Unanticipated difficult airway, inadvertant extubation of a difficult airway intraoperatively have been faced by all anaesthesiologists and are important causes of airway related morbidity and mortality [1]. American Society of Anaesthesiologists (ASA) recommend use of a Supraglottic Airway Devices (SGD) as a rescue ventilatory device in patients who cannot be intubated and ventilated conventionally. They also recommend SGD as a conduit for facilitating tracheal intubation [2]. Difficult Airway Society 2015 guidelines in adults have suggested using second generation supraglottic devices for unanticipated difficult airway situations due to less risk of aspiration and higher oropharyngeal leak pressure as compared to first generation SGD. This gives an anaesthetist more unhurried time to plan further steps carefully while the patient is being oxygenated and ventilated with minimal risk of aspiration [3].
In an emergency situation, effective airway should be established quickly to prevent hypoxia. It takes just 20-40 seconds for percentage saturation of haemoglobin with oxygen (SpO2) to fall from 80% to 40% [4]. Thus, it is of immense benefit to simulate a difficult airway scenario and identify before hand which supraglottic device would be able to establish airway successfully in minimum time in a real difficult airway scenario. Patients with cervical spine trauma with cervical spine immobilisation and burn contracture neck have difficult airway due to limited mouth opening, restricted head and neck movements and limited subluxation of the mandible [5]. This difficult airway scenario can be simulated using an extrication neck collar.
In an unfolding emergency scenario, the chance of successful insertion of a device improves with the experience of the operator with the device. LMA Supreme and i-gel are the two such second generation SGDs which have large scale studies and meta-analysis in adults with normal airways on them but very few studies comparing them in a difficult airway scenario [6-8]. An i-gel (Intersurgical ltd, Berkshire, UK) has a noninflatable cuff and is made-up of thermoelastic polymer. It has a rigid bite block and an oesophageal bent through which gastric tube can be passed. It can be used as a conduit for intubation due to presence of a wide airway tube [6]. LMA Supreme (LMA-S, Teleflex Incorporated, U.S.) is made up of polyvinyl chloride. It has an inflatable cuff, a reinforced tip, a semi rigid anatomically shaped airway tube and an oesophageal drain tube. Their potential advantages include easy insertion, high oropharyngeal leak pressure and airway protection [6].
A study showed that the LMA Supreme took significantly shorter time for insertion as compared to i-gel in spontaneously breathing anaesthetised patients with simulated difficult airway [9]. Hence, it was hypothesised that i-gel airway with its bulky cuff may be more difficult to insert in patients and will take longer time for successful insertion as compared to LMA Supreme in patients with simulated difficult airway undergoing general anaesthesia with controlled ventilation. Therefore in this study, evaluation and comparison of efficacy of i-gel and LMA supreme as ventilatory devices was done, in anaesthetised and paralysed patients with simulated difficult airway undergoing elective surgery. Primary outcome was time taken for successful insertion of device. Secondary outcomes were the number of attempts taken for insertion of device, oropharyngeal leak pressure, ease of gastric catheter insertion and fibreoptic bronchoscopic view of anatomical alignment of device with glottic opening.
Materials and Methods
The randomised controlled study was conducted in the Department of Anaesthesia and Intensive care from June 2016 to December 2016 after obtaining approval from the Institute Ethics committee (IEC/VMMC/SJH/Thesis/June-2015/598). It was registered with the Clinical Trail Registry of India (CTRI/2018/10/015901). A written informed consent was taken from all the patients included in the study.
The study included 180 adult patients of ASA physical status I and II, between age group of 18 to 65 years and weighing 30 to 70 kg. Any patient with BMI >30 kg/m2, difficult airway, mouth opening <4 cm, cervical spine pathology, intestinal and oesophageal pathology, pregnancy and surgeries done under spontaneous respiration were excluded from the study.
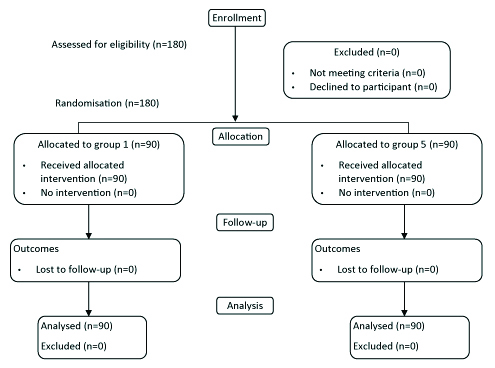
Block randomisation in series of blocks of ten was done to allocate patients to two groups based on sealed envelope method. In group I: i-gel was inserted (n=90) and in group S: LMA-supreme was inserted (n=90) [Table/Fig-1].
