A Morphometric and Morphological Study on Dry Adult Cuboid Bones
Sreya Moitra1
1 Assistant Professor, Department of Anatomy, College of Medicine and Sagore Dutta Hospital, Kamarhati, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sreya Moitra, Assistant Professor, Department of Anatomy, College of Medicine and Sagore Dutta Hospital, Kamarhati, Kolkata, West Bengal, India. Address: C/O Dr. Arupratan Maiti, Jeet Tapoban, Block D, 665 Madurdaha, Kolkata-700107, India.
E-mail: moitrasreya@gmail.com
Introduction
Precise biometric data of cuboid and calcaneocuboid joint are not discussed very distinctly in the text books of Anatomy. A better knowledge of the joint surfaces of cuboid and biometric data would generate a three dimensional modeling of the calcaneocuboid joint and would help in the management of Cuboid Syndrome.
Aim
To study about morphological and morphometric analysis in adult dry cuboid bone.
Materials and Methods
This study was conducted in the Department of Anatomy of a Medical College using 60 dry cuboid bones from museum. Each bone was observed for its morphometric analysis as well as its pattern of calcaneal and metatarsal articular facets. Results were statistically analysed using the Statistical Package for the Social Sciences (SPSS) software, version 19. Students t-test was applied to find the difference between the mean values of the parameters.
Results
Mean medial length of cuboid was 33.41 mm, lateral length was 19.73 mm, height was 26.17 mm, length index was 169.33, vertical and transverse diameters of calcaneal articular facet were 24.24 mm and 16.45 mm respectively, vertical and transverse diameters of metatarsal articular facet were 21.32 mm and 13.85 mm respectively, depth of peroneal groove was 0.63mm. Concavo-convex facet with posteromedial projection and oval or reniform in shape (Type 1A) was the most common calcaneal articular facet and convex pattern was the most common metatarsal articular facet of cuboid.
Conclusion
Morphological characterisation of articular facet of cuboid and its morphometric analysis help to understand the degree of movement at calcaneocuboid joint, its associated pathologies and instabilities.
Biometric values of cuboid, Calcaneal facet, Calcaneocuboid joint pathologies, Metatarsal facet, Tarsal bones
Introduction
The cuboid bone is present on lateral side in distal row of tarsal bone which is cuboid shaped with smooth articular surfaces where the other bones connect and are held together by ligaments and tendons. In front, it articulates with the bases of fourth and fifth metatarsal bones and behind with the calcaneus (heel bone) which is called calcaneocuboid joint. This is an important joint for stability, load transfer, and movement of foot and ankle [1-3]. The joints formed by cuboid bone and stabilised by the ligaments are as follows: calcaneocuboid, cuboideo-navicular, cuboideo-metatarsal, and long plantar ligaments along with tibialis posterior tendon [4].
The transverse tarsal (Chopart) joints include talonavicular and the calcaneocuboid joints. Isolated dislocations of transverse tarsal joints are rare due to strong periarticular ligamentous structural support. The inferior calcaneocuboid ligament, calcaneonavicular (spring) ligament, and bifurcate ligament all confer stability to the transverse tarsal joints and are important to support of the foot arch. For this reason, dislocations in the dorsal direction are infrequent, requiring disruption of these plantar ligaments. Among tarsometatarsal joints (Lisfranc’s joint) cuboid articulating with fourth and fifth metatarsals provide necessary gliding and adjustment during walking on uneven surface. Morphological variation in pattern of metatarsal articulating surface is important in understanding joint stability and factors disrupting it. On the plantar surface, the cuboid is divided by an oblique ridge further into an anterior grooved part (peroneal groove) and a posterior sloping part. From this anterior groove (osseo fibrous tunnel), Peroneus Longus tendon will transmit [5,6]. A shift in the position of the cuboid bone can cause loss of motion with the bone ‘locked’ in place. The surfaces of the connecting bones no longer line up which means the joint has lost its congruence. It causes pain along the lateral (outside) edge of the foot. This effect with the accompanying symptoms is a Cuboid Syndrome. Other names are Cuboid Fault Syndrome, Dropped Cuboid, Sublaxed Cuboid, Locked Cuboid, Peroneal Cuboid Syndrome and Lateral Plantar Neuritis [7].
