1039/C5EW00125K [Google Scholar] [CrossRef]
[10]. Nieß AM, Bloch W, Friedmann-Bette B, Grim C, Halle M, Hirschmüller A, Position stand: Return to sport in the current coronavirus Pandemic 2020 10.5960/dzsm.2020.437 [Google Scholar] [CrossRef]
[11]. Ruan Q, Yang K, Wang W, Jiang L, Song J, Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, ChinaIntensive Care Med 2020 46(5):846-48.10.1007/s00134-020-05991-x32125452 [Google Scholar] [CrossRef] [PubMed]
[12]. Zhu J, Ji P, Pang J, Zhong Z, Li H, He C, Clinical characteristics of 3,062 COVID-19 patients: a meta-analysisJ Med Virol 2020 92(10):1902-14.10.1002/jmv.2588432293716 [Google Scholar] [CrossRef] [PubMed]
[13]. CDC. Coronavirus Disease 2019 (COVID-19) [Internet]. Centers for Disease Control and Prevention. 2020 [cited 2020 Jun 14]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html [Google Scholar]
[14]. Conti P, Ronconi G, Caraffa AL, Gallenga CE, Ross R, Frydas I, Induction of pro-inflammatory cytokines (IL-1 and IL-6) and lung inflammation by Coronavirus-19 (COVI-19 or SARS-CoV-2): Anti-inflammatory strategiesJ Biol Regul Homeost Agents 2020 34(2):1 [Google Scholar]
[15]. Ye Q, Wang B, Mao J, The pathogenesis and treatment of the ‘Cytokine Storm’ in COVID-19J Infect 2020 80(6):607-13.10.1016/j.jinf.2020.03.03732283152 [Google Scholar] [CrossRef] [PubMed]
[16]. Connors JM, Levy JH, COVID-19 and its implications for thrombosis and anticoagulationBlood J Am Soc Hematol 2020 135(23):2033-40.10.1182/blood.202000600032339221 [Google Scholar] [CrossRef] [PubMed]
[17]. Madjid M, Safavi-Naeini P, Solomon SD, Vardeny O, Potential effects of coronaviruses on the cardiovascular system: A reviewJAMA Cardiol 2020 5(7):831-40.10.1001/jamacardio.2020.128632219363 [Google Scholar] [CrossRef] [PubMed]
[18]. Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Endo-thelial cell infection and endotheliitis in COVID-19The Lancet 2020 395(10234):1417-18.10.1016/S0140-6736(20)30937-5 [Google Scholar] [CrossRef]
[19]. Bohm P, Scharhag J, Meyer T, Data from a nationwide registry on sports-related sudden cardiac deaths in GermanyEur J Prev Cardiol 2016 23(6):649-56.10.1177/204748731559408726130495 [Google Scholar] [CrossRef] [PubMed]
[20]. Cooper LT, MyocarditisN Engl J Med 2009 360(15):1526-38.10.1056/NEJMra080002819357408 [Google Scholar] [CrossRef] [PubMed]
[21]. Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen C, Neurologic features in severe SARS-CoV-2 infectionN Engl J Med 2020 382:2268-70.10.1056/NEJMc200859732294339 [Google Scholar] [CrossRef] [PubMed]
[22]. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Neurologic manifestations of hospital-ized patients with coronavirus disease 2019 in Wuhan, ChinaJAMA Neurol 2020 77(6):683-90.10.1001/jamaneurol.2020.112732275288 [Google Scholar] [CrossRef] [PubMed]
[23]. Toscano G, Palmerini F, Ravaglia S, Ruiz L, Invernizzi P, Cuzzoni MG, Guillain-Barré syndrome associated with SARS-CoV-2N Engl J Med 2020 382:2574-76.10.1056/NEJMc200919132302082 [Google Scholar] [CrossRef] [PubMed]
[24]. Borges do Nascimento IJ, Cacic N, Abdulazeem HM, von Groote TC, Jayarajah U, Weerasekara I, Novel Coronavirus Infection (COVID-19) in humans: A scoping review and meta-analysisJ Clin Med 2020 9(4)10.3390/jcm904094132235486 [Google Scholar] [CrossRef] [PubMed]
[25]. Sun P, Qie S, Liu Z, Ren J, Li K, Xi J, Clinical characteristics of hospitalized patients with SARS-CoV-2 infection: A single arm meta-analysisJ Med Virol 2020 92(6):612-17.10.1002/jmv.2573532108351 [Google Scholar] [CrossRef] [PubMed]
[26]. The impact of COVID-19 on sport, physical activity and well-being and its effects on social development | DISD [Internet]. [cited 2020 Jun 14]. Available from: https://www.un.org/development/desa/dspd/2020/05/covid-19-sport/ [Google Scholar]