All the patients were made to fast as per standard ASA fasting guidelines and given antiaspiration and antianxiety prophylaxis. An extrication cervical collar (Stifneck select collar, Laerdal, Germany) was adjusted to proper size as per manufacturer’s instructions and kept ready for later application (size determined by finger sizing method with head of the patient in neutral position while sitting). Patient was made to lie supine on the operation table with a pillow of 5 cm height under the head. After attaching the standard monitors basal heart rate, noninvasive blood pressure (systolic, diastolic and mean) and SpO2 were noted.
Intravenous line was established and midazolam 0.02 mg/kg and glycopyrrolate 0.2 mg were given intravenously. Patients were preoxygenated for 3 minutes with 100% oxygen. Anaesthesia was induced with intravenous fentanyl 2 μg/kg body weight and propofol 2-2.5 mg/kg body weight intravenously. After checking ventilation, vecuronium bromide 0.1 mg/kg body weight was given intravenously to achieve neuromuscular blockade. Face mask ventilation was done with 100% oxygen and isoflurane (1-1.5%). After 1 minute of face mask ventilation, the extrication cervical collar [Table/Fig-2] with adjusted size was tied on the neck of the patient maintaining the head in the neutral position. Face mask ventilation was continued with the collar in place. Patient’s mouth was opened by the anaesthesiologist with two fingers and inter-incisor distance was measured with a measuring tape after 3 minutes of ventilation. After another 30 seconds of mask ventilation, in group I, i-gel of appropriate size was inserted and in group S, LMA-S of appropriate size was inserted as per manufacturer’s instructions, but in neutral position of head [10,11]. Size 3 of both i-gel and LMA-S was used for patients weighing 30-50 Kg and Size 4 of both devices was inserted in patients weighing 51-70 kg. After placement, the cuff of LMA supreme was inflated with air, to measure 60 cm of water using cuff pressure gauge (Covidien, Germany) and maintained at this pressure throughout anaesthesia. An i-gel has noninflatable cuff and did not need inflation. Airway tube of the used device was connected to closed circuit.
Picture of extrication collar used for the study.

Effective ventilation was said to be present, if there was bilateral symmetrical chest movements, bilateral equal air entry on auscultation, square wave form tracing on capnograph and lack of gastric insufflation during manual ventilation. The time taken for effective insertion of the device was noted. Any manipulations of the device required to optimise ventilation were noted.
Gastric catheter was passed though the gastric vent tube and its correct placement was confirmed by detection of injected air on epigastric auscultation. The device was secured in place by taping it over patient’s maxillae.
In case of failure of insertion of device or a significant audible air leak with ineffective ventilation, device was removed and reinsertion with same size device was attempted. The attempt where device had to be removed was taken as failed attempt of insertion. Three failed attempts of insertion were considered as failure of device. An attempt was to be aborted, if SpO2 fell below 92% and time to raise SpO2 to 100% with mask ventilation was to be included in total time for successful insertion. In case of failure of device, airway was secured after removal of extrication collar. Haemodynamic parameters were monitored till end of surgery.
The patient was ventilated on volume controlled mode of ventilation on anaesthesia work station using closed circuit breathing system with soda lime maintaining EtCO2 of 30-35 mmHg. Ventilatory parameters like inspiratory and expiratory tidal volume, EtCO2 and peak airway pressure were monitored. Oropharyngeal leak pressure was measured in the manual ventilation mode at fixed gas flow of 3 lt/min, by closing the circle system’s expiratory valve and noting the airway pressure at which equilibrium was reached (max 40 cm H2O allowed) [12].
Anatomical alignment of the device was assessed by passing a paediatric fiberoptic bronchoscope through the airway port and glottic view was graded keeping its tip just inside the distal end of airway tube. Extrication collar was removed within 10 minutes of insertion of device. Anaesthesia was maintained with N2O (67%, O2 33%), isoflurane (0.6-0.8%) and vecuronium bromide supplements, as and when required. At the end of surgery, patient was reversed using 100% oxygen, intravenous neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg. SGD was removed when patient was awake with return of reflexes. Device was inspected for blood stains and any visible trauma to the lips, tongue, teeth or oral cavity of the patient was also noted.