Cuboid Squeeze or Cuboid Whip is a treatment with the manipulation of bones. The process is like, the physical therapist by applying the force on the specific area shift the bone back to its normal position in the affected foot. The patient may feel and/or hear a click or pop. Immediate pain relief is often reported after manipulation but sometimes it may take more than one manipulation to completely resolve the problem [8]. The treatment and management of cuboid syndrome is based on good knowledge of the articular surfaces supported by analysis of different biometric data of the cuboid in a systematic manner. Also, this is important for surgeries of midfoot region and in isolated cuboid fractures. Various authors have studied morphology of different tarsal bones especially talus and calcaneum but there are very scanty studies reported on cuboid throughout the world [9-13]. Hence, this study was undertaken to report the morphometric data of cuboid and to evaluate its morphological variation of calcaneal articular facet and metatarsal articular facet.
Materials and Methods
This was an observational cross-sectional study for a period of approximately six months from May 2020 to October 2020. Sixty dry adult cuboid bones, 30 of right and 30 of left foot of unknown sex from the museum of the Department of Anatomy which were kept and preserved for academic purposes were used for study. Any cuboid bone with pathological concern found on general examination was excluded from the study. Approval from the Institutional Technical Advisory Committee and Ethics Committee was obtained (vide memo no. CMSDH/IEC/170/09-2020 dated 12.10.2020). The side of the bones was determined. Then each bone was numbered and measured using sliding vernier calipers (with minimum calibration length 0.1 mm). Also, the outline of the calcaneal articular facet and the metatarsal articular facet were marked, grouped and classified. The present study was greatly indebted to the study conducted by Viveka S and Kumar SS [9]. Since, there is no standardised classification for pattern of calcaneal and metatarsal articular facets of cuboid, the classification followed by them in their study was applied as per convenience in this study. Then the following parameters were studied:
1) Medial length: Straight distance between the most proximal and the most distally placed point on the medial margin of cuboid.
2) Lateral length: Straight distance between the most proximal and the most distally placed point on the lateral margin of cuboid.
3) Cuboid height: Maximum distance of the dorsal upper surface from plantar margin of cuboid tuberosity.
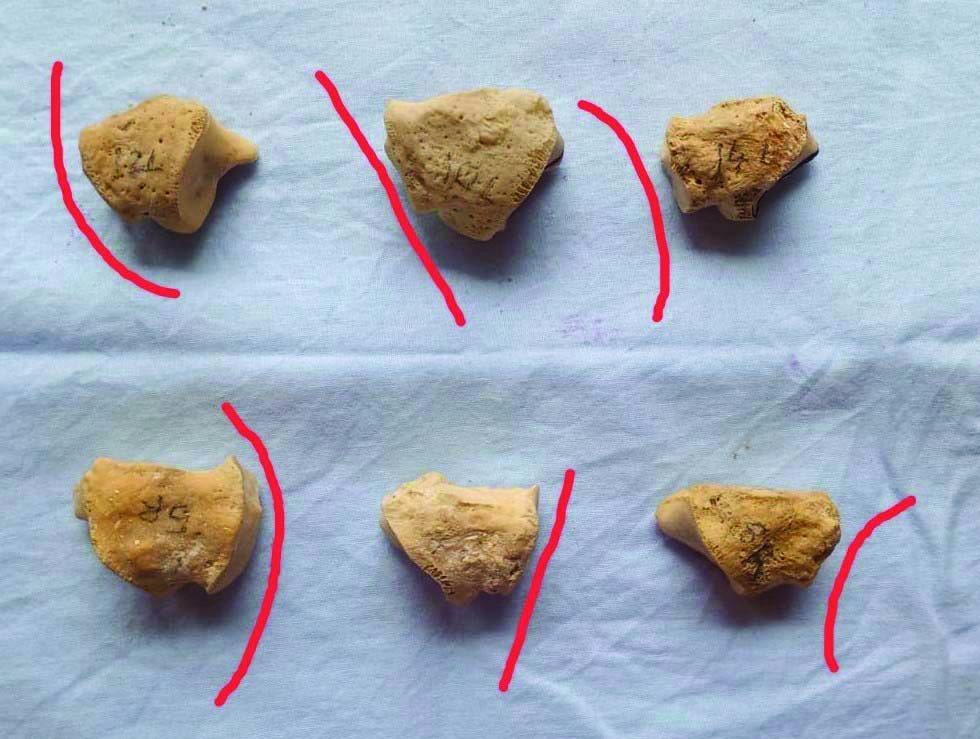
4) Peroneal groove depth: Maximum distance between the deepest point in the depression and a horizontal line drawn from the lower edge of metatarsal articulating facet from the lateral profile [Table/Fig-1].