[27]. Mujika I, Padilla S, Detraining: loss of training-induced physiological and performance ad-aptations. Part ISports Med 2000 30(2):79-87.10.2165/00007256-200030020-0000210966148 [Google Scholar] [CrossRef] [PubMed]
[28]. Kalkhoven JT, Watsford ML, Impellizzeri FM, A conceptual model and detailed framework for stress-related, strain-related, and overuse athletic injuryJ Sci Med Sport 2020 10.31236/osf.io/vzxga [Google Scholar] [CrossRef]
[29]. De Boer MD, Maganaris CN, Seynnes OR, Rennie MJ, Narici MV, Time course of muscular, neural and tendinous adaptations to 23 day unilateral lower-limb suspension in young menJ Physiol 2007 583(3):1079-91.10.1113/jphysiol.2007.13539217656438 [Google Scholar] [CrossRef] [PubMed]
[30]. Rejc E, Floreani M, Taboga P, Botter A, Toniolo L, Cancellara L, Loss of maximal explosive power of lower limbs after 2 weeks of disuse and incomplete recovery after re-training in older adultsJ Physiol 2018 596(4):647-65.10.1113/JP27477229266264 [Google Scholar] [CrossRef] [PubMed]
[31]. Publications, Data, & Statistics | Healthy Swimming | Healthy Water | CDC [Internet]. 2020 [cited 2020 Jun 14]. Available from: https://www.cdc.gov/healthywater/swimming/publications.html [Google Scholar]
[32]. Considerations for Public Pools, Hot Tubs, and Water Playgrounds During COVID-19 | CDC [Internet]. [cited 2020 Jun 14]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/parks-rec/aquatic-venues.html [Google Scholar]
[33]. CDC. Coronavirus Disease 2019 (COVID-19) [Internet]. Centers for Disease Control and Prevention. 2020 [cited 2020 Jun 14]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/testing-overview.html [Google Scholar]
[34]. Emergency Medical Relief | Ministry of Health and Family Welfare | GOI [Internet]. [cited 2020 Jun 14]. Available from: https://main.mohfw.gov.in/Organisation/Departments-of-Health-and-Family-Welfare/emergency-medical-relief [Google Scholar]
[35]. Standar Operating Procedure SOP fortr an sporting asuspector confirmed case of COVID19.pdf [Internet]. [cited 2020 Aug 3]. Available from: https://www.mohfw.gov.in/pdf/rd Operating Procedure SOP fortran sporting a suspector confirmed case of COVID19.pdf [Google Scholar]
[36]. Corsini A, Bisciotti GN, Eirale C, Volpi P, Football cannot restart soon during the COVID-19 emergency! A critical perspective from the Italian experience and a call for actionBr J Sports Med 2020 54(20):1186-87.10.1136/bjsports-2020-10230632209554 [Google Scholar] [CrossRef] [PubMed]
[37]. Maron BJ, Udelson JE, Bonow RO, Nishimura RA, Ackerman MJ, Estes NM, Eligi-bility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: Task force 3: Hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy and other cardiomyopathies, and myocarditis: a scientific statement from the American Heart Association and American College of CardiologyJ Am Coll Cardiol 2015 66(21):2362-71.10.1016/j.jacc.2015.09.03526542657 [Google Scholar] [CrossRef] [PubMed]
[38]. Pelliccia A, Solberg EE, Papadakis M, Adami PE, Biffi A, Caselli S, Recommenda-tions for participation in competitive and leisure time sport in athletes with cardio-myopathies, myocarditis, and pericarditis: Position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC)Eur Heart J 2019 40(1):19-33.10.1093/eurheartj/ehy73030561613 [Google Scholar] [CrossRef] [PubMed]
[39]. Organisation WH, Considerations for sports federations/sports event organisers when plan-ning mass gatherings in the context of COVID-19: Interim guidance, 14 April 2020World Health Organisation 2020 [Google Scholar]
[40]. Hassanzadeh-Rad A, Halabchi F, Stadiums as possible hot spots for COVID-19 spreadAsian J Sports Med 2020 11(2)10.5812/asjsm.103178 [Google Scholar] [CrossRef]