Hence the parameters noted in each case were:
(1) Time taken for successful insertion of device was noted from removal of the face mask to obtaining the first square wave capnograph tracing.
(2) Any manipulation done such as pushing in or pulling out of the device to achieve effective ventilation.
(3) Number of attempts taken for successful insertion of the device.
(4) Reasons for failure of device insertion.
(5) Ease of gastric catheter insertion (without any aid) was graded as: Score 1: Easy if inserted in first attempt, Score 2: Difficult if inserted in second attempt, Score 3: Impossible if could not be inserted in second attempt.
(6) Oropharyngeal leak pressure.
(7) Anatomical alignment of device with the glottic opening was seen with a fibreoptic bronchoscope and graded as [13]: Score 1: full view of vocal cords, Score 2: part of vocal cords and or arytenoids seen, Score 3: only epiglottis seen, Score 4: no laryngeal structure visible (though ventilation was still possible).
(8) Intraoperative and postoperative adverse events such as desaturation (SpO2<92%), aspiration or regurgitation and airway obstruction or any visible trauma were noted.
(9) Postoperative pharyngolaryngeal morbidity such as sore throat, hoarseness and pain on swallowing were noted at one hour and 24 hours.
Sample size estimation: A study observed that the insertion times for the LMA-S™ were significantly shorter than for i-gel™ (34±12 s vs 42±23 s, p=0.024) [9]. Taking these values as reference, the minimum required sample size with 80% power of study and 5% level of significance is 87 patients in each study group. It was decided to take 90 patients in each group to keep in account any dropouts from the study.
Formula used for calculation of sample size:
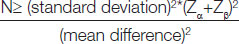
Where, Zα is value of Z at two sided alpha error of 5% and Zβ is value of Z at power of 80%.
Statistical Analysis
Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean±SD and median. Normality of data was tested by Kolmogorov-Smirnov test. If the normality was rejected, then non parametric test was used.
Quantitative variables were compared using Mann-Whitney Test (when the data sets were not normally distributed) between the two groups. Qualitative variables were compared using Chi-Square test/Fisher’s-exact test. A p-value of <0.05 was considered statistically significant. The data was entered in MS EXCEL spreadsheet and analysis was done using Statistical Package for Social Sciences (SPSS) version 21.0.
Results
Both the groups were comparable with respect to demographic profile of the patients [Table/Fig-3]. Both the groups were comparable with respect to the type of surgery (p-value=0.356), duration of surgical procedure (p-value=0.053) and size of the device used (p-value=0.541) [Table/Fig-3].
Demographic profile of the patients {Median(IQR)}
| Variables | i-GEL | LMA-Supreme | p-value |
|---|
| Age (Year) | 30 (24-42) | 31 (24-40) | 0.827** |
| Sex (M/F) | 24/66 | 26/64 | 0.739* |
| Weight (kg) | 54 (48-64) | 53 (45-62) | 0.277** |
| Height (cm) | 154 (150-160) | 155 (150-159) | 0.431** |
| BMI (kg/m2) | 22.92 (20.200-24.270) | 21.7 (19.65-24.79) | 0.130** |
| ASA(I/II) | 65/25 | 68/22 | 0.611* |
| Type of surgery (laparoscopic/non laparoscopic n, (%) | 74/16 (82.22/17.78) | 69/21 (76.67/23.33) | 0.356* |
| Duration of surgery (minutes) | 80 (75-90) | 88 (84-90) | 0.053** |
| Size of the device 3/4 n, (%) | 33/57 (36.67/63.33) | 37/53 (41.11/58.89) | 0.541* |
**Mann-Whitney U; *Chi-square test; LMA: Laryngeal mask airway supreme; M: Male; F: Female; p-value<0.05 considered statistically significant
There was no difference in the measured airway parameters and interincisor gap before and after application of extrication collar of patients in both the groups [Table/Fig-4].