5) Length index: A ratio obtained as Medial Length/Lateral Length x100.
6) The greatest vertical and transverse diameters of both calcaneal and metatarsal articular facet.
Lateral view of left cuboid (upper one) and right cuboid (lower one) showing depth of peroneal groove.

Statistical Analysis
The left and right side values of all the parameters considered were tabulated separately and were compared for statistical difference. Students t-test was applied to find the difference between the mean values of the above parameters among the two groups (right side and left side). The p-values <0.05 were considered as significant. Results were statistically analysed using the SPSS software, version 19.
Results
Pattern of calcaneal articular facet has been depicted in [Table/Fig-2,3].
Pattern of calcaneal articular facet- Type 1a, 1b, 2a, 2b of left cuboid (posterior view) from left to right.
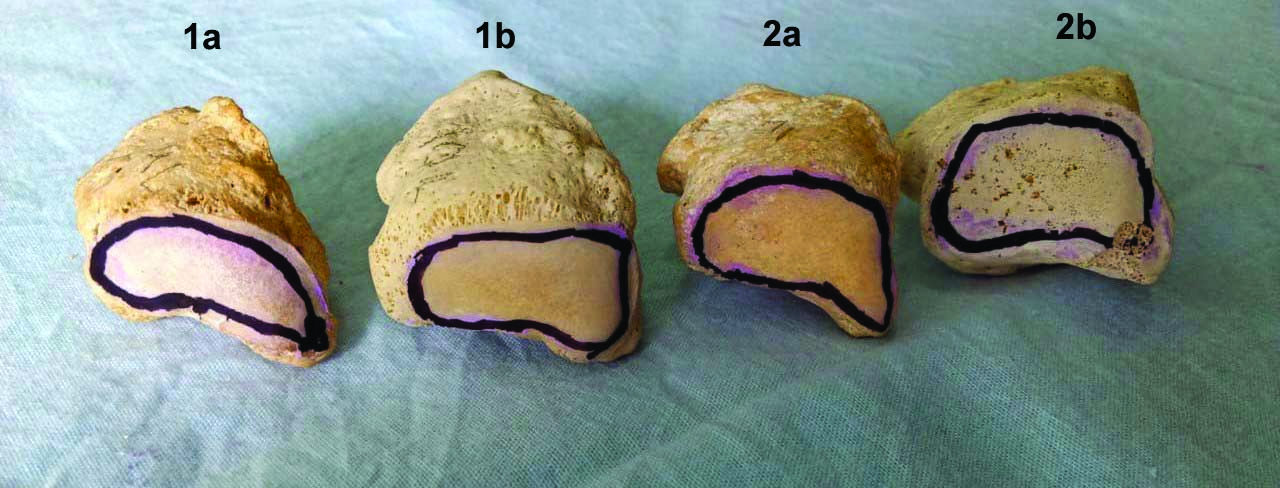
Pattern of calcaneal articular facet- Type 1a, 1b, 2a, 2b of right cuboid (posterior view) from left to right.
1a: Concavoconvex facet with posteromedial projection and oval or reniform shaped.
1b: Concavoconvex facet without posteromedial projection and rectangular shaped.
2a: Plane facet with posteromedial projection and oval or reniform shaped.
2d: Plane facet without posteromedial projection and rectangular shaped.
In this study, it was found that Type 1a was the most common calcaneal articular facet of cuboid and the combined percentage of both right and left sides were 38% [Table/Fig-4].
Percentage and frequencies of different types of calcaneal facets.
| Types | Frequency | Total no. of cuboid | Percentage |
|---|
| Right | Left |
|---|
| 1a | 11 | 12 | 23 | 38 |
| 1b | 6 | 7 | 13 | 22 |
| 2a | 7 | 6 | 13 | 22 |
| 2b | 6 | 5 | 11 | 18 |
| Total | 30 | 30 | 60 | 100 |
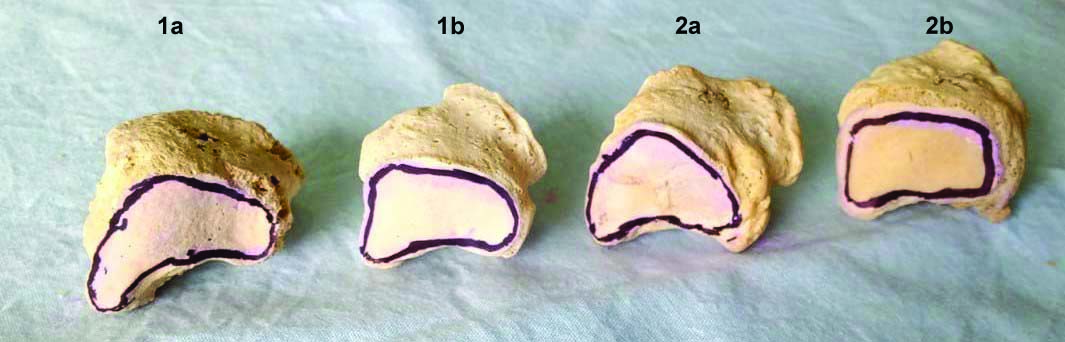
Pattern of metatarsal articular facet has been depicted in [Table/Fig-5].
Pattern of metatarsal articular facet from left to right-convex, plane and concave of left cuboid (upper row) and right cuboid (lower row).
Concave: Edges of metatarsal articulating facet projected anteriorly making a depression for articulation with the bases of fourth and fifth metatarsals.
Plane: Articular facet is flat.
Convex: Articular surface slopes posteriorly.
In this study, it was found that convex pattern was the most common metatarsal articular facet of cuboid and the combined percentage of both right and left sides were 53% [Table/Fig-6].
Percentage and frequencies of different types of metatarsal articular facets.
| Types | Frequency | Total no. of cuboid | Percentage |
|---|
| Right | Left |
|---|
| Concave | 6 | 5 | 11 | 18 |
| Plane | 8 | 9 | 17 | 28 |
| Convex | 16 | 16 | 32 | 53 |
| Total | 30 | 30 | 60 | 100 |
In the present study, the mean (combined values of both right and left side) medial length of cuboid was found to be 33.41 mm and the lateral length was 19.73 mm, length index was 169.33, height was 26.17 mm, depth of peroneal groove was 0.636 mm, vertical and transverse diameter of calcaneal facet were 24.24 mm and 16.45 mm, vertical and transverse diameter of metatarsal facet were 21.32 mm and 13.85 mm, respectively. Difference between left and right side of cuboid bone were not clinically significant as the p-value of all the parameters were >0.05 [Table/Fig-7].
Morphometric values on cuboid of both right and left sides with their p-values.
| Parameters | Minimum diameter | Maximum diameter | Range | Mean | Standard deviation | p-value* |
|---|
| Medial length (mm) | 29.2 | 39.2 | 10 | 33.41 | 2.442 | 0.676 |
| Lateral length (mm) | 16.9 | 24.75 | 7.85 | 19.73 | 1.803 | 0.145 |
| Length index | | | | 169.33 | | |
| Height (mm) | 22.4 | 30.65 | 8.25 | 26.17 | 2.061 | 0.420 |
| Peroneal groove depth (mm) | 0.32 | 1.025 | 0.705 | 0.636 | 0.186 | 0.161 |
| Vertical diameter of calcaneal facet (mm) | 19.65 | 28.45 | 8.8 | 24.24 | 2.190 | 0.231 |
| Transverse diameter of calcaneal facet (mm) | 13 | 20.35 | 7.35 | 16.45 | 1.640 | 0.965 |
| Vertical diameter of metatarsal facet (mm) | 17.85 | 26.7 | 8.85 | 21.32 | 2.189 | 0.083 |
| Transverse diameter of metatarsal facet (mm) | 11.1 | 17.15 | 6.05 | 13.85 | 1.422 | 0.706 |
*Students t-test was applied. Level of Significance ≤0.05
Discussion
Data on morphological and morphometric variations of cuboid bone on literature search was found to be limited on thorough literature search. The morphometric data in the present study reflects the biometric values reported by the study of Viveka S and Kumar SS except metatarsal articular pattern [9]. Type 1 was most common calcaneal articular facet and convex pattern was most common metatarsal articular facet which was in contrast to this study [Table/Fig-8] [9,11-16]. They also stated that these classifications provide rational basis for understanding calcaneocuboid joint stability. Type 1a with posteromedial projection provides deeper and congruent saddle surface for articulating with calcaneum where as Type 2b makes the joint relatively unstable. However, Ehlers-Danlos Syndrome and trauma can result in calcaneocuboid joint instability, variations in articulating facets may also significantly contribute to this condition [10].