Airway Parameters of the patients {Median(IQR)}
| S. No. | Variables | i-GEL | LMA-Supreme | p-value |
|---|
| 1. | Interincisor gap (cm) | 4.5 (4-5) | 4.5 (4.20-4.800) | 0.829** |
| 2. | Interincisor gap after extrication collar application (cm) | 2.2 (2.100-2.300) | 2.2 (2-2.300) | 0.061** |
| 3. | Thyromental distance (cm) | 7.3 (7.100-7.500) | 7.4 (7.100-7.500) | 0.963** |
| 4. | Upper lip bite test class (I/II/III) | 90/0/0 | 90/0/0 | - |
| 5. | Neck movement (N/R) n (%) | 90/0 (100/0) | 90/0 (100/0) | - |
| 6. | Mallampati class (I/II) n (%) | 37/53 (41.11/58.89) | 30/60 (33.33/67.67) | 0.280* |
**Mann-Whitney; *Chi-square test; LMA: Laryngeal mask airway supreme; p-value <0.05 considered statistically significant
The total time taken for successful insertion of SGD was significantly shorter with group i-gel as compared to group LMA supreme {median(IQR), 19(18.25-21) vs 24 (23-24) seconds respectively} with p-value ≤0.0001 [Table/Fig-5]. Overall success rate of insertion of i-gel was 96.67% (n=87) and that of LMA-S was 97.78% (n=88). The device was inserted successfully in first attempt in 91.11% (n=82) of patients in group i-gel and 93.33% (n=84) of patients in group LMA-S (p-value=0.781) [Table/Fig-5].
Performance characteristics of i-gel and LMA Supreme.
| S. No. | Performance | i-GEL | LMA- Supreme | p-value |
|---|
| 1. | Total time for successful insertion (secs) | <0.0001** |
| Mean±SD | 21.40±5.97 | 25.89±7 |
| Median (IQR) | 19 (18.25- 21) | 24 (23-24) |
| 2. | No. of attempts for device insertion | |
| 1 | 82 (91.11%) | 84 (93.33%) | 0.781* |
| 2 | 5 (5.56%) | 4 (4.44%) | 1*** |
| 3 | 0 | 0 | - |
| Failed Devices | 3 (3.33%) | 2 (2.22%) | 1*** |
| 3. | Oropharyngeal leak pressure (cm of water) | |
| Mean±SD | 26.98±6.01 | 26.15±4.74 | 0.555** |
| Median (IQR) | 26 (22-32) | 28 (22-30) |
| 4. | Gastric catheter insertion score | |
| 1 (Easy) | 87 (100%) | 88 (100%) | - |
| 2 (Difficult) | 0 | 0 | - |
| 3 (Impossible) | 0 | 0 | - |
| 5. | Fiberoptic bronchoscopic score | |
| 1 | 59 (67.82%) | 27 (30.68%) | <0.0001* |
| 2 | 27 (31.03%) | 55 (62.50%) | <0.0001* |
| 3 | 1 (1.15%) | 6 (6.82%) | 0.117*** |
| 4 | 0 | 0 | - |
| 6. | Blood stained device | 2 (2.30%) | 2 (2.27%) | 1*** |
| 7. | Postoperative complications | |
| Sore throat | 2 (2.30%) | 4 (4.54%) | 0.682*** |
| Hoarseness of voice | 0 | 0 | - |
| Difficulty in swallowing | 0 | 0 | - |
**Mann-Whitney U; *Chi-square test; ***Fischer-Exact test; LMA: Laryngeal mask airway supreme; p-value <0.05 considered statistically significant
Out of three device failures (all 3 attempts of insertion failed) for i-gel, the reason was ineffective ventilation due to air leak in one patient and insertion failure in two patients. In contrast, both the device failures for LMA-S were due to ineffective ventilation due to air leak. This difference was not statistically significant (p=1). Manipulations were required in six cases in each group to achieve effective ventilation. Changing the depth of the device (pushing in or pulling out) was the only manipulation done in this study.
The mean oropharyngeal leak pressure (cm of H2O) with the extrication collar in place in group i-gel was 26 (22-23) whereas in group LMA-S it was found out to be 28 (22-30) and the difference was statistically not significant (p-value=0.555). Gastric tube insertion score was 1 (easy) in 100% of the patients in both the groups. Fiberoptic grading of both the devices after insertion revealed i-gel has statistically significantly better anatomic alignment as compared to LMA-S (p-value≤0.0001) [Table/Fig-5]. The mean inspired and expired tidal volumes were found to be comparable between the groups (p-value=0.294 and 0.233 respectively). No intraoperative adverse events were found in either of the groups.
Blood staining of the supraglottic device, after removal, was observed in two patients in each of the groups. Sore throat was observed in two patients in group i-gel and in four patients in group LMA-S and it resolved within 24 hours.