Morphometric values on cuboid of both right and left sides with their p-values [9,11-16].
| Authors of the study (year) | No. of bones studied | Findings |
|---|
| Present Study (2020) | This observational cross-sectional study was performed on 60 dry cuboid bones of both sides and of unknown sex from the museum. | Mean medial length was 33.41 mm, lateral length was 19.73 mm, height was 26.17 mm, length index was 169.33, vertical and transverse diameter of calcaneal facet were 24.24 mm and 16.45 mm, respectively, vertical and transverse diameter of metatarsal facet were 21.32 mm and 13.85 mm, respectively, depth of peroneal groove was 0.636 mm. Type 1a and convex pattern were the most common calcaneal and metatarsal facets, respectively. |
| Viveka S and Kumar SS (2017) [9] | This study was conducted on 24 dry cuboid bones. | Mean medial length was 33.9 (±3.3) mm, lateral length was 17.9 (±1.6) mm, height was 22 (±1.5) mm, length index was 188.8, area of calcaneal and metatarsal articular facets were 124.9 (±10.9) mm2 and 91.9 (±5.7) mm2, depth of peroneal groove was 1.83 (±1.3) mm. Type1 and concave pattern were the most common calcaneal and metatarsal articular facets respectively. They concluded that the degree of movement at calcaneocuboid joint as well as the joint pathologies can be understood more by studying the patterns of the articular surfaces of the cuboid. |
| Archana Rao K et al., (2016) [11] | The study was performed on 53 dry adult human calcanei. | The cuboidal articular facet on calcaneus was grouped into 4 types: type 1=wedge, type 2=transverse oval, type 3=irregular, type 4=vertically oval as:Type 1 was the commonest with 54.7%, least was type 4 with 5.4%. |
| Kori D et al., (2016) [12] | The study was conducted on 600 dry calcanei of unknown sex and age. | The calcanei were classified into 5 types. Type 1=fusion of middle and anterior facets was predominant-73.9%, followed by type 2=anterior and middle facets were separate-21.5%. Total incidence of calcaneal spur was 17.7% of which 35% were dorsal spurs, 60.4% were plantar spurs while 4 bear both dorsal and plantar spurs. These spurs were found predominantly in Type1 calcanei, Type 3 and 4 did not exhibit dorsal and plantar spurs. |
| Prakash KG and Viveka S (2016) [13] | 34 dry human calcaneum bones were studied. | Type 1 was the most common talar articular facet (25 out of 34). Medial tubercular enthesophytes were most common type of abnormal bony outgrowths found in 21 bones (61.7%). Mean surface area of cuboidal articular facet was 386(±46)sq mm. The knowledge about these variations is important for surgeries of subtalar region. |
| Nagar SK et al., (2012) [14] | 529 calcanei of unknown sex in Gujarat state were studied. | It was found that in 3.67% of calcanei, the anterior and middle talar facets were continuous with each other and in 23.3% calcanei these two facets were separate from each other. In 1.13% calcanei the anterior facet was absent. It also showed racial similarities and differences which served as a prelude for biomechanics of foot. |
| Mini MP et al., (2012) [15] | 50 adult human calcanei were obtained irrespective of age and sex and were evaluated one by one. | Out of 50 calcanei, regarding the patterns of the talar facets, 13 were of TypeA (26%), 37 were of TypeB (74%) and none were of Type C. The mean intersecting angle of TypeA calcaneum was 121.50 and that of TypeB calcaneum was 151.60. The study revealed that the talar facet configuration of calcanei and the angle between anterior and middle facet influenced the stability of the subtalar joint. |
| Bonnel F et al., (2011) [16] | 40 taluses and 35 naviculars (dry, adult bones) of unknown sex were examined from the anatomy laboratory. | The inclination angle showed two main types of talus, one is more frequent with a mean angle of 115 degrees and the other is less frequent with a mean angle of 95 degrees. Also, three types of talus were demonstrated with the declination angle and for torsion. For talus, the surface pattern and radius of curvature along main axis were 40±(33-48)mm and 16±(15-18)mm, respectively. For navicular, the surface pattern and the radius of curvature along main axis were 28±4(24-32)mm and 23±4(19-25)mm, respectively. Out of 70 anatomic specimens mean length of talus was 6.12±0.27 cm and width was 4.26±0.31 cm. For calcaneus the mean length was 8.8±0.10 cm and width was 3.2±0.10 cm. These biometric values can be used as a comparative research with the values of other tarsal bones and thus provide logical classification of different foot pathologies. |
*Students t-test was applied. Level of Significance ≤0.05
Melinska AU et al., collected computed tomography data sets from 30 male subjects aged 17 to 63 years with no known foot pathology for developing statistical shape models for cuboid, navicular and talus [17]. They did the following steps: Image preprocessing, Contour extraction, 3D point cloud to surface, Land-marking, Averaging feature position and orientation, Spherical harmonics (SPHARM) decomposition, Model and model order selection. High sensitivity and specificity greater than 0.98 were found for all the considered bones based on parametric spherical harmonics representation. Sensitivity and specificity for calcaneus was 0.9600 and 0.9953, for cuboid 0.9960 and 0.9878, for navicular 1 and 0.9996, and for talus 0.9793 and 0.9958, respectively.
Seldom any case reports were found on calcaneocuboid joint dislocation and isolated cuboid injury. Analysing the reports which were found, emphasis, on the relevant anatomy and morphological variations of cuboid was made. However, no such strong conclusion can be drawn from these reports on the biometric values of the said bone [18-23].
Limitation(s)
In the present study, medial length of cuboid was taken as the straight distance between the most proximal and the most distally placed point on its medial margin. But this measurement does not correspond to the long axis of the cuboid bone anatomically. Again, the height of the cuboid was considered as the maximum distance of the dorsal upper surface from the plantar margin of the cuboid tuberosity which in maximum cases is the peroneal tubercle. The morphometric study of cuboid would have been more complete, if some more parameters like variations in number, position, shape and area of navicular and cuneiform articular facets, peroneal tubercle etc., were considered.
Conclusion(s)
Evidence based guidelines for the diagnosis and management of Cuboid Syndrome do not exist clearly. So, further research is needed in this area. It is a well-known fact that the cuboid syndrome is common among the dancers and the athletes. As such, it would be beneficial for all of us to be aware of the potential risk factors for the success or failure of the manipulation technique of the bone before application of the same. Further studies are recommended on corresponding cuboidal facets of calcaneum and fourth and fifth metatarsals in articulated foot, age and sex related changes on cuboid morphometry and midtarsal joint mechanics and movements. Also, variations of calcaneocuboid and other corresponding ligaments can be studied by cadaveric dissections to get a complete picture of cuboid evaluation. Along with these, radiological study will be more effective especially in cuboid syndrome subjects.
*Students t-test was applied. Level of Significance ≤0.05
*Students t-test was applied. Level of Significance ≤0.05
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 19, 2020
Manual Googling: Dec 02, 2020
iThenticate Software: Dec 19, 2020 (12%)
[1]. Bonnel F, Teisser P, Colombier JA, Toullec E, Assi C, Biometry of the calcaneocuboid joint: biomechanical implicationsFoot Ankle Surg 2013 19(2):70-75.10.1016/j.fas.2012.12.00123548445 [Google Scholar] [CrossRef] [PubMed]
[2]. Gray H, Anatomy of the Human Body 1918 20th edPhiladelphiaLea & Febiger [Google Scholar]
[3]. Datta AK, Essentials of Human Osteology 1997 4th edCurrent Books International:216 [Google Scholar]
[4]. Gill M, Vilella RC, Anatomy, Bony Pelvis and Lower Limb, Foot Cuboid Bone. [Updated 2020 Jul31]In: StatPearls[Internet]Treasure Island (FL)StatPearls [Google Scholar]
[5]. Harris AP, Johnson J, Waryasz GR, Isolated dorsal dislocations of the talonavicular and calcaneocuboid articulations (Chopart joints) from a low-energy mechanismAm J Emerg Med 2016 34(8):1733.e1-4.10.1016/j.ajem.2015.12.05426809661 [Google Scholar] [CrossRef] [PubMed]
[6]. Chen J, Sagoo N, Panchbhavi VK, The Lisfranc Injury: A literature review of anatomy, etiology, evaluation and managementFoot and Ankle Specialist[cited 2020 Aug 20]; Available from: https://doi.org/10.1177/193864002095013310.1177/193864002095013332819164 [Google Scholar] [CrossRef] [PubMed]
[7]. Durall CJ, Examination and treatment of Cuboid Syndrome: A literature reviewSports Health 2011 3(6):514-19.10.1177/194173811140596523016051 [Google Scholar] [CrossRef] [PubMed]