Discussion
In this study, the efficacy of LMA Supreme and i-gel in 180 adult patients with simulated difficult airway undergoing elective surgery under general anaesthesia was compared. It was found that i-gel requires less time for successful insertion compared to LMA-S, but the variation in median time of insertion being approximately 5 seconds, may not be clinically relevant. The longer time with LMA supreme can be explained by the time required for its cuff to be inflated and pressure to be measured to 60 cm of H2O with a hand held manometer. In contrast, the i-gel is a noninflatable cuffed device that requires no such inflation. Both devices had high and comparable first attempt success rate of insertion {91.11% (n=82) with i-gel and 93.33% (n=84) with LMA-S insertion, p-value=0.781}. The anatomic alignment of i-gel with glottic opening was significantly better than that of LMA-S, but it did not translate into better leak and better ventilation as oropharyngeal leak pressures and inspiratory and expiratory tidal volumes were comparable between the two devices.
Theiler LG et al., did a crossover comparison of LMA-S and i-gel in simulated difficult airway scenario in 60 anaesthetised spontaneously breathing patients using an extrication collar to restrict head and neck mobility and to reduce mouth opening. In their findings, patients had interincisor gap of 4.7±0.7 cm without the collar, and 2.3±0.7 cm with the collar [9]. However, their study showed that LMA-S took less time for insertion as compared to igel (34±12 sec versus 42±23 sec) (p-value <0.024). The difference in results with this study could be because of many factors. The patients in that study were on spontaneous respiration and not paralysed. In this study, paralysis probably helped in easy insertion of the i-gel. It was also noticed that the number of male patients in their study was higher than those in this study {32 (53%) vs 50 (28.5%), respectively}. Weight of the patients in their study was 74±13 kg (mean±SD) which was much higher than that in this study (median weight 54.0 kg in i-gel group and 53.0 kg in LMA Supreme group, respectively). The use of larger size i-gel 5 in their patients, which has a bulkier cuff than sizes 3 and 4 used in this study could have also made insertion time longer with i-gel as compared to LMA-S [9].
Overall success rate of insertion was 96.67% (n=87) with i-gel and 97.78% (n=88) with LMA-S (p=0.996). Reasons for first attempt failure/device failure were either ineffective ventilation due to air leak or resistance encountered in advancing the device through pharynx during insertion and differences between the two groups were not statistically significant. No patient required an attempt of insertion to be aborted and mask ventilation to be done due to fall in SpO2 below 92%. The results are similar to the of study by Theiler LG et al., which showed that that the overall success rate of insertion for i-gel was 93% (n=56) and that for LMA-S was 95% (n=57) (p-value=0.18). They observed that inadequate ventilation due to airleak was the reason for all the three LMA-S failures while out of four i-gel failures, two were due to impossible insertion and the other two were due to inadequate ventilation [9].
Oropharyngeal leak pressure was comparable in the two groups. It is an important indicator of both the success of positive pressure ventilation and the degree of airway protection [14,15]. In this study, full view of the vocal cords (grade 1 view) was seen in 59 (67.82%) patients in i-gel group and 27 (30.68%) patients in LMA-S group. A better anatomic alignment with glottis was achieved with i-gel as compared to that with LMA-S. This can be explained by the fact that i-gel has an epiglottic rest to prevent epiglottic downfolding, thus revealing a clear view of the vocal cords but in LMA Supreme, the drainage tube is posterior to the ventilatory unit and traverses the cuff bowl in the midline dividing the cuff bowl into two equal parts and prevents clear view of glottis. No intraoperative and postoperative adverse events were reported in any patients in both the groups.
Limitation(s)
The results of this study should not be applied to patients with a difficult airway due to reasons other than those simulated in this study. Also, due to safety and ethical concerns difficult airway scenario was created by using a cervical collar and the use of both the devices in patients with actual difficult airway was not studied.
Conclusion(s)
Hence, this study suggests that both i-gel and LMA Supreme can be used effectively as rescue ventilatory devices in cannot intubate or ventilate scenarios in anaesthetised and paralysed patients when airway is difficult due to reduced mouth opening, limited subluxation of mandible and restricted neck mobility. Lastly, an excellent anatomic fit of i-gel suggests that it can be used as a conduit for inserting an endotracheal tube in difficult airway cases.
**Mann-Whitney U; *Chi-square test; LMA: Laryngeal mask airway supreme; M: Male; F: Female; p-value<0.05 considered statistically significant
**Mann-Whitney; *Chi-square test; LMA: Laryngeal mask airway supreme; p-value <0.05 considered statistically significant
**Mann-Whitney U; *Chi-square test; ***Fischer-Exact test; LMA: Laryngeal mask airway supreme; p-value <0.05 considered statistically significant