[8]. Jennings J, Davies GJ, Treatment of Cuboid Syndrome secondary to lateral ankle sprain: A case seriesJournal of Orthopaedics and Sports Physical Therapy 2005 35(7):409-41.10.2519/jospt.2005.35.7.40916108581 [Google Scholar] [CrossRef] [PubMed]
[9]. Viveka S, Kumar SS, Morphological and morphometric features of cuboid boneNational Journal of Clinical Anatomy 2017 6(3):273-79.10.4103/2277-4025.298226 [Google Scholar] [CrossRef]
[10]. Wainwright AM, Parmar HV, Gregg PJ, Calcaneocuboid dislocation in a case of Ehlers- Danlos syndromeInjury 1993 24(4):27410.1016/0020-1383(93)90188-C [Google Scholar] [CrossRef]
[11]. Archana Rao K, Jyothi KC, Shetty S, Morphometrical study of cuboidal articular facet of the human calcaneus bone and its clinical implicationsInt J Anat Res 2016 4(3.2):2652-55.10.16965/ijar.2016.284 [Google Scholar] [CrossRef]
[12]. Kori D, Prasad G, Rani A, Dewan RK, Singh R, Singh P, Study of variations in talar articular facets of human calcanei and their association with calcaneal spurs in North Indian populationInt J Anat Res 2016 4(3):2710-16.10.16965/ijar.2016.313 [Google Scholar] [CrossRef]
[13]. Prakash KG, Viveka S, Morphometric considerations of articular surfaces of calcaneum, occurrence of enthesophytes and evolutionary significance of cuboidal facetIndian J Clin Anat Physiol 2016 3(1):61-64.10.5958/2394-2126.2016.00016.5 [Google Scholar] [CrossRef]
[14]. Nagar SK, Ojaswini M, Dharati K, Gosai SR, Andani RH, Patel B, Types of talar articular facets and morphometric measurements of the human calcaneus boneNational Journal of Medical Research 2012 2(2):4995 [Google Scholar]
[15]. Mini MP, Silotry N, Haritha KN, Morphological study on patterns of talar articular facets of human calcaneiInternational Journal of Medical and Clinical Research 2012 3(3):136-39.10.9735/0976-5530.3.3.136-139 [Google Scholar] [CrossRef]
[16]. Bonnel F, Teisser P, Maestro M, Ferre B, Toullec E, Biometry of bone components in the talonavicular joint: A cadaver studyOrthopaedics and Traumatology: Surgery and Research 2011 97(6):S66-73.10.1016/j.otsr.2011.06.00521807576 [Google Scholar] [CrossRef] [PubMed]
[17]. Melinska AU, Romaszkiewicz P, Wagel J, Antosik B, Sasiadek M, Iskander DR, Statistical shape models of cuboid, navicular and talus bonesJ Foot Ankle Res 2017 10:610.1186/s13047-016-0178-x28163787 [Google Scholar] [CrossRef] [PubMed]
[18]. Bojsen Moller F, Calcaneocuboid joint and stability of the longitudinal arch of the foot at high and low gear push offJ Anat 1979 129(1):165-76. [Google Scholar]
[19]. Yu G, Yu T, Yang Y, Yuan F, Old nutcracker fracture of cuboidIndian J Orthop 2013 47(3):310-12.10.4103/0019-5413.11151323798765 [Google Scholar] [CrossRef] [PubMed]
[20]. Buckley R, Displaced isolated Cuboid fracturesClin Res Foot Ankle 2016 4(180):210.4172/2329-910X.1000180 [Google Scholar] [CrossRef]
[21]. Kamiya T, Watnabe K, Teramoto A, Yamashita T, Cuboid-navicular tarsal coalitionin an adolescent femaleathleteJBJS Case Connect 2015 5(4):e9310.2106/JBJS.CC.O.0000229252799 [Google Scholar] [CrossRef] [PubMed]
[22]. Awan O, Graham JA, The rare cuboid navicular coalition presenting as chronic foot painCase Reports Radiol 2015 285:e62510.1155/2015/62528525688320 [Google Scholar] [CrossRef] [PubMed]
[23]. Yildirim Y, Ergun S, Ankgulle AH, Cansu E, Calcaneocuboid joint dislocation: A case reportJ Am Podiatr Med Assoc 2014 104(6):644-48.10.7547/8750-7315-104.6.64425514277 [Google Scholar] [CrossRef] [PubMed]